Introduction to Brachial Plexus Surgery
The network of nerves known as the Brachial Plexus runs from the spinal cord in the neck, through the shoulder region, into the arm, forearm and hand. It transmits motor commands and sensory signals for the upper limb.
When the brachial plexus is significantly injured-by trauma, stretching, avulsion, tumour or birth-related damage-its capacity to convey signals may be lost. In such cases, surgery may be required to restore nerve continuity, relieve compression, repair or transfer nerves, or in extreme cases perform muscle/tendon transfers.
The purpose of brachial plexus surgery is therefore twofold: to relieve pain and/or restore function (movement, strength, sensation) in the shoulder, arm and hand.
Because the time window, severity of injury and the patient's condition all influence outcome, brachial plexus surgery is a highly specialized field, typically involving microsurgical techniques, nerve grafting, nerve transfers and rehabilitation.
In this article we will explore the causes & risks, signs & symptoms, diagnosis, treatment options (including surgery), prevention/management, possible complications and living with the condition after surgery.
Causes and Risk of Brachial Plexus Injury (leading to need for surgery)
Brachial plexus injury occurs when the network of nerves that sends signals from the spine to the shoulder, arm, and hand is stretched, compressed, or torn. These nerves control movement and sensation, so severe damage can lead to significant weakness, numbness, or paralysis that may require surgical repair.
Causes
Some of the common causes of brachial plexus injuries are:
-
High-energy trauma: For example motor-vehicle accidents (especially motorcycle crashes), falls, gunshot wounds, or other injuries that forcibly stretch or tear the upper limb/skull/neck region.
-
Sports injuries: Contact sports (football, rugby) or other situations where the shoulder is forced down and the head/neck is forced in the opposite direction-this traction injures the plexus.
-
Birth injuries (obstetric brachial plexus palsy): During difficult deliveries, lateral traction on the infant's head/shoulder, shoulder dystocia, breech deliveries, large birth weight infants-all increase risk of injury to the brachial plexus in newborns.
-
Tumours, radiation or compression: A tumour growing in or near the brachial plexus, or fibrosis from radiation therapy, may compress or damage the nerve network.
-
Iatrogenic (medical) injury: During neck, shoulder or chest surgery, nerve roots of the brachial plexus may be inadvertently injured.
Risk factors
-
Participation in high-impact contact sports or motor vehicle riding.
-
For infants: high birth weight, prolonged labour, breech presentation, shoulder dystocia.
-
Delay in diagnosis and treatment: The longer the nerve remains damaged, the greater the risk of irreversible muscle atrophy and poor outcome.
-
Age may influence prognosis: Younger patients tend to have better outcomes.
This section highlights why early recognition, referral and management are so important.
Symptoms and Signs of Brachial Plexus Injury
Brachial plexus injury symptoms vary greatly depending on which nerves are damaged, how severely they are stretched or torn, and where along the nerve pathway the lesion occurs. These symptoms can affect motor control, sensation, and pain levels in the shoulder, arm, hand, and sometimes the neck on one side of the body.
Mild injuries
-
A sudden burning or stinging "electric shock" sensation down the arm (often called a "stinger" or "burner" in athletes).
-
Temporary numbness, tingling or weakness in the arm or hand lasting seconds to minutes (or longer).
More severe injuries
-
Persistent or worsening weakness or inability to use certain muscles of the shoulder, arm, wrist or hand.
-
Loss of sensation (numbness) in parts of the arm, hand or fingers.
-
Severe pain, often neuropathic in nature (burning, shooting, deep aching) in the shoulder/arm region.
-
A limp or floppy arm ("arm hangs limply") in the most extreme cases where nerve roots are avulsed (torn) from the cord.
When to suspect serious injury
If you have weakness or loss of motion in the arm/hand, numbness, persistent pain, or symptoms in both arms - you should seek urgent evaluation.
In your blog, you may wish to emphasise that early referral to a specialist is key, because time-to-surgery matters for optimal outcome.
Diagnosis of Brachial Plexus Injury
Diagnosing a brachial plexus injury requires combining physical examination findings with detailed imaging and electrodiagnostic tests to determine the type, location, and extent of nerve damage. Early and accurate diagnosis is critical to guide treatment decisions and determine whether surgery is needed.
Clinical assessment
-
Detailed history: mechanism of injury (trauma, birth, sports, tumour), timing, progression of symptoms, previous treatments, presence of other injuries.
-
Physical examination: assessment of motor strength (shoulder, elbow, wrist, fingers), sensory testing (light touch, pin-prick), reflexes, muscle wasting/atrophy, special signs (e.g., shoulder droop, scapular winging).
Imaging and electrophysiology
-
X-ray: to check associated fractures, dislocations or bony anomalies near the plexus.
-
MRI / CT scan: detailed imaging of soft tissue, nerve roots, tumour/compression, and to assess nerve avulsion or continuity.
-
Electromyography (EMG) and nerve conduction studies (NCS): to evaluate nerve function, degree of denervation, and to monitor recovery over time.
Timing matters
Because nerves regenerate slowly and muscle changes (atrophy) may set in, it
is crucial to monitor progression. If no recovery is seen over 3-6 months,
surgical intervention is often recommended.
Thus, the diagnostic pathway must be handled by a multidisciplinary team
involving neurology, neurosurgery/orthopaedic, hand surgery, physical
therapy and rehabilitation.
Treatment Options of Brachial Plexus Injury / Surgery
Treatment for brachial plexus injury depends on the cause, extent, and severity of the nerve damage. Mild injuries may recover with conservative management, while severe nerve ruptures or avulsions typically require surgery. Surgical intervention is most effective when performed within 3-6 months of injury to prevent irreversible muscle atrophy and nerve degeneration.
Non-surgical (conservative) management
-
In mild injuries (nerve stretch/compression but not rupture), symptoms may improve without surgery over weeks to months.
-
Physical therapy / occupational therapy: to maintain joint mobility, prevent contractures and muscle atrophy while waiting for nerve recovery.
-
Splints or braces: for hand/arm protection when sensation is reduced, to prevent secondary injury.
-
Pain management: neuropathic pain may require medications (anticonvulsants, antidepressants, nerve pain modulators), and specialist pain services.
Surgical interventions
When nerve injury is severe, surgery is often indicated. The success of surgery depends greatly on timing (earlier is better) and the type of injury.
Timing
-
Some injuries (penetrating, open wounds, vascular involvement) may require urgent surgery (within first 1-2 weeks).
-
For other traumatic plexus injuries, many experts suggest surgery within 3 to 6 months if there is no clinical/EMG sign of recovery. Delays beyond 9-12 months result in significantly worse outcomes due to muscle atrophy and denervation.
Surgical techniques
Depending on the nature of the nerve damage, surgeons may use one or more of the following approaches:
-
Nerve repair / primary neurorrhaphy: If a nerve is cleanly cut, the two ends may be sewn together under microscope.
-
Neurolysis / decompression: When the nerve is intact but compressed or encased in scar tissue, freeing it up (removing adhesions) may help recovery.
-
Nerve grafting: When a segment of nerve is lost/damaged, a graft (from e.g., the sural nerve) can bridge the gap and allow regrowth.
-
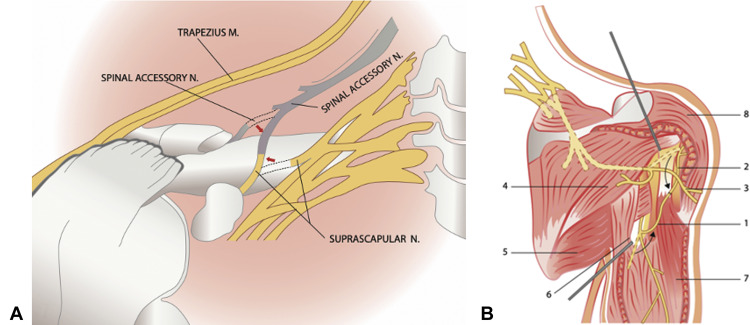
Nerve transfer (neurotization): A healthy nearby donor nerve is connected to the injured distal nerve to supply function earlier; this can shorten regeneration distance and improve outcomes.
-
Tendon or muscle transfer: In cases where nerve repair is no longer feasible (delayed cases, irreversible muscle atrophy), functioning tendons/muscles are moved to restore key functions (e.g., elbow flexion, hand grip).
-
Free functional muscle transplantation: Transplanting a muscle (with its nerve and blood supply) from another part of the body (e.g., thigh) into the arm to restore function when original muscle is nonviable.
Post-operative rehabilitation
-
After surgery, intensive physical and occupational therapy is essential. Regenerating nerves grow slowly (1-3 mm/day) and functional improvement may take many months to years.
-
Maintaining joint mobility, preventing contractures, proper positioning of limb, and monitoring muscle function are critical.
Prognosis
-
Outcomes depend on factors such as age, type and level of injury (root avulsion worse than stretch), timing of surgery, surgical technique used, and rehabilitation compliance.
-
Even with optimal management, full recovery may not be possible-residual weakness, numbness or disability may remain.
For your page:
You may want to provide a table or bullet list of surgical options, plus a "when is surgery indicated" box (e.g., no improvement after 3-6 months, root avulsion, open wound, vascular injury, etc.)
Prevention and Management of Brachial Plexus Injury / Post-Surgical Care
Prevention and management of brachial plexus injury, along with proper post-surgical care, are essential to protect nerve function, promote recovery, and prevent secondary complications. These strategies involve a combination of physical therapy, correct positioning, patient education, and long-term rehabilitation under medical supervision.
Prevention
-
While some causes (severe trauma) cannot be entirely prevented, risk reduction is possible:
-
In contact sports, use proper protective equipment, coach supervision, and safe techniques to avoid high-risk neck/shoulder strains.
-
For birth injuries: managing shoulder dystocia, breech deliveries, appropriate obstetric care can minimise risk to brachial plexus in newborns.
-
Minimising iatrogenic nerve injury by ensuring careful surgical positioning, avoiding undue traction on the shoulder/neck.
-
Early management / non-surgical care
-
For suspected injury, prompt evaluation by specialist centres (nerve/hand surgeons) is important. Delay can compromise outcome.
-
During the waiting period (perhaps before surgery) focus on:
-
Keeping joints mobile (passive and active range of motion exercises) to avoid stiffness.
-
Protecting the limb from injury if sensation is impaired (e.g., using splints, padding).
-
Pain control and psychological support (nerve injury and persistent weakness cause distress).
-
Post-surgical management
-
Clear rehabilitation plan: early gentle mobilization, progression as per surgeon/therapist instructions.
-
Monitoring for signs of complications (infection, wound issues, graft failure) and for evidence of nerve recovery (electrophysiology, clinical exam).
-
Long-term functional adaptation: Even with partial recovery, patients may need to adapt their lifestyle, use assistive devices, and modify activities.
Patient education
-
Inform patients about the long duration of recovery (months to years). Encourage compliance with physiotherapy.
-
Explain realistic outcome expectations: full pre-injury function may not always be achieved, but meaningful improvement is possible.
-
Emphasise avoidance of further injuries, protecting the limb, ergonomics in daily life and occupation.
Complications of Brachial Plexus Injury & Surgery
Complications of brachial plexus injury and surgery vary from mild loss of sensation to permanent paralysis or chronic pain, depending on the location, type, and severity of the nerve damage. Even with surgical repair, nerve regrowth and functional recovery are often slow and incomplete, requiring long-term follow-up and rehabilitation.
From the injury itself
-
Permanent muscle weakness, paralysis or atrophy if nerve supply is lost and not restored in time.
-
Loss of sensation, which increases risk of injuries (burns, cuts, unnoticed trauma).
-
Joint stiffness, contractures, frozen shoulder/elbow due to immobility.
-
Chronic neuropathic pain: burning, shooting, electric-shock type pain.
From surgery
-
General surgical risks: infection, bleeding, anaesthesia complications.
-
Specific to nerve surgery: donor-nerve morbidity (in nerve graft/transfer), incomplete or failed nerve regeneration, neuroma formation (painful nerve scar).
-
Delayed or inadequate functional recovery: even after technically successful surgery, muscle and nerve regeneration may lag or be insufficient.
-
Need for additional procedures (tendon/muscle transfer) if nerve repair alone is insufficient.
Impact on life
-
Permanent disability may lead to reduced quality of life, psychosocial issues, occupational limitations.
-
In paediatric cases (birth injuries) the long-term impact on growth, shoulder/arm development may pose challenges.
Your blog may include a "red-flag" box: if you notice increasing pain, sudden loss of function, signs of infection post-surgery-seek medical attention promptly.
Living with the Condition (Post-Surgery and Long-Term Outlook)
Living after a brachial plexus injury-especially post-surgery-requires long-term physical, emotional, and functional adaptation. Full recovery often takes months to years, depending on how severe the injury was and how quickly nerves regenerate. Ongoing physiotherapy, pain management, and psychological support form the foundation for maintaining an independent and fulfilling life.
Rehabilitation journey
-
After surgery, nerve regrowth is slow. Patients and families must understand that recovery may continue for up to 2-3 years (or more) and progress may be gradual.
-
Consistent physical/occupational therapy is essential for maximizing outcome: improving strength, control, range of motion, and adapting to residual deficits.
-
Use of compensatory strategies: assistive devices, adaptive tools for daily activities (dressing, feeding, writing, using a computer).
Psychological & social aspects
-
Dealing with chronic pain, partial disability or changed function can impact mental health: anxiety, depression, frustration. Including psychological support and counselling may be beneficial.
-
Occupational adjustments: depending on job (manual labour vs desk work) some patients may need retraining or job modification.
Long-term monitoring
-
Periodic assessment of nerve/muscle recovery; monitoring for joint stiffness, pain flare-ups, secondary injuries (due to numbness).
-
Maintenance exercises, stretching, strengthening as advised by therapist to sustain gains and prevent deterioration.
Quality of life and realistic expectations
-
It is important to set realistic goals: complete restoration to pre-injury status may not always be possible, but meaningful improvements in function and pain reduction often are.
-
Many patients achieve independence in most activities of daily living, even if full strength is not restored. Emphasise success stories (if available) and keep hope alive while being realistic.
Tips for patients
-
Protect the limb: especially if sensation is reduced - avoid burns, sharp objects, extreme temperatures.
-
Maintain joint mobility: even when nerve recovery is ongoing.
-
Stay active in therapy and follow-ups.
-
Seek support networks: patient groups, online forums, peer mentoring.
-
Adopt healthy lifestyle: good nutrition, avoid smoking (which impairs nerve/muscle healing), manage comorbidities (diabetes, vascular disease) which may impact nerve recovery.
Top 10 Frequently Asked Questions about Brachial Plexus Surgery
1. What Is the Brachial Plexus and Why Is It So Important?
The brachial plexus is a complex network of nerves that originates from the spinal cord in the neck (from C5 to T1 nerve roots). These nerves branch out to control the muscles and sensations of the shoulder, arm, forearm, and hand.
When these nerves are stretched, compressed, or torn, the result can be severe functional loss - ranging from weakness and tingling to total paralysis of the upper limb. Injuries to the brachial plexus are often seen in motorcycle or car accidents, sports trauma, falls, or birth injuries (Erb's palsy) in newborns.
Without proper treatment, the muscles controlled by these nerves may atrophy, making timely surgical intervention essential.
2. What Exactly Is Brachial Plexus Surgery?
Brachial Plexus Surgery is a highly specialized procedure performed to restore movement and sensation in an arm affected by nerve injury.
Depending on the nature and extent of the injury, the surgeon may perform:
-
Nerve Grafts: Damaged nerve sections are removed and replaced with healthy nerve segments (often from the leg's sural nerve).
-
Nerve Transfers: A nearby functioning nerve that performs a less critical function is connected to the injured nerve to restore essential muscle function (e.g., transferring a chest nerve to the biceps nerve).
-
Tendon or Muscle Transfers: If nerve repair alone is not possible, healthy muscles from another part of the body (like the thigh or chest) are transplanted to restore movement.
The choice of technique depends on how old the injury is, where the nerve is damaged, and the patient's age and overall health.
3. Who Is a Good Candidate for Brachial Plexus Surgery?
Candidates for brachial plexus surgery typically include individuals who have:
-
Severe nerve damage with persistent weakness or paralysis lasting over 3-6 months.
-
No spontaneous nerve recovery seen on physical examination or nerve conduction tests.
-
Post-traumatic injuries due to accidents or sports.
-
Birth-related nerve injuries that do not improve with conservative management (in infants).
Before recommending surgery, doctors perform MRI, CT Myelography, and Electromyography (EMG) to assess nerve continuity and function.
4. How Soon Should Brachial Plexus Surgery Be Done After Injury?
Timing is crucial. The best outcomes are achieved when surgery is performed within 3 to 6 months after injury.
Delaying beyond a year can reduce success rates because muscles lose their ability to respond to regenerated nerves. However, certain cases (like late referrals or partial injuries) may still benefit from reconstructive procedures such as tendon or muscle transfers.
In infants with obstetric brachial plexus palsy, surgery is often considered between 3 and 9 months of age if there's no significant spontaneous improvement.
5. What Happens During the Surgery?
Brachial plexus surgery is performed under general anesthesia and can take anywhere from 4 to 12 hours, depending on the complexity.
The key steps may include:
-
Identification of injured nerves using microscopic visualization.
-
Removal of scar tissue or damaged segments.
-
Reconstruction using nerve grafts or transfers.
-
Microsurgical suturing of nerves using fine instruments under a high-powered microscope.
The surgery may involve the neck, shoulder, or even leg (for harvesting grafts). Patients usually stay in the hospital for several days for observation and initial rehabilitation guidance.
6. What Is the Recovery Process Like After Brachial Plexus Surgery?
Recovery is gradual and requires patience and dedication.
-
Initial Recovery (0-6 Weeks): The arm is usually supported in a sling or brace. Pain and swelling are managed with medication.
-
Rehabilitation Phase (6 Weeks-12 Months): Physiotherapy starts early to maintain joint flexibility and prevent stiffness. Electrical stimulation and gentle exercises help stimulate nerve regeneration.
-
Nerve Regrowth: Nerves grow slowly - about 1 millimeter per day, so noticeable muscle contractions may take 6 to 12 months to appear.
-
Long-term Recovery (1-3 Years): Continued therapy and monitoring ensure steady improvement. Some patients regain partial but functional movement, while others achieve near-complete recovery.
7. What Are the Risks or Possible Complications of Brachial Plexus Surgery?
Like any complex microsurgery, brachial plexus surgery carries some risks, including:
-
Infection or bleeding at the surgical site.
-
Scar formation or neuroma (painful nerve scar).
-
Persistent weakness or incomplete recovery.
-
Nerve pain or altered sensations.
-
Anesthesia-related complications.
However, with modern microsurgical techniques and postoperative rehabilitation, complication rates are relatively low. Choosing an experienced neurosurgeon or peripheral nerve specialist significantly improves success rates.
8. What Results Can Be Expected After Surgery?
Results vary depending on factors like age, time since injury, and injury severity.
-
Patients with early surgical intervention often regain strong shoulder and elbow movement.
-
Hand and finger movement recovery can be more limited, especially in complete avulsion injuries.
-
In cases where nerves cannot be repaired, muscle or tendon transfers can still restore partial but functional movement.
With dedicated physiotherapy, 70-90% of patients report meaningful functional improvement, such as the ability to lift the arm, bend the elbow, or grip light objects.
9. What Role Does Physiotherapy Play After Surgery?
Physiotherapy is the cornerstone of recovery. It helps retrain muscles, maintain flexibility, and prevent contractures.
A typical rehabilitation plan includes:
-
Range of motion exercises to prevent stiffness.
-
Strengthening routines once nerve signals start reaching the muscles.
-
Mirror therapy and occupational training to enhance muscle control.
-
Electrical stimulation to support nerve regeneration.
Rehabilitation may last 12 to 24 months, and consistent therapy is often the deciding factor between partial and full recovery.
10. What Is the Cost and Insurance Coverage for Brachial Plexus Surgery?
The cost of Brachial Plexus Surgery depends on:
-
The complexity of the injury and type of reconstruction needed.
-
Hospital and surgeon fees.
-
Duration of hospital stay and physiotherapy sessions.
In India, for example, the cost typically ranges from ₹2,00,000 to ₹8,00,000 (USD $2,500-$10,000). In the U.S. and Europe, costs can range from $20,000 to $100,000 depending on the case.
Many insurance providers and government health schemes cover this surgery if it is medically necessary (for trauma-related or birth injuries). Cosmetic or elective nerve surgeries may not be covered. Always check with your insurance company for exact coverage details.


