Source: neurologyadvisor.com
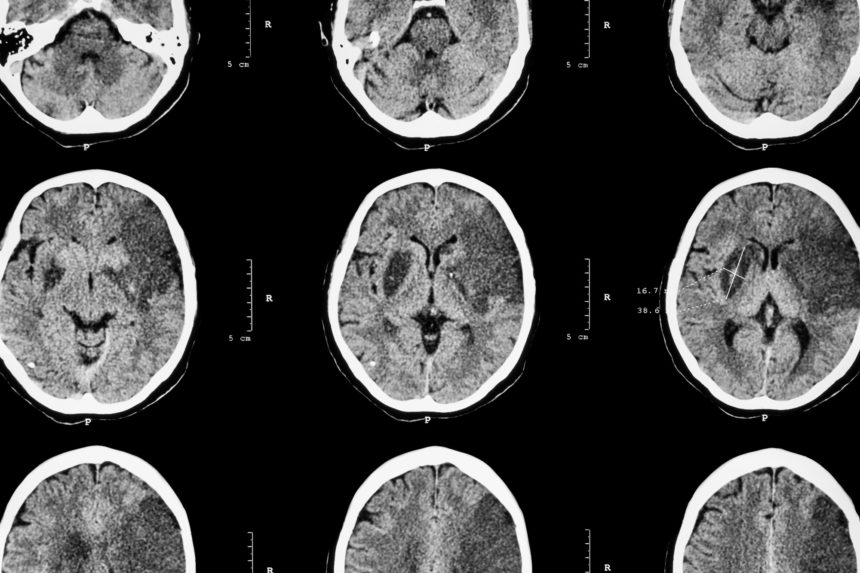
Migraine headache, particularly migraine with aura, is associated with increased risk for cardiovascular disease and cerebrovascular events, including ischemic stroke. In light of the high prevalence of migraine headache, this association should be further investigated, according to a review published in the Journal of the American Heart Association.
Other than the characteristic headache, migraine may be associated with transient focal neurology symptoms (eg, aura) that usually persist for less than an hour. There is a wide inter-individual and intra-individual variability in the frequency of migraine attacks. Migraine is most common in women aged 25 to 55 years, and the prevalence decreases after the fifth decade of life.
There are several possible mechanisms for the increased risk for cardiovascular and cerebrovascular disease in patients with migraine, including higher prevalence of hypertension and hyperlipidemia, generalized endothelial dysfunction and increased platelet aggregation, higher prevalence of patent foramen ovale (PFO), and the effect of medications used to treat these patients.
Previous studies have reported gender differences in migraine characteristics, as the disease is more prevalent and frequently more severe in women. It is believed that fluctuations in hormone levels, particularly estrogen, may be responsible for these gender differences.
Many studies have reported an association between migraine and cardiovascular and cerebrovascular disease, with a more robust association in cases of migraine with aura. There are data associating migraine with aura with an increased risk for ischemic stroke, myocardial infarction, cardiovascular mortality, as well as venous thromboembolism and peripheral artery disease.
As noted, PFO may be more common in patients with migraine. Several studies have suggested that closure of PFO may be beneficial and reduce migraine attack frequency. However, as this was not the primary outcome of the studies, routine PFO closure for migraine should not be recommended at this point.
While there are many studies reporting an association between migraine and cardiovascular and cerebrovascular events, the rate of events in all these studies was low. On the other hand, due to the high prevalence of migraine worldwide, this still translates into a substantial increase in population risk.
At this point, there are no established recommendations aimed at reducing cardiovascular risk in patients with migraine. Evidence of potential benefit of anti-platelet, beta-blocker, and statin therapy in patients with migraine are lacking. Moreover, limited data are available on the effect of controlling migraine symptoms on cardiovascular events.
While triptans have not been shown to increase cardiovascular risk in patients with migraine, nonsteroidal anti-inflammatory drugs use should be limited to acute migraine episodes, as chronic use may be associated with increased cardiovascular risk.
Patients with migraine should be counseled about a healthy lifestyle, including regular physical activity, smoking cessation, blood pressure control, and weight loss.
“To date, there has been no established therapy to lower cardiovascular risk among women with migraine. Physicians should inquire about migraine history when assessing the cardiovascular risk of women,” concluded the researchers.