2. Introduction
Mpox, commonly known as Monkeypox, is a zoonotic viral disease caused by the Monkeypox virus, a member of the Orthopoxvirus genus. The disease is endemic in parts of Central and West Africa but has seen sporadic outbreaks in non-endemic regions, raising global health concerns. This guide aims to provide detailed information about Mpox, covering its transmission, symptoms, diagnosis, treatment, and prevention. The guide is intended for both healthcare professionals and the general public to enhance understanding and foster effective management of the disease.
3. What is Mpox?
Mpox is a viral illness with symptoms similar to those of smallpox, though generally less severe. The disease was first discovered in monkeys in 1958, and the first human case was recorded in 1970 in the Democratic Republic of Congo. The virus is classified into two genetic clades:
- Central African (Congo Basin) Clade: More virulent and transmissible, often associated with higher mortality.
- West African Clade: Less severe with a lower case-fatality rate.
Table: Comparison of Mpox Clades
| Feature | Central African Clade | West African Clade |
|---|---|---|
| Geographic Location | Central Africa (Congo Basin) | West Africa |
| Virulence | High | Moderate |
| Transmission | Human-to-human transmission higher | Lower human-to-human transmission |
| Mortality Rate | Higher (up to 10%) | Lower (1-3%) |
4. Transmission
Mpox is primarily transmitted from animals to humans through direct contact with blood, bodily fluids, or cutaneous/mucosal lesions of infected animals. Human-to-human transmission can occur through respiratory droplets, close contact with an infected person, or contact with contaminated materials like bedding.
Transmission Routes:
- Animal-to-Human Transmission:
- Direct contact with infected animals (e.g., rodents, monkeys).
- Consumption of undercooked meat from infected animals.
- Human-to-Human Transmission:
- Respiratory droplets during prolonged face-to-face contact.
- Direct contact with body fluids or lesions.
- Indirect contact via contaminated objects.

Table: Risk Factors for Mpox Transmission
| Risk Factor | Description |
|---|---|
| Contact with Infected Animals | Handling, bites, or scratches from infected animals. |
| Close Contact with Infected Persons | Household members, healthcare workers, caregivers. |
| Consumption of Bushmeat | Eating undercooked meat from infected animals. |
| Lack of Protective Measures | Absence of PPE for healthcare workers, inadequate hygiene. |
5. Symptoms
The incubation period for Mpox is generally 6-13 days but can range from 5-21 days. The disease typically progresses through several stages, starting with an initial set of symptoms that are followed by the development of a characteristic rash.
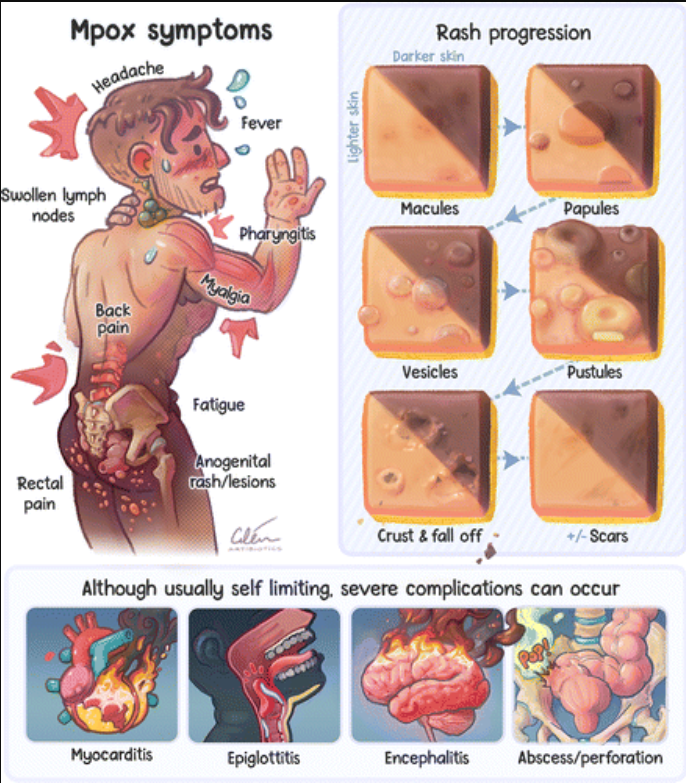
Initial Symptoms:
- Fever
- Intense headache
- Muscle aches (myalgia)
- Back pain
- Low energy (fatigue)
- Swollen lymph nodes (lymphadenopathy)
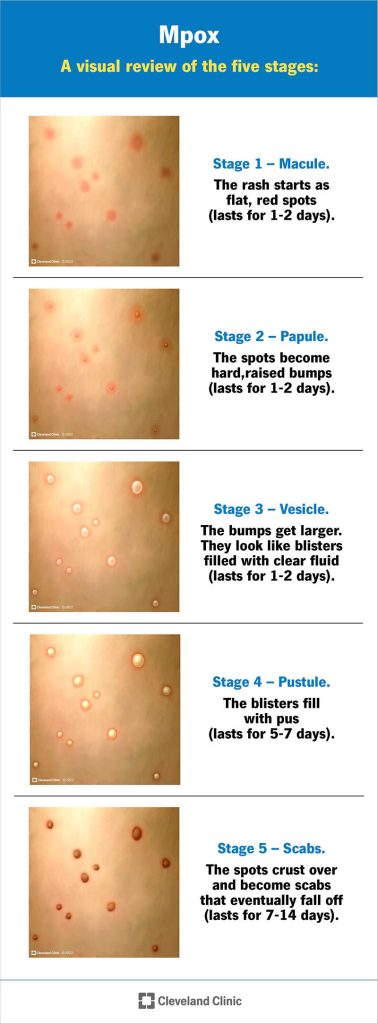
Rash Progression:
The rash usually begins on the face and then spreads to other parts of the body, including the palms, soles, and mucous membranes. It goes through the following stages:
- Macules: Flat, red spots.
- Papules: Raised, hard bumps.
- Vesicles: Small, fluid-filled blisters.
- Pustules: Pus-filled lesions.
- Scabs: Lesions crust over and eventually fall off.
Table: Stages of Mpox Rash Development

| Stage | Description | Duration |
|---|---|---|
| Macules | Flat, discolored spots on the skin. | 1-2 days |
| Papules | Raised, firm bumps. | 1-2 days |
| Vesicles | Fluid-filled blisters. | 1-2 days |
| Pustules | Pus-filled lesions; can be painful. | 5-7 days |
| Scabs | Lesions crust over; scabs eventually fall off. | 1-2 weeks |
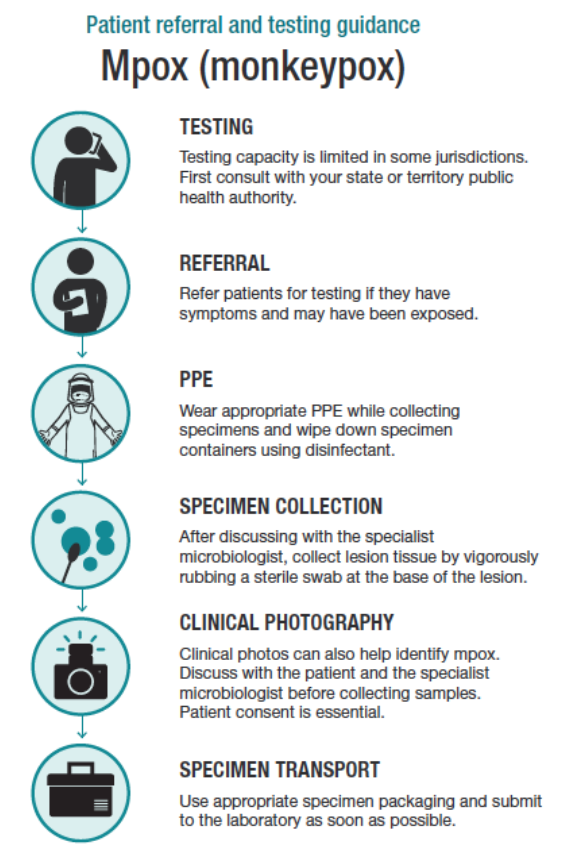
6. Diagnosis
Diagnosing Mpox involves a combination of clinical examination, patient history, and laboratory testing. Due to its similarity to other pox-like diseases, laboratory confirmation is essential.

Diagnostic Methods:
- Clinical Examination: Assessment of symptoms, especially the characteristic rash.
- Laboratory Testing:
- PCR (Polymerase Chain Reaction): The most reliable method, using samples from skin lesions, blood, or respiratory specimens.
- Electron Microscopy: Identifies the virus particles in samples.
- Serology: Detects antibodies, though less commonly used for acute diagnosis.
Table: Diagnostic Criteria for Mpox
| Criterion | Method | Importance |
|---|---|---|
| Symptom Assessment | Clinical examination | Initial identification based on symptoms. |
| PCR Testing | Laboratory analysis of lesions or blood | Confirms presence of Monkeypox virus. |
| Electron Microscopy | Visualization of virus particles | Provides visual confirmation, usually in research settings. |
| Serology | Detection of antibodies in blood | Useful for retrospective diagnosis, not acute cases. |
7. Treatment
There is no specific treatment approved for Mpox; however, certain antivirals developed for smallpox may be effective. Treatment primarily focuses on symptom management and supportive care.
Available Treatments:
- Symptomatic Treatment:
- Fever reducers (e.g., paracetamol).
- Pain management (e.g., ibuprofen).
- Hydration support (oral or intravenous fluids).
- Antiviral Treatment:
- Tecovirimat (ST-246): An antiviral drug approved for smallpox, showing efficacy in treating Mpox.
- Cidofovir and Brincidofovir: Other antivirals used off-label for severe cases.
Supportive Care:
- Isolation of the patient to prevent transmission.
- Monitoring for complications (e.g., secondary bacterial infections).
- Nutritional support during recovery.
Table: Mpox Treatment Options
| Treatment Type | Example | Indication |
|---|---|---|
| Symptomatic Treatment | Paracetamol, Ibuprofen | Reducing fever and managing pain. |
| Antiviral Treatment | Tecovirimat, Cidofovir | Used in severe or high-risk cases. |
| Supportive Care | Hydration, Isolation | Ensuring recovery and preventing spread. |
8. Prevention
Prevention strategies for Mpox focus on reducing exposure to the virus through both vaccination and non-pharmaceutical measures.
Preventative Measures:
- Vaccination:
- Smallpox Vaccine: Provides cross-protection against Mpox.
- JYNNEOS Vaccine: Specifically approved for both smallpox and Mpox, recommended for high-risk groups.
- Hygiene Practices:
- Regular hand washing with soap and water.
- Use of alcohol-based hand sanitizers.
- Avoiding Contact:
- Avoiding close contact with infected individuals and animals.
- Safe handling of animals and animal products in endemic areas.
- Protective Equipment:
- Use of Personal Protective Equipment (PPE) by healthcare workers.
- Ensuring proper sterilization of medical instruments and environments.
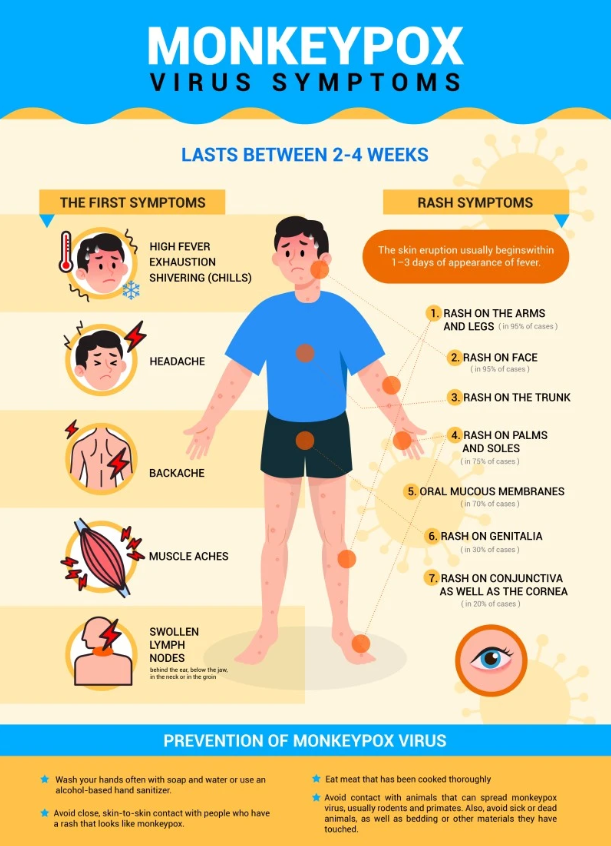
Table: Mpox Prevention Strategies
| Prevention Method | Description | Target Group |
|---|---|---|
| Vaccination | JYNNEOS and Smallpox vaccine | High-risk individuals, healthcare workers. |
| Hygiene Practices | Handwashing, use of sanitizers | General public, especially in endemic areas. |
| Avoiding Contact | Minimizing interaction with infected animals/people | General public, travelers to endemic regions. |
| Protective Equipment | PPE for healthcare workers, sterilization | Healthcare workers, laboratory personnel. |
9. Complications
Mpox can lead to a variety of complications, particularly in vulnerable populations such as children, pregnant women, and immunocompromised individuals.
Potential Complications:
- Secondary Bacterial Infections: Can occur if skin lesions become infected.
- Bronchopneumonia: Inflammation of the lungs due to the virus or secondary infection.
- Sepsis: A severe response to infection leading to systemic inflammation.
- Encephalitis: Inflammation of the brain, which can lead to neurological complications.
- Corneal Infection: Can result in scarring and potentially vision loss.
Table: Common Complications of Mpox
| Complication | Description | Risk Group |
|---|---|---|
| Secondary Infections | Bacterial infection of skin lesions | All, especially those with poor hygiene. |
| Bronchopneumonia | Lung inflammation | Children, elderly, immunocompromised. |
| Sepsis | Body-wide infection response | Severe cases, immunocompromised. |
| Encephalitis | Brain inflammation | Children, severe cases. |
| Corneal Infection | Eye infection leading to vision loss | Severe cases, lack of early treatment. |
10. Public Health Guidelines
Public health guidelines for Mpox aim to prevent and control outbreaks, minimize transmission, and provide appropriate care for infected individuals.
Key Guidelines:
- Isolation: Infected individuals should be isolated until all lesions have healed.
- Contact Tracing: Identifying and monitoring contacts of confirmed cases to prevent further spread.
- Reporting: Healthcare providers must report suspected or confirmed cases to public health authorities immediately.
- Vaccination Campaigns: In areas with outbreaks, vaccination of at-risk populations is crucial.
- Education and Awareness: Public health campaigns to inform the public about symptoms, transmission, and prevention of Mpox.
Table: Public Health Measures for Mpox Control
| Measure | Description | Implementation |
|---|---|---|
| Isolation | Separation of infected individuals | Healthcare settings, home isolation. |
| Contact Tracing | Identifying and monitoring exposed individuals | Public health departments. |
| Reporting | Mandatory reporting of cases to health authorities | Healthcare providers. |
| Vaccination | Targeted vaccination of high-risk populations | Local and national health agencies. |
| Public Education | Awareness campaigns on symptoms and prevention | Government, NGOs, healthcare facilities. |
11. Vaccination
Vaccination is a critical tool in preventing Mpox, particularly in high-risk populations and during outbreaks.
Available Vaccines:
- Smallpox Vaccine: Historically used to eradicate smallpox, it also provides protection against Mpox due to the related nature of the viruses.
- JYNNEOS Vaccine: A newer, non-replicating vaccine specifically approved for use against both smallpox and Mpox. It is recommended for individuals at high risk, such as healthcare workers, laboratory personnel, and those exposed to confirmed cases.
Vaccination Strategies:
- Pre-Exposure Prophylaxis (PrEP): Vaccination of individuals at high risk before they are exposed to the virus.
- Post-Exposure Prophylaxis (PEP): Vaccination within four days of exposure to prevent the onset of disease; vaccination up to 14 days after exposure may reduce the severity of symptoms.
Table: Mpox Vaccination Overview
| Vaccine Name | Type | Target Population | Efficacy |
|---|---|---|---|
| Smallpox Vaccine | Live, replicating | General public, at-risk groups | High, also effective against Mpox |
| JYNNEOS Vaccine | Live, non-replicating | High-risk populations (healthcare workers, contacts) | High, specifically designed for Mpox |
12. Mpox in Specific Populations
Mpox can present differently and have more severe consequences in certain populations, including children, pregnant women, and immunocompromised individuals.
Mpox in Children:
- Symptoms: Similar to adults but with a higher risk of severe disease and complications.
- Complications: Higher likelihood of secondary bacterial infections, pneumonia, and encephalitis.
Mpox in Pregnant Women:
- Risks: Potential for vertical transmission to the fetus, leading to congenital Mpox, stillbirth, or preterm birth.
- Management: Close monitoring, supportive care, and early antiviral treatment if necessary.
Mpox in Immunocompromised Individuals:
- Severity: Greater risk of prolonged and severe illness, with higher chances of complications such as sepsis and encephalitis.
- Treatment: More aggressive antiviral treatment and supportive care may be required.
Table: Mpox Impact on Specific Populations
| Population | Risks/Complications | Recommended Actions |
|---|---|---|
| Children | Severe disease, secondary infections | Early diagnosis, supportive care, vaccination. |
| Pregnant Women | Vertical transmission, pregnancy complications | Close monitoring, antiviral treatment. |
| Immunocompromised | Prolonged/severe illness, complications | Aggressive treatment, isolation, vaccination. |
13. Myths and Facts
Given the recent rise in Mpox cases, misinformation has spread. It is crucial to address these myths to ensure the public receives accurate information.
Common Myths and Facts:
| Myth | Fact |
|---|---|
| Mpox is a new disease | Mpox was first identified in humans in 1970. |
| Mpox only affects people in Africa | Cases have been reported globally, including in non-endemic regions. |
| Mpox is always fatal | The majority of cases are mild and recover without treatment. |
| Vaccination is not necessary | Vaccination is a key preventive measure, especially for high-risk groups. |
| Mpox can be transmitted through the air | Transmission occurs primarily through direct contact with bodily fluids or lesions, not airborne spread. |
14. Resources and Support
Access to accurate information and support is essential for managing Mpox effectively. Below are some key resources and support networks.
Resources:
- World Health Organization (WHO): Mpox Information
- Centers for Disease Control and Prevention (CDC): Mpox Resources
- National Health Services (NHS): Mpox Guidance
- Local Health Departments: Contact your local public health office for region-specific information and assistance.
Support Networks:
- Online Forums: Communities where patients and caregivers can share experiences and advice.
- Hotlines: Many countries have established hotlines for Mpox-related inquiries and support.
- NGOs and Health Organizations: Provide education, resources, and support for those affected by Mpox.
15. Conclusion
Mpox, while similar to smallpox, is generally less severe but still poses a significant public health challenge. Public awareness, early diagnosis, effective treatment, and vaccination are critical in controlling the spread of the virus. By staying informed and following recommended guidelines, individuals can protect themselves and their communities from Mpox.
16. References
A list of references should be included, citing the most recent and reliable sources used to compile the guide. This may include scientific journals, public health organizations, and expert guidelines.