Source – https://www.dovepress.com/
Bikila Balis
Department of Midwifery, School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Western Oromia, Ethiopia
Correspondence: Bikila Balis
School of Nursing, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Tel +251 921788619
Email bik.balis2008@gmail.com
Background: Human immunodeficiency virus infection has been one of the top health-related challenges for the past four decades. Ethiopia is extremely infected by HIV pandemic every year, whereby 22,300 people were newly infected and 690,000 were living with HIV at the end of 2018. Sexual behavior of HIV positive individuals visiting treatment clinics is a neglected issue. Nonetheless, it has been a significant way of HIV transmission to serodiscordant partners.
Methods: A facility-based cross-sectional study design was used on a sample of 432 women attending treatment clinics in west Oromia from February 26 to March 26, 2019. Systematic sampling was used to select the study participants. A pretested and structured interviewer-administered questionnaires were used to collect the data. The data were coded, entered, cleaned and exported to SPSS version 20.0 for analysis. Descriptive statistics were used to present frequency distributions. Variables with P-value < 0.25 during bivariate analysis were entered into multiple logistic regression models to control for all possible confounders. Odds ratio along with 95% CI were estimated to measure the strength of the association. Level of statistical significance was declared at a p-value less than 0.05.
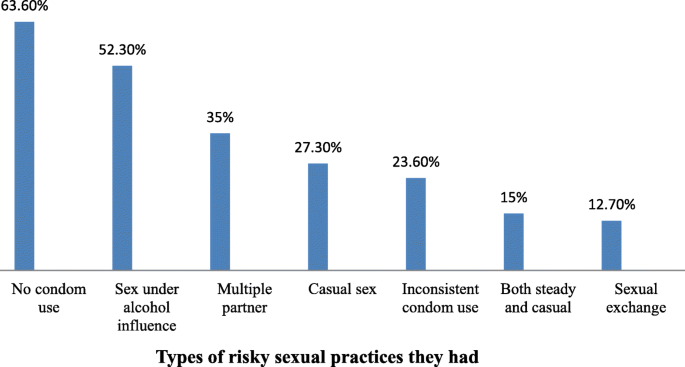
Results: Out of total respondents, 240 (56.9%), 95% CI: (52.1– 61.6%) were involved in risky sexual practices in the prior 12 months. Urban residence [AOR: 3.24, (95% CI: (1.52, 6.89)], those with no formal education [AOR: 2.77, (95% CI: (1.18, 6.54)], being on ART for > 2years [AOR: 2.74, (95% CI: (1.13, 6.65)] and CD4 count ≥ 200 cells/mm3 [AOR: 3.20, (95% CI: (1.50, 6.82)] were factors significantly associated with risky sexual practice.
Conclusion: A considerable number of respondents were involved in risky sexual practices 240 (56.9%) due to being rural residence, not attending formal education, being on ART for > 2 years and CD4 count ≥ 200 cells/mm3.
Keywords: women, HIV/AIDS, risky sexual practices, Oromia, Ethiopia