Introduction to Root Canal Treatment
Root canal treatment is one of the most common dental procedures performed worldwide. Also known as endodontic therapy, it is designed to treat problems in the pulp, the soft inner tissue of the tooth, which contains nerves, blood vessels, and connective tissue. The main goal of root canal therapy is to save a tooth that would otherwise have to be extracted due to infection or decay.
While many people may dread the thought of needing a root canal, advancements in dental techniques and anesthesia have made this procedure safer and far less uncomfortable than ever before. In fact, root canal treatment can significantly improve the quality of life by relieving pain, preventing infection from spreading, and allowing you to retain your natural tooth for many years.
What Is a Root Canal?
The pulp of a tooth contains nerves and blood vessels that help nourish the tooth during its development. However, when the pulp becomes infected due to deep decay, trauma, or repeated dental procedures, it can cause severe pain, swelling, and even abscesses (pus-filled sacs) that can threaten both the tooth and the surrounding tissue.
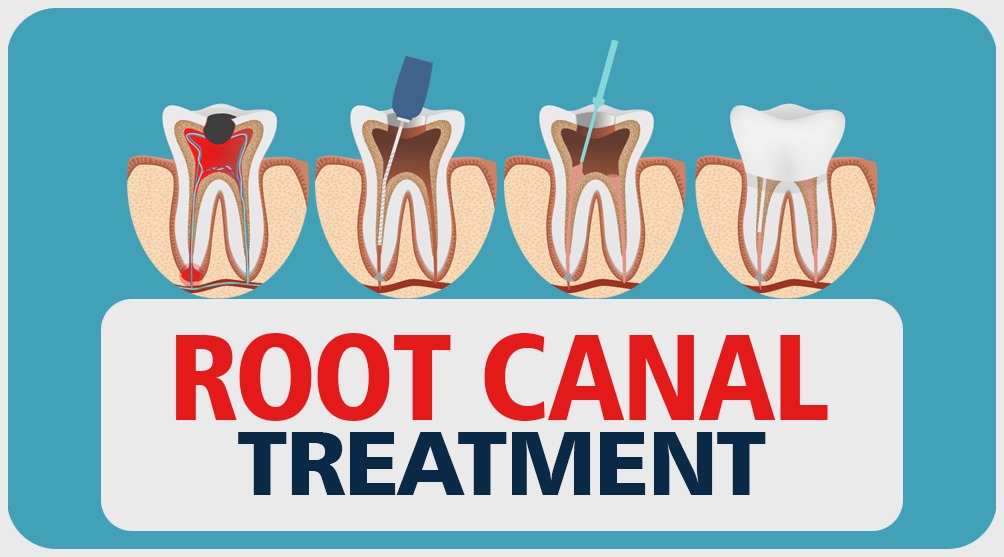
Root canal therapy involves the removal of the infected pulp tissue and cleaning of the root canals. After cleaning and disinfecting the canal, the space is filled with a biocompatible material to prevent future infections. Typically, the treated tooth is restored with a crown to ensure its strength and functionality.
Causes and Risk Factors of Root Canal Issues
Root canal issues typically arise when the inner tissue of a tooth, known as the pulp, becomes infected or damaged. The causes and risk factors for root canal problems are varied and can stem from both internal and external factors. Here's a breakdown:
Causes of Pulp Damage
-
Deep Tooth Decay: The most common cause of pulp infection is untreated dental decay that penetrates deep into the tooth, reaching the pulp.
-
Tooth Trauma or Injury: Even if there are no visible cracks or chips, an injury to the tooth may damage the pulp. A sports injury, car accident, or even a fall can cause internal trauma to the tooth.
-
Repeated Dental Procedures: Multiple dental procedures on the same tooth, such as fillings or crowns, can weaken the pulp and lead to infection.
-
Cracked or Broken Teeth: A cracked tooth allows bacteria to enter the pulp, which can lead to infection or abscess formation.
-
Gum Disease: If gum disease (periodontitis) spreads and reaches the tooth's root, it can cause infection and inflammation in the pulp.
-
Faulty Restorations: Poorly placed fillings or crowns that do not adequately seal the tooth can allow bacteria to enter and infect the pulp.
Risk Factors
-
Age and Genetics: While tooth decay can affect people of all ages, older individuals or those with a genetic predisposition to certain dental conditions may be at a higher risk.
-
Neglecting Oral Hygiene: Not brushing and flossing regularly can cause plaque buildup, leading to tooth decay and eventually pulp infection.
-
High-Sugar Diet: Diets rich in sugar promote tooth decay by feeding bacteria that produce acids, which erode tooth enamel.
-
Previous Tooth Damage: A history of dental trauma or poorly treated cavities increases the likelihood of needing a root canal.
Symptoms and Signs That Indicate the Need for a Root Canal
Root canal problems are often linked to symptoms that suggest infection or damage in the pulp. Early detection of these signs is critical for preventing the spread of infection and avoiding tooth extraction.
Common Symptoms of Root Canal Problems
-
Severe Tooth Pain: Often described as a throbbing or sharp pain, especially when chewing or applying pressure on the tooth.
-
Lingering Sensitivity: Heightened sensitivity to hot or cold foods or drinks that lingers long after the stimulus has been removed.
-
Swollen or Tender Gums: Gums around the affected tooth can become swollen, red, or tender. Sometimes, a pimple-like bump on the gums (fistula) may form due to infection.
-
Tooth Discoloration: A tooth may become darker or grayish, which is often a sign that the pulp is dying or has become infected.
-
Abscess Formation: The presence of an abscess (a painful, pus-filled bump) near the affected tooth is a clear indication that there is an infection within the pulp.
-
Painful to Touch: The tooth may be sensitive to tapping or pressure, making it painful to touch or chew.
-
Swelling of the Face or Jaw: Severe cases of infection can lead to noticeable facial swelling, especially near the affected tooth.
Advanced Symptoms
-
Nerve Damage: If the infection spreads to the surrounding nerves, it may cause numbness or tingling sensations in the affected area.
-
Inability to Close the Mouth Properly: In some cases, the infection or swelling may restrict normal mouth movement, making it painful to close or open the mouth fully.
Diagnosis of Root Canal Problems
Diagnosing the need for a root canal involves a series of steps, combining clinical examination and diagnostic tools to assess the health of the tooth and the surrounding tissue.
Step 1: Comprehensive Examination
The dentist will ask questions about your medical history, dental history, and any symptoms you may be experiencing. A thorough visual inspection of the tooth, gums, and surrounding areas will also be performed to check for visible signs of infection, cracks, or decay.
Step 2: X-Rays
X-rays are essential for visualizing the tooth's internal structure. They provide the dentist with a detailed view of the pulp, roots, and surrounding bone. They can show the extent of decay or infection, as well as any abscesses that may be present.
Step 3: Sensitivity Tests
The dentist may conduct sensitivity tests to determine the health of the tooth's pulp. These tests may include:
-
Cold Sensitivity Test: The dentist applies a cold stimulus to the affected tooth to observe whether the response is prolonged or painful.
-
Electrical Pulp Testing: A small electrical current is applied to the tooth to check for pulp vitality. A lack of response may indicate that the pulp is necrotic.
Step 4: Percussion Tests
Percussion tests involve tapping on the affected tooth with a dental instrument to check for pain or tenderness. Sensitivity to this can indicate an infection or damage to the tooth.
Treatment Options for Root Canal Issues
Once the diagnosis is made, root canal treatment is typically the best option for saving the tooth. The procedure involves several steps that are carefully performed to ensure success.
Step 1: Local Anesthesia
Local anesthesia is administered to numb the tooth and surrounding areas, ensuring the procedure is comfortable for the patient. Sedation options are available for patients with anxiety or for those undergoing more complex treatments.
Step 2: Accessing the Root Canal
The dentist creates an opening in the top of the tooth (the crown) to access the pulp chamber. The infected or inflamed pulp is then removed using special instruments.
Step 3: Cleaning and Shaping
Once the pulp is removed, the root canals are cleaned and shaped to remove any remaining tissue or debris. This step is critical for preventing future infections.
Step 4: Filling the Root Canals
After the canals are thoroughly cleaned and shaped, they are filled with a rubber-like material known as gutta-percha. This material helps to seal the root canal and prevent bacteria from re-entering the tooth.
Step 5: Sealing the Tooth
Once the canal is filled, the dentist seals the opening with a temporary or permanent filling. Most root canal-treated teeth will need a crown to restore the tooth's strength and function.
Prevention and Management of Root Canal Issues
While it is not always possible to avoid the need for a root canal, the following preventive measures can help reduce the risk:
-
Regular Dental Checkups: Routine dental visits allow early detection of cavities, cracks, or other issues that could potentially lead to a root canal.
-
Excellent Oral Hygiene: Brushing twice a day with fluoride toothpaste and flossing daily helps to prevent cavities, gum disease, and tooth infections that can lead to root canal issues.
-
Dietary Choices: Limiting sugary snacks and drinks helps reduce the risk of tooth decay, as sugar feeds harmful bacteria that produce acids that damage tooth enamel.
-
Avoiding Tobacco: Smoking or using tobacco products can increase the risk of gum disease and oral infections, which can lead to the need for a root canal.
-
Timely Treatment for Dental Issues: If you notice any signs of infection, pain, or sensitivity in your teeth, seek dental care promptly to prevent further complications.
Complications of Root Canal Treatment
While root canal treatment is generally safe and effective, there are a few potential complications that patients should be aware of:
-
Infection: In some cases, an infection may persist after the root canal procedure, requiring additional treatment or retreatment.
-
Tooth Fracture: Teeth that undergo root canal treatment are more prone to fracture due to the removal of the pulp. A crown is recommended to protect the tooth from damage.
-
Dry Socket: This condition can occur if the blood clot in the root canal is dislodged or fails to form properly, leading to pain and discomfort.
-
Allergic Reactions: Some patients may have an allergic reaction to the materials used in root canal fillings, although this is rare.
-
Failure to Heal: In rare cases, the tooth may fail to heal properly after the procedure, leading to ongoing infection or the need for tooth extraction.
Living with Root Canal Treatment
After a root canal procedure, most patients experience significant relief from pain and discomfort. However, it is essential to follow the post-treatment care instructions to ensure optimal healing and prevent complications.
Post-Treatment Care Tips
-
Pain Management: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage mild discomfort. Follow your dentist's instructions for pain management.
-
Dietary Adjustments: Stick to soft foods for the first few days after the procedure to avoid putting stress on the treated tooth.
-
Oral Hygiene: Gently brush your teeth, including the treated area, but avoid flossing until the permanent restoration is placed.
-
Follow-Up Appointments: Regular follow-up visits are essential to monitor the healing process and ensure that no further treatment is necessary.
-
Restoration with a Crown: It is crucial to have a crown placed over the treated tooth to protect it from further damage and restore its function.
Top 10 Frequently Asked Questions about Root Canal Treatment
1. What is a root canal treatment?
A root canal treatment is a dental procedure used to treat infection or damage to the pulp of a tooth. The pulp is the soft tissue inside the tooth, containing nerves and blood vessels. During a root canal, the infected or damaged pulp is removed, and the space is cleaned, disinfected, and sealed. The tooth is then restored with a filling or crown to ensure it functions properly.
2. Why do I need a root canal?
You may need a root canal if the pulp inside your tooth becomes infected or inflamed due to:
-
Severe tooth decay that reaches the pulp
-
Trauma or injury to the tooth that causes damage to the pulp
-
Repeated dental procedures on the same tooth
-
Cracked or fractured teeth that allow bacteria to enter the pulp
Without treatment, the infection can spread, leading to abscess formation, severe pain, and even tooth loss. A root canal helps save the tooth and alleviate pain.
3. How do I know if I need a root canal?
Common signs that you may need a root canal include:
-
Severe tooth pain, especially when chewing or applying pressure
-
Lingering tooth sensitivity to hot or cold temperatures
-
Swollen or tender gums near the affected tooth
-
Darkened or discolored tooth
-
Pimple-like bump on the gums near the tooth
If you experience any of these symptoms, it's important to visit your dentist for a proper diagnosis. They may take X-rays to confirm the need for a root canal.
4. Does a root canal hurt?
Many people fear that a root canal is painful, but the procedure is usually no more uncomfortable than getting a regular filling. Local anesthesia is used to numb the area around the tooth, ensuring you don't feel pain during the procedure. Afterward, you may experience mild discomfort or soreness, which can be managed with over-the-counter pain medication. The pain you may experience before the procedure due to the infection is often much worse than the procedure itself.
5. How long does a root canal procedure take?
A typical root canal procedure usually takes about 60 to 90 minutes for a single tooth. The length of time may vary depending on the complexity of the case, the number of roots in the tooth, and the severity of the infection. If the infection is extensive or if the root canal requires multiple visits, the procedure may take longer and require follow-up appointments.
6. What happens during a root canal procedure?
Here's what you can expect during a root canal treatment:
-
Anesthesia: The area around the affected tooth is numbed with local anesthesia to ensure you don't feel any pain.
-
Accessing the tooth: The dentist creates a small opening in the top of the tooth to access the pulp chamber.
-
Cleaning and disinfecting: The infected or damaged pulp is removed, and the space is cleaned and disinfected.
-
Sealing the tooth: The empty space is filled with a biocompatible material, and the opening is sealed to prevent future infection.
-
Restoration: In most cases, a crown or filling is placed on the tooth to restore its function and protect it from further damage.
7. How long will the tooth last after a root canal?
With proper care, a tooth treated with a root canal can last for many years, even a lifetime. The longevity of the tooth depends on several factors, including:
-
The extent of the damage before the root canal
-
How well you follow oral hygiene practices
-
Whether the tooth receives appropriate restoration, such as a crown, after the procedure
Root canal-treated teeth are typically strong and functional, but they can become brittle over time, so it's important to maintain regular dental check-ups.
8. What is the success rate of root canal treatments?
Root canal treatments are highly successful, with a success rate of about 95%. The procedure is designed to remove all infection and seal the tooth to prevent reinfection. Most people experience a significant reduction in pain and are able to keep their tooth for many years after the treatment. However, in some cases, retreatment may be necessary if an infection returns or the tooth is not healing properly.
9. What are the risks and complications of a root canal?
While root canal treatments are generally safe, there are some potential risks, including:
-
Infection: If the tooth is not completely cleaned or sealed, bacteria can re-enter the tooth.
-
Tooth fracture: Root canal-treated teeth can become brittle over time, increasing the risk of fracture, especially if not properly restored with a crown.
-
Failed treatment: In some cases, the root canal may not completely eliminate the infection, leading to the need for retreatment or even tooth extraction.
Your dentist will take measures to minimize these risks and ensure the best possible outcome.
10. How much does a root canal cost?
The cost of a root canal depends on factors like the tooth's location (front teeth are less expensive than molars), the complexity of the case, and whether additional treatments, such as a crown, are needed. On average, a root canal costs between $500 and $2,000 per tooth. Your dental insurance may cover part of the cost, so it's a good idea to check with your provider. If you need a crown or other restoration, the total cost may be higher.


