Introduction to Anal Stretch
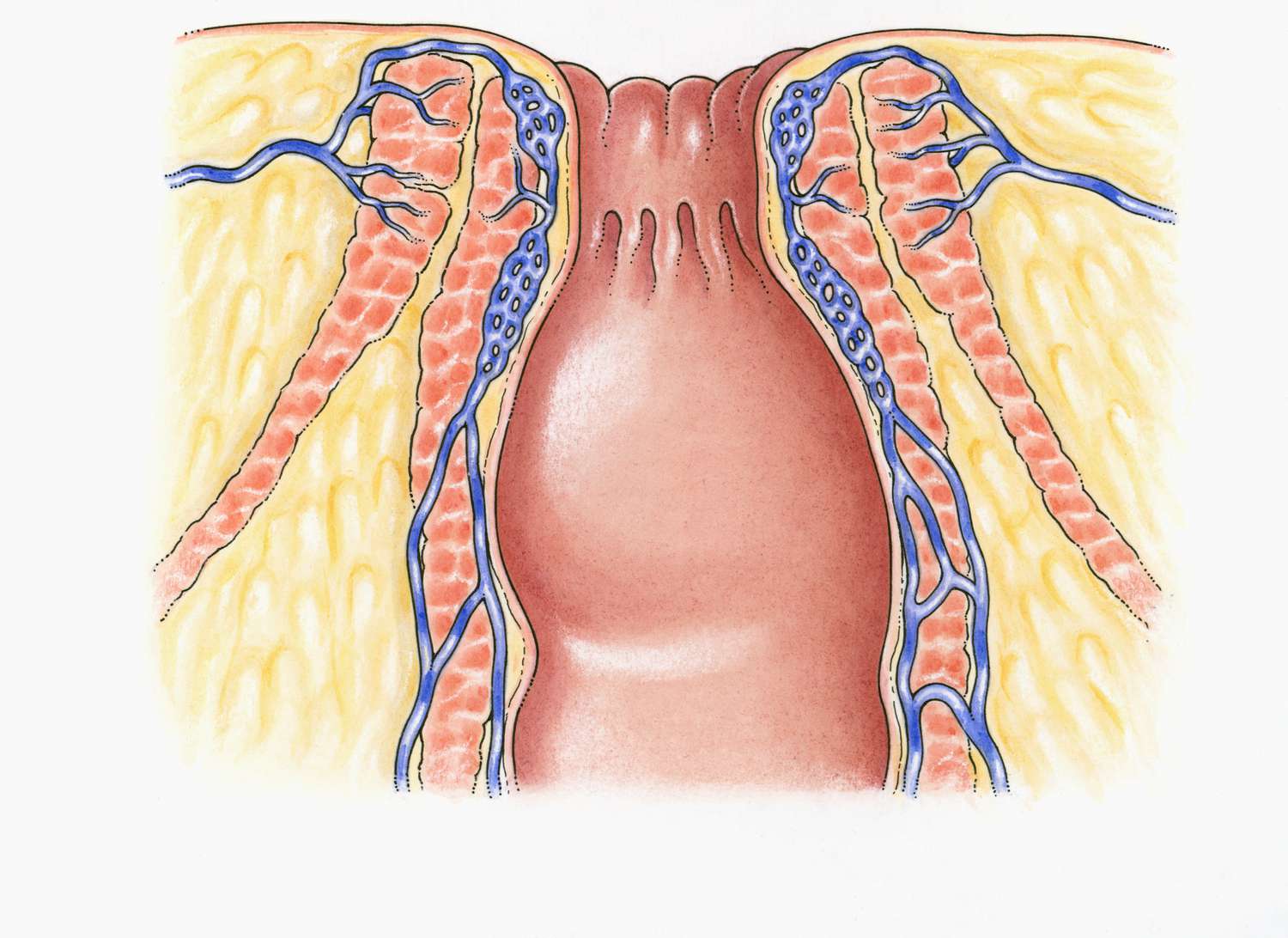
Anal stretching is the process of gradually expanding and relaxing the muscles of the anal sphincter to increase flexibility, comfort, and tolerance in the area. The anal sphincter is a ring of muscles that controls the opening and closing of the anus, and it is naturally tight to maintain continence. Stretching these muscles can be undertaken for multiple purposes, including sexual exploration, preparation for anal intercourse, medical procedures, or therapeutic treatment for conditions like anal fissures or chronic tension in the anal region.
The process typically involves the careful and progressive use of fingers, anal plugs, dilators, or other devices, always paired with adequate lubrication and a slow, patient approach to prevent pain or injury. Successful anal stretching requires attention to anatomy, muscle relaxation, and comfort levels, with a strong emphasis on hygiene to avoid infections. Beyond physical aspects, it also involves mental preparation, as anxiety or tension can increase muscle tightness.
Gradual and consistent practice over time allows the sphincter muscles to adapt safely, enhancing both functional and sensory experiences. While widely discussed in sexual health communities, anal stretching also has recognized medical applications, such as facilitating colonoscopies or aiding recovery after certain anorectal surgeries. Safety, patience, and proper technique remain the cornerstones of effective anal stretching, making it a practice that combines physiological understanding with mindfulness and self-awareness.
Causes and Risk Factors (Why Anal Stretch / Dilation May Be Needed)
Because anal stretch is a treatment modality, not a disease, this section addresses underlying conditions or scenarios in which anal dilation is indicated, as well as risk factors that influence decision-making.
Indications / Situations That Prompt Anal Stretch / Dilation
-
Anal or anorectal stenosis / strictures
-
After surgery (e.g. hemorrhoidectomy, anorectal procedures), scar tissue may contract and narrow the anal canal; dilation helps maintain or restore patency.
-
Following repair of congenital anorectal malformations (e.g. in pediatric settings) to prevent stenosis of the newly formed anal canal.
-
Secondary to chronic inflammatory or infectious disease processes (less common) leading to fibrotic narrowing.
-
-
Supportive therapy post-surgery
-
After certain anorectal operations, surgeons may prescribe dilation to prevent postoperative contraction of tissues (scar contraction) and maintain lumen size.
-
Early dilation can reduce risk of stricture formation.
-
-
Relief of symptomatic tightness / spasm
-
In patients who have hypertonic anal sphincter (muscle spasm) or discomfort, gentle dilation may help relieve muscle tension, reduce spasm, and ease passage of stool.
-
As adjunct therapy in certain chronic anal fissures or anal discomfort settings.
-
-
Preparation for or maintenance of certain medical or sexual practices
-
In some cases, dilation is used (under medical or guided conditions) to ease discomfort from tight anal tissues in contexts of anal intercourse / penetration (though this must be medically supervised if underlying pathology is present).
-
Use of dilators may also help preempt microtrauma or tears in patients with known vulnerability.
-
Risk Factors / Considerations in Patient Selection
-
History of anal incontinence / weak sphincter function — risk of further weakening or damage to sphincter with stretching.
-
Prior surgeries, scarred tissues, fibrosis — less elasticity means more resistance and higher risk of tearing.
-
Poor tissue healing (e.g. diabetes, malnutrition, vascular disease)
-
Very advanced age or general frailty
-
Uncontrolled infections or anorectal disease
-
Patient noncompliance or poor technique in home dilation regimen
-
Excessive force or incorrect use of dilators — risk of injury, tearing, bleeding
-
Anatomical abnormalities in the anal canal or sphincter complex
Modern research on controlled manual anal dilatation suggests that if done properly, risks to sphincter function are lower than older, aggressive stretching techniques. A recent paper (“Long-term Efficacy and Safety of Controlled Manual Anal Dilatation”) reports that standardized protocols may yield favorable outcomes with minimal long-term sphincter damage.
However, more cautious practice is widely adopted because older techniques (e.g. nonstandard Lord's stretch) were associated with higher incontinence rates.
Symptoms and Signs (What Leads Patients to Seek Anal Stretch)
Since anal stretch is a therapy, this section describes the clinical features of the underlying problems (e.g. stenosis, postoperative narrowing, anal discomfort) that lead to considering dilation.
Symptoms (Patient-Reported)
-
Progressive difficulty in passing stool (straining, narrow caliber, discomfort)
-
Pain during defecation
-
Sensation of tightness or constriction in the anus
-
Incomplete evacuation or a feeling of residual stool
-
Occasional bleeding or mucous discharge due to friction/trauma
-
Recurrent anal fissures or microtears due to elevated shear stress
-
In patients with prior surgery, symptoms may worsen over time as fibrosis contracts
-
For post-operative protocols (especially pediatric), failure to maintain anal opening may lead to constipation, pain, or obstructive symptoms
Signs (Exam / Clinical Findings)
-
On digital rectal exam: increased resistance, tight sphincter tone, narrowed canal
-
On anoscopy or proctoscopy: evidence of narrowing, scarring, fibrotic rings
-
In severe stenosis, inability to pass even small probes/dilators
-
Postoperative surgical site contraction or puckering
-
Possible microtears, ulcerations or mucosal inflammation where high friction occurs
Because anal dilation is typically used for structural or mechanical narrowing, the signs are often obvious upon inspection and assessment of anal canal caliber.
Diagnosis Preoperative Evaluation
This section describes how clinicians assess patients to confirm the need for anal stretch/dilation, and to plan a safe, effective protocol.
History & Clinical Evaluation
-
Detailed bowel history: stool consistency, frequency, straining, pain, bleeding
-
Prior anorectal surgeries, injuries, or interventions
-
Incontinence history, sphincter function, continence scoring
-
Comorbid conditions affecting healing (diabetes, vascular disease)
-
Patient's ability and willingness to comply with dilator protocols
Physical Examination
-
External inspection of perianal skin and surgical scars
-
Digital rectal exam: assess sphincter tone, tenderness, resistance, canal diameter
-
Anoscopy / Proctoscopy: visualize the mucosa, luminal narrowing, rings, scarring
-
Try gentle passage of small graduated probes or dilators under controlled conditions to gauge baseline tolerance
Imaging / Ancillary Tests (Selective)
-
Endoscopy (sigmoidoscopy / colonoscopy) if suspicion of deeper rectal pathology or inflammatory disease
-
Manometry or sphincter function tests (in select patients) to document baseline sphincter pressures
-
MRI / ultrasound imaging of the anal sphincter complex if anatomical disruption or incontinence risk is a concern
Planning & Protocol Design
-
Determine initial dilator size, target size, frequency, and progression schedule
-
Provide clear patient (or caregiver) education, demonstrations, and supervised practice
-
Assess risk vs benefit carefully, especially in patients with borderline continence
-
Set follow-up and monitoring schedule to catch complications early
In many pediatric protocols (e.g. after anorectal surgery), dilation is introduced early (within weeks) and gradually advanced, with schedules tapering over months.
Treatment Options Protocols
This is the core section. It covers the array of techniques (manual, device, balloon), their pros/cons, and how they are used in practice.
A. Manual Stretching / Controlled Manual Anal Dilatation
-
Traditional Lord's procedure of manual, forceful stretching of the anal canal is largely out of favor today due to variable results and risk of sphincter damage.
-
Controlled manual dilatation uses a defined finger count, gentle incremental expansion under anesthesia or sedation, and standardized protocols. Recent studies show that carefully executed controlled manual dilation can maintain or improve canal caliber with low rates of long-term sphincter injury.
-
After manual dilation, patients often follow up with maintenance dilator sets.
B. Gradual Dilator / Probe Methods (Outpatient / Home Protocols)
-
Use of sets of graduated anal dilators or probes of increasing diameters, usually made of medical-grade stainless steel, silicone, or inert materials.
-
The patient or caregiver gently inserts the dilator (lubricated) to the prescribed depth, holds for a specified duration, may rotate slightly, then withdraws. Over time, larger diameters are introduced as tolerated.
-
The frequency (daily, twice daily, every other day) and duration (minutes) vary by protocol and indication.
-
This approach is particularly useful in postoperative care (to prevent contraction) and in milder stenosis cases.
C. Balloon Dilatation
-
Balloon dilation is done in a controlled medical setting: an uninflated balloon is inserted into the anal canal and gradually inflated to stretch the tissues. Some studies report favorable healing rates in patients with anal fissures or stenosis using balloon dilation, with less trauma than blind stretching.
-
This method allows precise control over diameter increase and reduces the risk of overt stretching trauma.
D. Combination / Adjunctive Therapies
-
Topical therapies, such as nitroglycerin, nifedipine, or diltiazem, may reduce sphincter tone and improve comfort during dilation.
-
Botulinum toxin (Botox) injection into internal sphincter may relax the muscle temporarily and make dilation easier or reduce recurrence.
-
In cases of severe or refractory stenosis, surgical enlargement, mucosal advancement flaps, or scar resection may be needed, and dilation is adjunctive.
-
In pediatric or congenital anorectal repair patients, dilation is standard postoperative maintenance therapy along with stool regimen, diet, and monitoring.
E. Choosing the Appropriate Method
The decision considers:
-
Severity of narrowing (mild, moderate, severe)
-
Patient age, tolerance, and compliance
-
Baseline continence function and sphincter health
-
Presence of scarring or fibrosis
-
Necessity of anesthesia vs outpatient approach
-
Risk tolerance and prior history
For example, in mild postoperative narrowing, a dilator protocol may suffice. In more severe, fibrotic strictures, balloon dilation or surgical correction plus maintenance dilators might be favored.
Prevention Management (Avoiding Recurrence / Optimizing Outcomes)
This section gives strategies to prevent needing dilation and to reduce relapse or complications in patients already undergoing it.
Prevention (Primary / Before Problem Emerges)
-
During anorectal surgeries, use tissue-sparing techniques to minimize excessive scarring.
-
Prophylactic early gentle dilation when surgeon anticipates contraction risk (especially in pediatric reconstructions).
-
Adequate postoperative care: stool softeners, fiber, hydration, pain control, avoiding strain.
-
Aggressive management of constipation or bowel motility issues.
Management & Maintenance (After Initial Dilation / Procedure)
-
Strict adherence to dilator schedule as prescribed (frequency, duration, progression).
-
Gradual tapering rather than abrupt cessation of dilation to maintain lumen.
-
Ongoing stool consistency management: fiber, laxatives, stool softeners to avoid trauma.
-
Monitor for signs of constriction early; reinstitute dilation at recurrence.
-
Regular follow-up visits and possible re-evaluation of dilator size or technique.
-
In receptive-risk patients (children, prior surgeries), periodic “maintenance” dilation even when asymptomatic may be considered.
Patient Education & Compliance
-
Clear instructions (written + demonstration) are essential.
-
Emphasize gentleness, patience, hygiene, lubrication, and listening to body signals.
-
Encourage reporting of bleeding, sharp pain, or resistance early.
-
Monitor progression—if dilation becomes too easy, move to the next size; if too painful, regress or pause.
-
Ensure clean technique to prevent infection.
Complications of Acne
Any medical intervention carries risk; dilation is no exception, especially in delicate tissues. This section should honestly present possible adverse outcomes, so patients and clinicians can weigh benefits vs risks.
Common / Mild Complications
-
Mild discomfort or soreness after dilation
-
Minor bleeding or spotting, especially when increasing dilator size
-
Local irritation or mucosal microtrauma
-
Transient increase in mucous discharge
Moderate / Less Common Risks
-
Tissue tears or lacerations if force or poor technique is used
-
Infection at the dilated site if hygiene is inadequate
-
Scarring / fibrosis if repeated injury or trauma occurs
-
Stricture recurrence if dilation is inadequate or discontinued
-
Pain or hypersensitivity if nerve endings are irritated or trauma is repeated
Serious / Rare Risks
-
Sphincter injury / internal anal sphincter damage — historically a major concern, especially with aggressive stretching (Lord's technique). Many surgeons now avoid nonstandardized stretch for this reason.
-
Fecal incontinence (flatus or stool leakage) — risk depends on extent of sphincter damage or baseline weakness
-
Hemorrhage / hematoma formation
-
Deep tissue necrosis (very rare)
-
Severe pain or crisis necessitating halting the protocol
In the 2023 controlled manual dilation study, results indicated low rates of continence issues when strict protocols are followed, but vigilance remains essential.
Because of historical risk from aggressive methods, many colorectal surgeons prefer alternative or adjunctive strategies (e.g. balloon dilation, surgical correction) to mitigate those risks.
Living with the Condition Aftercare / Patient Experience
This section is patient-oriented: what to expect during recovery, how to plan daily life, and tips for success with dilation protocols.
Recovery & Adjustment Period
-
The first sessions may cause mild discomfort; expect some soreness, mucus, or slight bleeding.
-
Begin with gentle, minimal dilation; never force resistance.
-
Use soothing measures after dilation: sitz baths, analgesics, gentle perianal hygiene.
-
Progress gradually: only increase dilator size once the previous one moves smoothly without pain or resistance.
Daily Life & Practical Tips
-
Always lubricate generously with a water-based or compatible lubricant.
-
Use clean technique: wash hands, clean dilator before/after each use.
-
Try to pick comfortable times when relaxation is optimal (warm bath before, calming environment).
-
Maintain soft, regular stools—avoid hard strain (fiber, water, stool softeners).
-
Keep a log or chart: dilator size, duration, any discomfort or bleeding.
-
Don't rush progression; waiting even a few extra days longer is safer than pushing too fast.
-
Pause and regress if you hit pain, resistance, or bleeding, then restart gently.
Long-Term & Maintenance
-
Once desired caliber is achieved, taper frequency gradually but continue occasional dilation to maintain patency.
-
Monitor symptoms: if narrowing recurs, reinstitute dilation early.
-
In patients who had surgeries (especially pediatric reconstructions), lifelong periodic evaluation may be necessary to guard against late contraction.
-
Be alert to red-flag signs: new onset incontinence, severe pain, bleeding, inability to insert small dilators — seek doctor's evaluation.
Quality-of-Life Considerations & Psychological Aspects
-
Patients may be anxious about discomfort, embarrassment or incontinence risks; setting realistic expectations is key.
-
Frequent, gentle dilation is better accepted than abrupt or forceful sessions.
-
Provide patient support, counseling, and gradual escalation to build confidence.
-
Encourage patients to maintain open communication with the treating colorectal or GI specialist.
Top 10 Frequently Asked Questions about Anal Stretch
1. What is an Anal Stretch?
An Anal Stretch, also known as anal dilatation or anal stretching procedure, is a medical procedure performed to relieve anal tightness or spasms, often caused by conditions such as anal fissures, chronic constipation, or anal stenosis. The procedure involves gently stretching the anal canal under controlled medical supervision to reduce pain, improve bowel movements, and prevent tearing.
2. Who needs an Anal Stretch?
Anal Stretch is recommended for individuals experiencing:
-
Chronic anal pain or tightness
-
Anal fissures that do not heal with conservative treatment
-
Constipation or difficulty passing stool due to a tight anal sphincter
-
Post-surgical anal stenosis
A thorough evaluation by a colorectal surgeon or proctologist is required to determine if the procedure is suitable.
3. How is an Anal Stretch performed?
Anal Stretch can be done under local anesthesia, sedation, or general anesthesia depending on patient comfort and the extent of stretching needed.
The procedure typically involves:
-
Lubricating the anal canal with a medical-grade gel.
-
Using specially designed dilators to gently stretch the anal sphincter.
-
Maintaining the stretch for a controlled duration to prevent muscle injury.
The procedure is usually quick, often completed in 15-30 minutes, and may be performed on an outpatient basis.
4. Is Anal Stretch painful?
Most patients experience minimal discomfort due to local anesthesia or sedation. Some mild pressure or stretching sensation may be felt during the procedure. After the procedure, temporary soreness or mild bleeding can occur but usually resolves within a few days.
5. What is the recovery time after Anal Stretch?
Recovery from an anal stretch is generally short:
-
Immediate post-procedure: Patients can usually go home the same day.
-
First 1-2 days: Mild soreness or slight bleeding may occur. Pain can be managed with over-the-counter pain relief.
-
First week: Most patients can resume normal activities. Stool softeners and increased hydration may be recommended to avoid strain.
Complete healing and normalization of bowel movements typically occur within 1-2 weeks.
6. Are there any risks or complications?
Anal Stretch is generally safe but may carry some risks:
-
Mild bleeding or bruising
-
Temporary anal soreness or discomfort
-
Rarely, anal tearing or infection
-
Risk of over-stretching, which can affect sphincter function
Choosing an experienced colorectal surgeon significantly reduces these risks. Following post-procedure care instructions is critical.
7. Can Anal Stretch be done at home?
While gentle anal dilators can sometimes be used at home under a doctor's guidance for minor cases, professional medical supervision is strongly recommended for:
-
Severe anal stenosis
-
Chronic anal fissures
-
Post-surgical narrowing
Improper stretching at home can cause tears, bleeding, or incontinence.
8. How long do the results of Anal Stretch last?
The effects of Anal Stretch vary based on the underlying condition:
-
For anal fissures or minor tightness: Relief may be long-lasting if underlying causes are addressed.
-
For severe anal stenosis: Multiple sessions may be required for optimal results.
Lifestyle modifications, stool softeners, and avoiding chronic constipation help maintain the benefits.
9. How should I prepare for an Anal Stretch procedure?
Preparation usually includes:
-
Bowel preparation: A mild enema may be required before the procedure.
-
Medical evaluation: Discuss any medications (blood thinners, anticoagulants) with your surgeon.
-
Fasting: Required if sedation or general anesthesia is used.
-
Hygiene: Cleanliness of the anal area is important to reduce infection risk.
Your surgeon will provide specific pre-procedure instructions tailored to your needs.
10. Is Anal Stretch a permanent solution?
Anal Stretch provides effective short-term relief, especially for painful anal tightness or fissures.
-
In many cases, results are long-lasting when combined with dietary modifications, high-fiber diet, and stool softeners.
-
For severe or recurrent anal stenosis, multiple treatments or surgical interventions may be required.
Proper follow-up care and preventive measures help maintain the procedure's benefits over time.


