Introduction to Alaplasty
Alaplasty is a specialized cosmetic surgical procedure that focuses on reshaping or reducing the width of the nasal alae — the outer flaring parts of the nostrils — to create a more balanced and proportionate appearance of the nose and face. It is often performed to address aesthetic concerns such as wide, flared, or asymmetrical nostrils, which may be due to genetic factors, ethnicity, or the result of previous nasal surgeries. The primary goal of alaplasty is to refine the nasal base, improve facial harmony, and enhance the overall aesthetics of the nose without compromising its natural function or breathing ability.
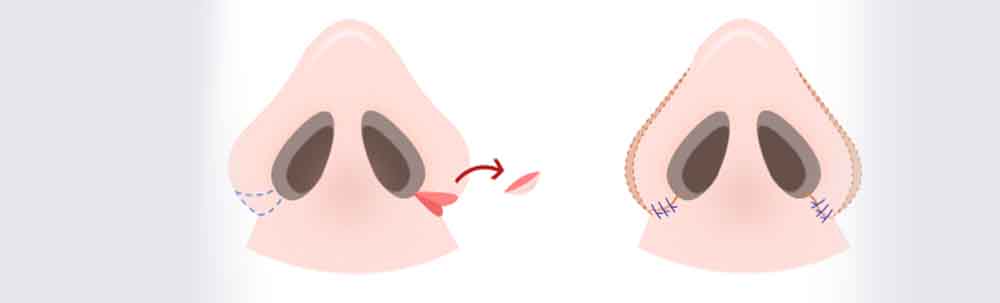
During alaplasty, small incisions are typically made at the natural creases where the nostrils meet the cheeks, allowing the surgeon to remove or reposition a wedge of tissue. This technique helps narrow the nostrils or alter their flare in a controlled and symmetrical way. Depending on the individual's needs, alaplasty can be performed as an isolated procedure or as part of a comprehensive rhinoplasty. Surgeons often consider factors such as nasal tip shape, facial proportions, and ethnic characteristics to ensure that the final outcome appears natural and preserves the patient's unique features.
Postoperative care plays a crucial role in achieving optimal results. Swelling and mild bruising are common in the early recovery phase, but these effects typically subside within a few weeks. Patients are usually advised to avoid strenuous activities and direct pressure on the nose during healing. When performed by an experienced surgeon, alaplasty can produce long-lasting improvements in nasal contour, enhance self-confidence, and create a more refined yet natural-looking appearance. Overall, alaplasty is a precise and artistic procedure that combines surgical skill with aesthetic judgment to harmonize the nose with the rest of the face.
Causes and Risk Factors for Considering Alaplasty
Strictly speaking, "alaplasty" is not a disease but a surgical procedure. However, there are anatomical, cosmetic, or functional reasons why a person may seek alaplasty. Below are the common indications or underlying situations (i.e. "causes") motivating the surgery, and risk factors influencing outcomes.
Indications / "Causes" for the Procedure
-
Wide or flared nostrils (alar flaring)
Some individuals have naturally broad alar bases or nostrils due to genetic or ethnic nasal structure. They may feel the nostrils are disproportionate to the rest of the nose or face. -
Post-traumatic changes or deformity
Injury to the nose or prior surgeries (e.g. trauma repair, previous rhinoplasty) can distort the alar base or nostril shape, requiring targeted correction. -
Asymmetry of the nostrils / alar bases
One nostril may appear more flared, wider, or misaligned, either congenitally or after surgery or injury. Alaplasty can help restore symmetry. -
Functional breathing concerns
In some cases, overly wide alae or irregular nostril shape interferes with airflow dynamics (especially in combination with other nasal structural issues). A modest alar base reduction may assist in improving airflow or relieve turbulence. -
Cleft lip / cleft palate nasal deformities
In patients with cleft lip/nose deformities, alar correction (ala plasties) is often part of secondary nasal reconstruction to correct alar asymmetry. -
Cosmetic dissatisfaction
Many seek alaplasty purely for aesthetic reasons — to refine nose shape, improve facial balance, or boost self-image.
Risk Factors / Predictors of Poor Outcomes
While the surgery is relatively safe, several patient- or procedure-related factors may increase risk or complicate results:
-
Poor general health or comorbidities (e.g. uncontrolled diabetes, vascular disease)
-
Smoking or tobacco use (impairs healing)
-
Thin or fragile skin over the alar region
-
Prior nasal surgeries, scar tissue, or altered blood supply
-
Excessive tissue removal or overly aggressive correction (leading to distortion)
-
Poor surgical planning or inexperience of surgeon
-
Inadequate patient expectations or unrealistic goals
In planning content, you may want to emphasize the importance of selecting a skilled, board-certified plastic surgeon to minimize risks.
Symptoms / Signs / Presentation
Since alaplasty is a surgery, there's no "disease" to present symptoms. But when advising prospective patients, consider what signs/concerns drive individuals to seek this procedure. In addition to those, we should discuss the postoperative signs / expected physical changes.
Preoperative Signs / Concerns (What patients notice)
-
Noticeably wide or flared nostrils, particularly when viewed frontally
-
Nostril shape that appears disproportionate relative to the nose or face
-
Flaring or spreading of the nostril base during inhalation or facial expression
-
Asymmetry — one nostril looks larger or more open
-
Feedback from others about nose shape or flaring
-
Psychological or emotional discomfort / dissatisfaction with appearance
Postoperative / Recovery Signs
These are expected and not necessarily "abnormal":
-
Swelling, redness, bruising around nostrils especially early (day 1–7)
-
Mild discomfort or tightness around the surgical site
-
Minor bleeding or oozing, especially in first 1–2 days
-
Tenderness to touch
-
Slight nasal obstruction or stuffiness (due to swelling)
-
Temporary change in sensation or mild numbness around the incision site
-
Gradual resolution of swelling over weeks to months
If signs such as persistent pain, increased redness, pus, severe bleeding, or asymmetry occur, they may indicate complications (see "Complications" later).
Diagnosis / Preoperative Evaluation
Before proceeding with alar base surgery, a careful evaluation is required to plan the surgery precisely and screen for contraindications. Below is how the "diagnosis" or preoperative workup typically proceeds.
1. Consultation & History
-
Comprehensive medical history (comorbidities, bleeding disorders, medications, prior nasal or facial surgeries)
-
Allergies, smoking status
-
Patient's aesthetic goals and expectations
-
Discussion of nasal breathing or functional issues if present
-
Physical examination and photography (frontal, lateral, basal views)
2. Physical Examination & Nasal Assessment
-
Inspection of nostril shape, width, flare, asymmetries
-
Measurement of interalar distance (distance between outermost edges of nostrils)
-
Assessment of alar rim position, alar base insertion relative to cheek
-
Skin thickness and quality over alar region
-
Internal nasal examination (if breathing issues present)
-
Evaluation of other nasal structural issues (septal deviation, internal valve collapse)
3. Imaging (If Needed)
In many typical cases of isolated alar base reduction, imaging (CT, MRI) is not required. However, if the patient has complex nasal deformities or prior surgeries, imaging may help in surgical planning.
4. Surgical Planning & Marking
-
Preoperative digital / printed images help planning
-
Surgeon marks incision lines (e.g. wedge excision, sill excision, V–Y advancement) on the patient's skin to guide precise removal and closure
-
Simulations or sketches of expected change may help patient–surgeon communication
5. Laboratory / Pre-op Tests
-
Standard preoperative labs (CBC, coagulation profile, metabolic panel)
-
Medical clearance if the patient has systemic diseases
-
Preoperative instructions (cease blood-thinning medications, smoking cessation, etc.)
This diagnosis/planning phase helps ensure safety, symmetry, and alignment with patient goals.
Treatment Options / Surgical Techniques
This is the core of your content. Here you describe what treatment (surgical) options exist under the umbrella of "alaplasty / alar base reduction," how they are done, pros/cons, and adjunctive techniques.
Overview
Because the alar base reduction is a localized procedure, treatment is always surgical (no effective non-surgical alternative exists for true narrowing).
Surgeons choose among various techniques or combinations depending on the anatomical needs. Common techniques include:
-
Alar wedge excision (Weir incision, alar base wedge resection)
-
Nostril sill excision
-
V–Y advancement of ala
-
Combination techniques or diamond wedge excision
-
Alar cinching / subcutaneous flap or cinch sutures
-
Revision / secondary corrections
Below is more detail:
1. Alar Wedge Excision (Weir / Base Wedge)
-
The most classic and common technique. A small wedge-shaped piece of tissue is excised at the junction of nostril and cheek along the natural crease (alar base crease).
-
Removal of that wedge allows the two edges to be approximated more medially, narrowing the alar base width.
-
This technique preserves the natural curvature and can yield a hidden scar in the crease.
-
Pros: simple, effective, predictable
-
Cons: overcorrection risk, visible scar if not well placed
2. Nostril Sill Excision
-
In some patients, the width is largely contributed by the nasal sill (the base floor of the nostril), not just the side walls. In such cases, an excision is made along the sill to reduce width.
-
Can be done in combination with alar wedge excision to fine-tune the shape.
3. V–Y Advancement
-
Instead of removing tissue, a V-shaped incision is made in the alar region, and closure in a Y-shape allows repositioning / advancement of the ala medially.
-
This is a tissue-conserving technique and useful when only shape adjustment is needed rather than major reduction.
4. Diamond Wedge / Diamond Excision Extensions & Alar Cinching
-
Some advanced techniques incorporate diamond wedge excision plus modification of sidewall curvature, or alar cinching (suturing to cinch or tighten soft tissue) for enhanced control.
-
These allow better control over the three-dimensional shape of the alar base.
-
The "Diamond wedge excision with subcutaneous flaps" approach is described in plastic surgery literature to refine the axis, sidewall contour, and reduce distortion.
5. Combined / Hybrid Approaches
-
In many patients, multiple techniques are combined (e.g. alar wedge + sill excision + cinch sutures) to optimize shape, symmetry, and minimize undesirable side effects.
6. Revision / Secondary Alaplasty
-
Some individuals require revision surgery (e.g. in case of asymmetry, overcorrection, or scarring). Planning for potential revision should be part of the informed consent.
-
Revision techniques often involve more delicate tissue handling and sometimes grafting or soft tissue rearrangement.
Anesthesia, Duration, and Logistics
-
Alaplasty is often done under local anesthesia ± sedation. In combined cases (with rhinoplasty) general anesthesia may be used.
-
The procedure is typically 30 to 60 minutes, depending on complexity and combination with other nasal procedures.
-
The incisions are sutured (often with fine, dissolvable or fine non-dissolvable sutures) and dressed.
-
Many patients are day-case (same-day discharge) unless combined surgery or special circumstances.
Postoperative Care / Adjunctive Measures
-
Nasal splints or internal supports may be used briefly
-
Cold compresses, head elevation, limited movement
-
Antibiotics, analgesics, and avoidance of nasal trauma
-
Scar care (silicone gel, massage) once healing permits
You can expand this section with diagrams, before & after photos, and surgeon quotes.
Prevention Management (Before and After Surgery)
Though surgical, there are steps patients can take before and after to optimize outcomes, reduce risks, and manage expectations. This section is a good place to offer patient-friendly "tips & best practices."
Preoperative (Prevention of Complications)
-
Choose a qualified, experienced plastic surgeon (board-certified, good track record)
-
Realistic expectations: the goal is refinement, not a completely new nose
-
Stop smoking well before (ideally weeks) the surgery
-
Discontinue blood-thinning medications/supplements (aspirin, NSAIDs, herbal supplements) as advised
-
Manage comorbid conditions (diabetes, hypertension)
-
Avoid skincare irritation or active skin infections around the nose prior to surgery
-
Preoperative photos, marking, and planning in detail
Immediate Postoperative (First few days to weeks)
-
Head elevation (sleep with extra pillows) to reduce swelling
-
Cold compresses applied intermittently (with care to avoid pressure)
-
Gentle cleaning of incision sites as instructed
-
Strict avoidance of blowing nose, forceful sneezing, or touching the nose
-
Medication adherence (antibiotics, analgesics)
-
Soft diet if needed; avoid strenuous activity
-
Use of scar therapy (silicone gel sheets, massage) once healing is adequate
-
Avoid direct sun exposure to surgical area (use sunscreen after healing)
-
Follow-up visits and suture removal (usually after ~1 week)
Long-Term / Maintenance
-
Monitor for scar formation or hypertrophic/keloid scarring; treat early with steroids or silicone
-
If minor asymmetries appear, consider non-invasive adjuncts or minor touch-ups
-
Protect the nose from trauma
-
Maintain realistic expectations: subtle improvements are often more harmonious
-
For combined rhinoplasty patients, adhere to full nasal care and follow-up protocols
Emphasize that adherence to surgeon instructions is critical for successful outcome.
Complications Risks of Alaplasty
Though relatively low-risk compared to more extensive nasal surgery, alaplasty has potential complications, some of which are serious. This section should be thorough to inform patients properly.
Common / Mild Risks
-
Swelling, bruising, redness (expected, usually transient)
-
Mild bleeding or oozing early post-op
-
Discomfort / pain / tightness (usually manageable with analgesics)
-
Temporary changes in sensation (numbness or tingling)
-
Mild nasal obstruction during early healing
Moderate / Less Common Risks
-
Infection — requires prompt treatment to avoid further complications
-
Poor wound healing / dehiscence (opening of incision)
-
Scarring / hypertrophic scars / keloids (especially in susceptible individuals)
-
Asymmetry or unsatisfactory correction (one side more reduced than the other)
-
Overcorrection / excessive narrowing — may lead to distortion or impaired nasal function
-
Distortion of alar rim / nostril shape (e.g. notching, retraction)
-
Visible or unfavorable scars if incision placement or technique is suboptimal
-
Change in nasal airflow if narrowing is too aggressive
-
Need for revision surgery
Rare / Serious Risks
-
Hematoma formation
-
Tissue necrosis (if blood supply compromised)
-
Adverse reaction to anesthesia
-
Permanent numbness or altered sensation
-
Unpredicted aesthetic result requiring further surgery
You should also include in your content the importance of discussing these risks in the informed consent process, and emphasize that careful preoperative planning, conservative technique, and surgeon experience reduce complications significantly.
Living With the Condition / After Surgery: Patient Experience Recovery
This section helps readers envision postoperative recovery, quality of life, what to expect, and timeline. It also offers reassurance and practical advice.
Early Recovery (First Week)
-
Expect swelling, redness, mild discomfort, and possibly some light bleeding
-
Sleep with head elevated
-
Gentle care of incision, no touching or manipulation
-
Avoid strenuous activity, bending over, or heavy lifting
-
Many patients can resume light daily tasks within 2–3 days (depending on comfort and surgeon's advice)
-
Suture removal typically around 7 days
Intermediate Recovery (Weeks 2 to 6)
-
Swelling gradually reduces; nasal shape becomes clearer
-
Light activities may resume; avoid contact sports or anything that pressures the nose
-
Scar maturation begins; scar often initially pink then fades over months
-
Use of scar gels, massage, sunscreen over scars
Late Recovery (3 to 12 Months)
-
Final contour of nostrils becomes evident over several months
-
Scars continue to soften and fade
-
If minor residual asymmetries remain, some surgeons may consider touch-up corrections after full healing
-
Patients often adapt to new nasal shape, see improvements in confidence
Patient Satisfaction & Psychological Impact
-
Many patients report improved facial harmony, satisfaction with nose proportions, and enhanced self-esteem
-
It helps to show before/after photos, patient testimonials, and realistic result expectations
-
For patients with breathing issues, improvement may also contribute to functional benefit
When to Contact Your Surgeon
Include a "red flag" list for patients:
-
Persistent or worsening pain not relieved by medications
-
Increased redness, swelling, or heat around incision
-
Purulent drainage (pus), foul odor, or fever — signs of infection
-
Significant bleeding
-
Wound separation or exposure of deeper tissue
-
Marked asymmetry or distortion
-
Difficulty breathing beyond expected swelling
Long-Term Follow-up
-
Schedule periodic follow-ups to monitor healing, scar progression, and satisfaction
-
In rare cases, revision surgery may be considered after 6–12 months
-
Encourage patients to maintain realistic expectations: even perfect surgery has biological variation
Top 10 Frequently Asked Questions about Alaplasty
1. What is Alaplasty (Alarplasty)?
Alaplasty, also known as Alar Base Reduction Surgery or Nostril Reduction
Surgery, is a type of cosmetic nasal procedure designed to alter the shape,
size, or flare of the nostrils. It primarily targets the alar base — the outer
edges of the nostrils — to achieve a more balanced and refined nasal appearance.
The goal of alaplasty is to create harmony between the nose and other facial features.
It is a commonly requested procedure among individuals who feel their nostrils are too
wide, too open, or asymmetrical. Alaplasty can be performed as a standalone procedure or
in combination with rhinoplasty (nose reshaping surgery) for a comprehensive aesthetic
improvement.
2. Who is an ideal candidate for Alaplasty?
The best candidates for alaplasty are individuals who:
-
Feel their nostrils appear too wide or flared when viewed from the front.
-
Desire a more refined nasal base without changing the overall nasal shape.
-
Have realistic expectations about surgical results.
-
Are in good physical and psychological health.
-
Do not smoke or are willing to stop smoking before and after surgery.
-
Are generally 18 years or older, as facial growth is usually complete by that age.
Alaplasty is suitable for people of all ethnicities. In fact, it's often chosen by patients seeking ethnic rhinoplasty enhancements — aiming to preserve their natural ethnic features while achieving a more proportionate look.
3. How is the Alaplasty procedure performed?
Alaplasty is typically performed under local anesthesia with sedation, although general
anesthesia may be used for combined procedures.
During the surgery:
-
The surgeon makes precise, small incisions at the base of the nostrils — usually within the natural creases, minimizing visible scarring.
-
A wedge, crescent, or triangular piece of tissue is carefully removed to reduce the width of the nostrils.
-
The remaining tissue edges are meticulously sutured together to achieve a more refined nasal base.
The surgery usually takes 30 minutes to 1 hour. The simplicity and precision of alaplasty make it an outpatient procedure, meaning patients can go home the same day.
4. What are the benefits of Alaplasty?
The benefits of alaplasty extend beyond aesthetics. Common advantages include:
-
Improved nasal symmetry and balance with the rest of the face.
-
Reduction of nostril width or flare for a softer and more proportionate nasal appearance.
-
Natural-looking results that complement existing nasal features.
-
Permanent correction, with results that last a lifetime.
-
Minimal downtime and relatively quick recovery compared to full rhinoplasty.
For many patients, alaplasty brings greater self-confidence and facial harmony without significantly altering their natural appearance.
5. Will there be visible scars after Alaplasty?
Most patients experience minimal to no visible scarring. The incisions are typically
hidden in the natural crease where the nostril meets the cheek. Over time, these scars
fade and become almost invisible.
Surgeons use fine, dissolvable sutures and advanced closure techniques to ensure optimal
healing and aesthetic results. Regular application of scar-reducing creams or silicone
gel, as recommended by your surgeon, can further improve scar appearance.
6. What is the recovery process like after Alaplasty?
Recovery from alaplasty is generally straightforward. Most patients experience mild
swelling, redness, and tenderness around the nostrils for the first week. Bruising is
usually minimal.
Typical recovery timeline:
-
Day 1–3: Mild discomfort, controlled with pain medication.
-
Day 4–7: Swelling and bruising start to subside; stitches may be removed if non-dissolvable.
-
Week 2: Most visible swelling fades, and normal activities can resume.
-
Week 4–6: Final results become more apparent as tissues heal and settle.
Patients are advised to avoid strenuous activities, nose rubbing, or wearing glasses directly on the nose during the early healing phase.
7. What are the potential risks or complications of Alaplasty?
Like any surgical procedure, alaplasty carries certain risks, although complications are
rare when performed by a skilled surgeon.
Possible risks include:
-
Infection at the incision site.
-
Mild bleeding or hematoma (blood accumulation).
-
Asymmetry or uneven healing.
-
Excessive scarring (rare).
-
Overcorrection or undercorrection of nostril width.
Choosing a board-certified plastic or facial surgeon with extensive experience in nasal surgeries is the best way to minimize these risks and ensure optimal results.
8. Can Alaplasty be combined with other cosmetic procedures?
Yes, alaplasty is often performed alongside other cosmetic surgeries for enhanced results. Common combinations include:
-
Rhinoplasty: For reshaping the entire nose along with nostril refinement.
-
Tip Plasty: To refine the nasal tip and balance nostril shape.
-
Septoplasty: To correct a deviated septum for better breathing function.
Combining procedures not only saves recovery time but also ensures aesthetic consistency across all nasal features.
9. How long do the results of Alaplasty last?
The results of alaplasty are permanent. Once the nostrils have been
reshaped and tissues have fully healed, they maintain their new size and contour for
life.
However, patients should note that normal aging processes may subtly change facial
features over decades, though these changes rarely affect the results of alaplasty.
10. How much does Alaplasty cost, and is it covered by insurance?
The cost of alaplasty varies depending on several factors:
-
Geographic location and clinic reputation.
-
Surgeon's expertise and qualifications.
-
Whether the procedure is combined with rhinoplasty.
-
Facility and anesthesia fees.
In general, the average cost ranges between $1,500 and $4,000 USD. Since
alaplasty is primarily a cosmetic procedure, it is not covered by health
insurance unless performed for reconstructive or functional reasons (such
as nasal trauma correction or congenital deformities).
During your consultation, your surgeon will provide a detailed cost estimate, including
post-operative care.


