Introduction to VSD (Ventricular Septal Defect) Closures
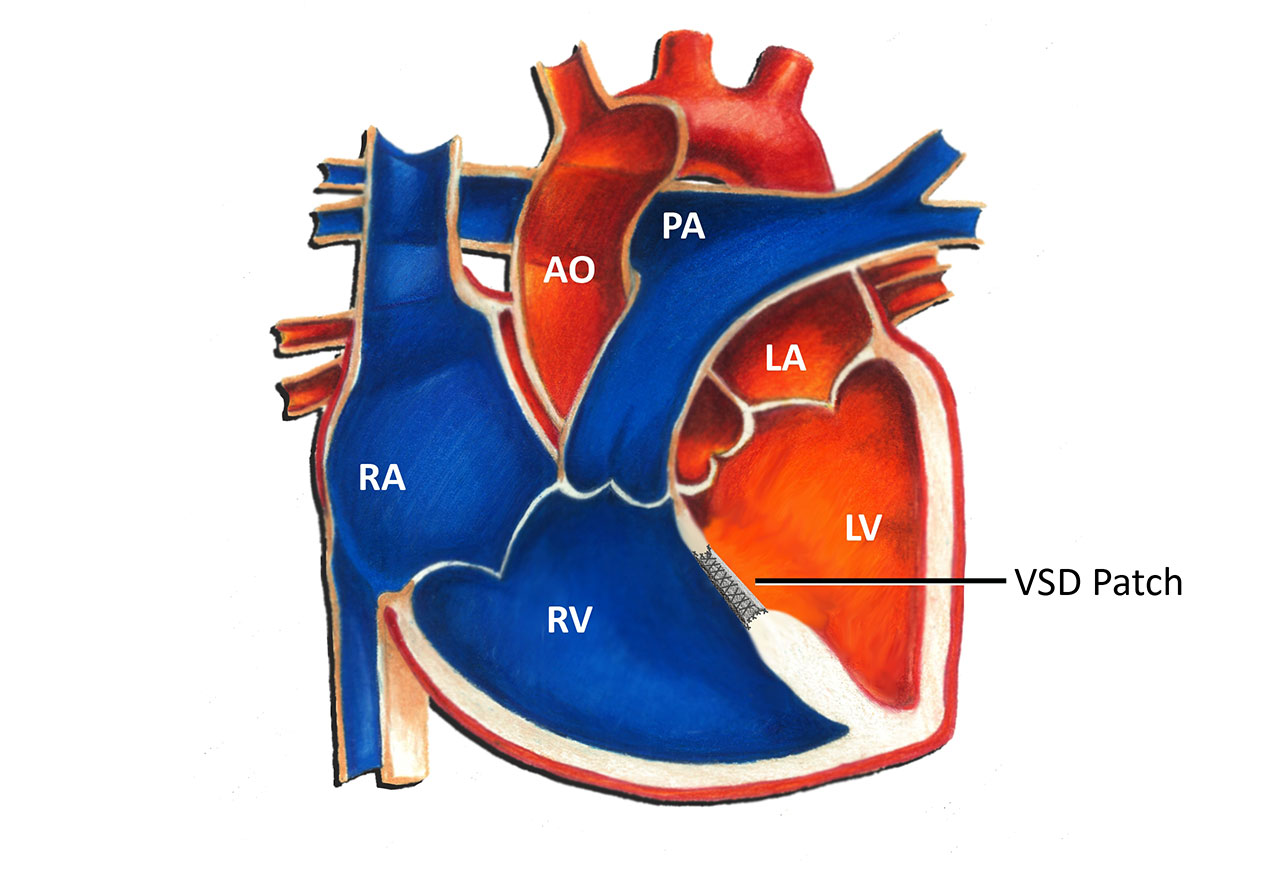
Ventricular Septal Defect (VSD) is a congenital heart defect that involves an abnormal opening or hole in the ventricular septum, the wall that divides the left and right ventricles of the heart. VSD is one of the most common congenital heart defects, and its severity can range from a small, asymptomatic hole to a large, life-threatening defect that requires immediate medical intervention. The condition causes an abnormal flow of blood between the two ventricles, potentially leading to a range of symptoms, including heart failure, pulmonary hypertension, and poor growth in children.
While some small VSDs close spontaneously over time, larger VSDs that do not close naturally typically require medical or surgical intervention, which can include VSD closure surgery or catheter-based closure techniques. Ventricular septal defect closures are performed to prevent complications like heart failure, arrhythmias, and stunted growth.
VSD closure procedures aim to close the hole, restore normal blood flow, and ensure that the heart functions efficiently. The procedure can be performed surgically or percutaneously (through a catheter), depending on the size of the VSD, the patient's age, and the presence of any other complications.
Causes and Risk Factors of VSD (Ventricular Septal Defect) Closures
Ventricular Septal Defect (VSD) is a congenital heart condition characterized by an abnormal hole in the septum, the wall separating the two lower chambers (ventricles) of the heart. This defect allows blood to flow between the ventricles, which can lead to various complications. While some VSDs close on their own as a child grows, others may require medical or surgical intervention. Here are the causes and risk factors that contribute to the development of VSDs and the closure of such defects:
1. Congenital Causes
Most VSDs are congenital, meaning they are present at birth due to abnormal heart development in the fetus. The precise cause of congenital VSDs remains unclear, but several factors contribute to their development:
-
Genetic Mutations: Abnormalities in genes that regulate heart development can cause VSDs. Chromosomal disorders such as Down syndrome, Turner syndrome, and DiGeorge syndrome often involve congenital heart defects, including VSDs.
-
Environmental Factors: Exposure to certain teratogens (agents that can cause birth defects) during pregnancy can increase the risk of congenital heart defects, including VSD. These factors include maternal diabetes, rubella infection, and the use of alcohol or drugs during pregnancy.
-
Familial Patterns: Family history can increase the risk of VSD. In some cases, inherited conditions like Marfan syndrome or Ehlers-Danlos syndrome may be linked to heart defects, including VSDs.
2. Maternal Health Conditions
Maternal health plays a significant role in the development of congenital heart defects. Some conditions that increase the risk of VSD include:
-
Diabetes: Maternal diabetes can cause disruptions in fetal heart development, leading to defects like VSD.
-
Infections: Infections such as rubella (German measles) during pregnancy can lead to birth defects, including heart problems.
-
Medications and Alcohol: Use of certain medications or alcohol during pregnancy can also increase the risk of congenital heart defects.
3. Prematurity
Premature infants have an increased likelihood of developing congenital heart defects, including VSDs. Preterm birth (before 37 weeks) is associated with an increased risk of various cardiovascular malformations, including VSD.
Symptoms and Signs of VSD (Ventricular Septal Defect) Closures
The symptoms of VSD vary depending on the size of the defect and the associated heart conditions. While some small VSDs may not cause any symptoms and may even close spontaneously, large VSDs can lead to significant complications. The following are the most common symptoms of VSD:
1. Heart Murmur
A heart murmur is the most common sign of a VSD, detected during a physical exam by a doctor using a stethoscope. The abnormal flow of blood through the VSD causes a turbulent sound that is heard as a murmur.
2. Shortness of Breath (Dyspnea)
One of the most common symptoms of VSD, especially in children, is shortness of breath during physical activity or even at rest. As blood flows inefficiently through the heart, the lungs may become congested with fluid, making breathing difficult.
3. Fatigue
Children with large VSDs often show signs of fatigue and weakness due to insufficient oxygenated blood being pumped to the body's tissues and organs. This often results in poor growth and developmental delays.
4. Swelling (Edema)
Swelling in the legs, feet, abdomen, and ankles can occur when the heart is unable to effectively pump blood, leading to fluid retention.
5. Frequent Respiratory Infections
Children with untreated VSD are at a higher risk of frequent respiratory infections due to fluid buildup in the lungs, which facilitates bacterial growth.
6. Cyanosis (Bluish Skin)
If a VSD is large and causes significant shunting of blood from the left ventricle to the right ventricle, it can result in a reduction in oxygen levels in the bloodstream. This condition, known as cyanosis, results in a bluish tint to the lips, fingers, and toes.
7. Failure to Thrive
Infants with large VSDs may experience poor feeding, delayed growth, and failure to thrive because the heart is not able to circulate blood efficiently to supply nutrients and oxygen.
Diagnosis of VSD (Ventricular Septal Defect) Closures
A Ventricular Septal Defect (VSD) is a congenital heart condition characterized by a hole in the septum (wall) that separates the heart’s two lower chambers (ventricles). The condition allows blood to flow between the ventricles, potentially leading to complications like increased lung blood flow, heart failure, or pulmonary hypertension.
1. Physical Examination
During a physical examination, doctors will listen to the heart for abnormal heart murmurs, which often signal the presence of a VSD. They will also assess symptoms like shortness of breath, fatigue, and swelling.
2. Echocardiogram (Ultrasound of the Heart)
An echocardiogram is the primary diagnostic tool for diagnosing a VSD. This test uses sound waves to produce real-time images of the heart, revealing the size, location, and severity of the VSD. The echocardiogram will also help assess blood flow through the heart and determine how much the VSD is affecting the heart's function.
3. Electrocardiogram (ECG)
An ECG measures the electrical activity of the heart and can detect arrhythmias that may result from a VSD or its complications.
4. Chest X-ray
A chest X-ray can be used to observe heart enlargement, fluid in the lungs, or other signs of heart failure caused by the VSD.
5. Cardiac Catheterization
In rare cases, a cardiac catheterization may be required to measure pressures inside the heart chambers and to visualize the defect. This is typically used for more complex or complicated cases of VSD.
6. MRI/CT Imaging
For complex VSDs or pre-surgical planning, cardiac MRI or CT scans may be used to obtain detailed images of the heart's anatomy.
Treatment Options for VSD (Ventricular Septal Defect) Closures
Ventricular Septal Defect (VSD) is a congenital heart condition where there is an abnormal hole in the wall (septum) that separates the two ventricles of the heart. This allows blood to flow from the left ventricle (which is under higher pressure) into the right ventricle, leading to abnormal blood flow and potential complications.
1. Observation for Small Defects
Many small VSDs that do not cause significant symptoms may close spontaneously within the first few years of life. These children will often be monitored with periodic echocardiograms to ensure that the defect does not lead to further complications.
2. Medications
While medications cannot close the VSD itself, they are often used to manage symptoms and reduce the burden on the heart:
-
Diuretics: Help reduce fluid buildup in the lungs and body.
-
Beta-blockers: To reduce the workload on the heart and control arrhythmias.
-
ACE inhibitors: To lower blood pressure and relieve stress on the heart.
3. Surgical VSD Closure
-
Open-heart surgery is the most common method for closing large VSDs. A patch or stitches are used to close the hole in the septum, restoring normal blood flow.
-
Minimally invasive surgery is a newer approach for some VSDs, where small incisions are made and robotic or catheter-based techniques are used to perform the procedure.
4. Percutaneous (Catheter-Based) Closure
For certain types of VSDs, a percutaneous procedure may be performed. In this method, a catheter is inserted through a vein (often through the groin), and a device is placed inside the VSD to close the hole. This approach is less invasive and has a shorter recovery time.
Prevention and Management of VSD (Ventricular Septal Defect) Closures
Ventricular Septal Defect (VSD) is a congenital heart condition where there is an abnormal opening in the septum that divides the left and right ventricles of the heart. This condition can lead to an imbalance in the flow of blood between the two chambers of the heart and may cause serious complications such as pulmonary hypertension or heart failure if left untreated.
1. Prenatal Care
-
Expectant mothers should ensure regular prenatal checkups and screenings to detect potential heart defects in the fetus.
-
Healthy pregnancy habits, such as proper nutrition, taking prenatal vitamins (including folic acid), avoiding smoking and alcohol, and managing pre-existing conditions like diabetes, can reduce the risk of congenital heart defects.
2. Lifestyle Modifications
Maintaining a healthy lifestyle is important for the long-term health of the heart:
-
Exercise: Regular physical activity helps strengthen the heart and improve overall cardiovascular health.
-
Healthy Eating: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains is beneficial for heart health.
-
Stress Management: Reducing stress and managing anxiety can have positive effects on heart function.
Complications of VSD (Ventricular Septal Defect) Closures
Complications of Ventricular Septal Defect (VSD) closures can vary depending on the method of treatment (surgical repair or device closure) and the patient's individual health status. Some potential complications include:
1. Surgical Complications
-
Infection: Risk of wound infections, endocarditis, and other surgical complications.
-
Bleeding: Discussion of bleeding risks during surgery and post-operative care.
-
Restenosis: The possibility that the VSD may reopen after surgical closure, particularly in larger defects.
2. Long-Term Risks
-
Arrhythmias: Increased risk of irregular heart rhythms (e.g., atrial fibrillation, ventricular arrhythmias) following surgery.
-
Heart Failure: How large VSDs left untreated can lead to heart failure, and the potential for heart failure to develop after surgery.
-
Prosthetic Valve Dysfunction: In cases where artificial valves are used, there may be risks of valve dysfunction and thrombosis.
Living with the Condition of VSD (Ventricular Septal Defect) Closures
Ventricular Septal Defect (VSD) is a heart condition where there is a hole in the wall (septum) that divides the two lower chambers of the heart, called ventricles. This hole allows blood to flow from the left ventricle to the right ventricle, disrupting the normal flow of blood in the heart. This condition can vary in severity, depending on the size of the hole and the amount of blood flowing through it.
1. Post-Surgery Recovery
After surgery, most patients experience a recovery period during which they are closely monitored for complications. Physical therapy and cardiac rehabilitation may be recommended to help regain strength and energy.
2. Long-Term Management
-
Regular Checkups: Follow-up appointments with the cardiologist will ensure that the heart continues to function properly.
-
Psychosocial Support: Children and adults living with VSD and undergoing surgery may face emotional challenges. Support from family, friends, and professionals is essential.
Top 10 Frequently Asked Questions about Ventricular Septal Defect (VSD) Closures
1. What is a Ventricular Septal Defect (VSD)?
A Ventricular Septal Defect (VSD) is a congenital heart condition where there is a hole in the septum (wall) that separates the left and right ventricles of the heart. This hole allows blood to flow between the two chambers, which can cause inefficient heart function, leading to symptoms like fatigue, heart murmurs, and in some cases, heart failure.
2. What are the symptoms of a VSD?
Symptoms of a VSD can vary depending on the size and location of the defect. Common signs and symptoms include:
-
Heart murmur (abnormal heart sound)
-
Fatigue or tiredness, especially during physical activity
-
Shortness of breath
-
Frequent respiratory infections
-
Poor growth in infants
-
Swelling in the legs, abdomen, or feet in severe cases
Larger defects can lead to more significant symptoms and complications, including heart failure.
3. How is a VSD diagnosed?
VSD is often diagnosed through:
-
Physical examination: A heart murmur may be detected by a doctor.
-
Echocardiogram (ultrasound of the heart): This is the most common and definitive test for diagnosing a VSD, providing detailed images of the heart's structure.
-
Electrocardiogram (EKG): To check the heart's electrical activity
-
Chest X-ray: To visualize the size of the heart and detect any enlargement or fluid buildup
-
Cardiac MRI or CT scan: In some cases for more detailed imaging
4. What is VSD closure surgery?
VSD closure surgery is a procedure used to close the hole in the ventricular septum, preventing abnormal blood flow between the heart's ventricles. The surgery can be performed using open-heart surgery or catheter-based techniques (for smaller defects). The goal is to restore normal heart function and prevent complications like heart failure or pulmonary hypertension.
5. When is VSD closure necessary?
VSD closure is usually necessary when:
-
Symptoms are present (such as difficulty breathing, fatigue, or poor growth)
-
The hole is large, causing significant blood flow issues
-
The VSD causes complications, such as pulmonary hypertension (high blood pressure in the lungs)
-
The defect does not close on its own or causes long-term damage to the heart or lungs
In some cases, smaller VSDs that do not cause significant issues may be monitored without immediate surgery.
6. How is VSD closure surgery performed?
There are two main types of VSD closure:
-
Open-heart surgery: The chest is opened, and the heart is temporarily stopped. The surgeon closes the VSD using sutures or a patch. This procedure is more common for larger defects.
-
Catheter-based closure: A minimally invasive technique where a catheter is inserted through a vein (usually in the groin) and guided to the heart. A device or plug is deployed to close the VSD without the need for open surgery. This is typically used for smaller, more accessible defects.
7. What are the risks and complications of VSD closure surgery?
Although VSD closure is generally safe, there are some risks, including:
-
Infection at the surgical site
-
Bleeding during or after surgery
-
Damage to heart valves or blood vessels
-
Arrhythmias (abnormal heart rhythms)
-
Heart failure in rare cases if the heart is not properly supported after the procedure
-
Failure of the closure (if the defect reopens)
Your cardiologist and surgeon will assess the risks based on the size and location of the VSD and the patient's overall health.
8. What is the recovery time after VSD closure surgery?
Recovery time varies depending on the type of surgery and the patient's overall health:
-
Open-heart surgery: Hospital stay is typically 5-7 days, with recovery taking 6-8 weeks for most patients.
-
Catheter-based closure: The procedure is minimally invasive, so patients may go home the same day or the following day, with recovery taking 1-2 weeks for most patients.
Full recovery may take 2-3 months, with regular follow-up appointments to monitor heart function.
9. Can a VSD reoccur after surgery?
In most cases, VSD closure surgery is successful, and the hole does not reopen. However, in rare cases, the defect may recur, particularly if the closure was not complete or if there were complications during the procedure. Regular follow-ups, including echocardiograms, are essential to monitor the repair and ensure the heart is functioning properly.
10. Can I live a normal life after VSD closure?
Yes, most patients can live a normal, healthy life after VSD closure surgery. After recovery, the heart will typically function normally, and the symptoms of the VSD (such as shortness of breath or fatigue) will significantly improve. However, lifestyle changes, such as avoiding strenuous activities in the early recovery period and attending regular check-ups, are important to ensure the continued health of the heart.


