Introduction to Coronary Angioplasty
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a medical procedure used to open narrowed or blocked coronary arteries — the blood vessels that supply blood to the heart muscle. This condition is typically caused by atherosclerosis, where plaque (fatty deposits) builds up inside the arteries, obstructing blood flow.
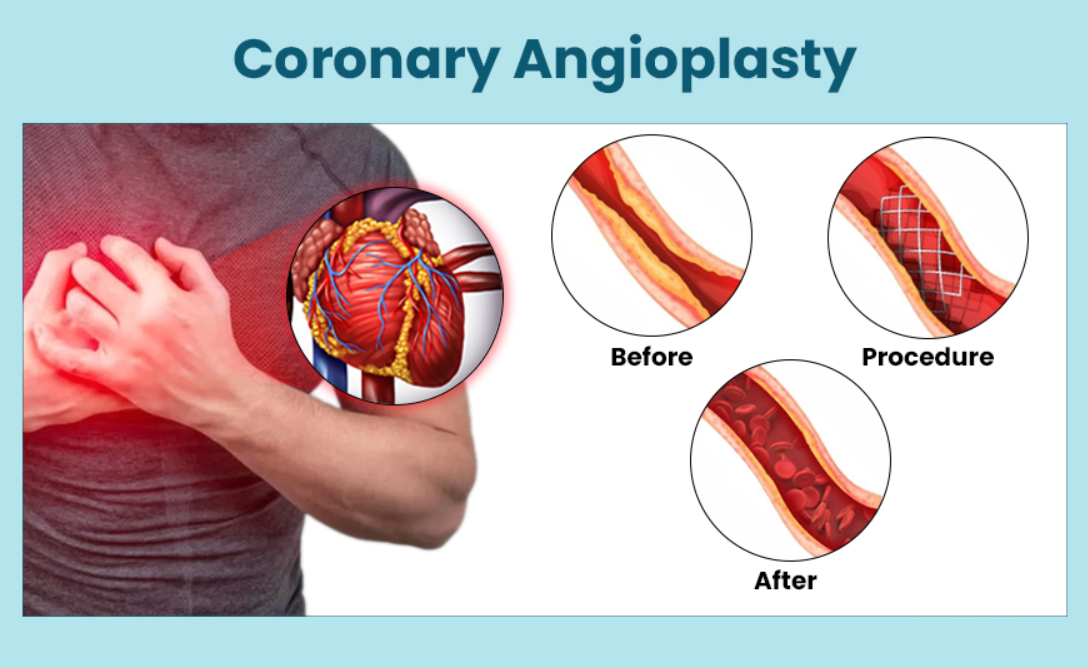
Angioplasty is a minimally invasive procedure that can be performed to relieve symptoms of coronary artery disease (CAD), such as chest pain (angina) and to prevent heart attacks. During the procedure, a balloon catheter is inserted into the affected artery to widen the artery and restore normal blood flow. Sometimes, a stent (a small mesh tube) is placed to keep the artery open.
Coronary angioplasty has revolutionized the treatment of heart disease and remains one of the most common procedures performed in modern cardiology. It can significantly improve a patient's quality of life by reducing symptoms and reducing the risk of future heart attacks.
Causes and Risk Factors of Coronary Angioplasty
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a medical procedure used to open narrowed or blocked coronary arteries, typically caused by atherosclerosis. While coronary angioplasty is an effective treatment for people with coronary artery disease (CAD), it's important to understand the causes and risk factors that contribute to the condition and the need for this intervention.
1. Atherosclerosis (Main Cause)
The most common cause of coronary artery blockages is atherosclerosis, a condition where plaque made up of fat, cholesterol, and other substances accumulates inside the arterial walls. This buildup narrows the arteries, restricting blood flow to the heart muscle and increasing the risk of heart attacks.
2. Risk Factors for Atherosclerosis
Several risk factors increase the likelihood of developing atherosclerosis and coronary artery disease:
-
High Blood Pressure (Hypertension): Increased blood pressure causes additional stress on the artery walls, contributing to plaque buildup.
-
High Cholesterol: Elevated LDL ("bad" cholesterol) levels increase plaque formation, while low HDL ("good" cholesterol) contributes to poor artery health.
-
Smoking: Smoking accelerates the process of atherosclerosis by damaging blood vessels and promoting the buildup of plaque.
-
Diabetes: High blood sugar levels promote the formation of plaque and increase the risk of CAD.
-
Obesity: Excess weight strains the heart, increases blood pressure, and worsens cholesterol levels, all of which contribute to the development of CAD.
-
Family History: Genetics play a significant role in an individual's risk of coronary artery disease.
-
Age: The risk of developing coronary artery disease increases with age, particularly after 45 for men and 55 for women.
-
Sedentary Lifestyle: Lack of physical activity contributes to many risk factors such as high blood pressure, cholesterol, and obesity.
-
Poor Diet: A diet high in unhealthy fats and low in fiber and nutrients increases the risk of plaque buildup.
Symptoms and Signs of Coronary Artery Disease
Coronary Artery Disease (CAD) is a condition where the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to a buildup of plaque (atherosclerosis). The symptoms and signs of CAD can vary, and in some cases, individuals may not experience any symptoms until the condition is advanced. Below are the common symptoms and signs:
1. Angina (Chest Pain)
-
Stable Angina: Occurs during physical exertion or stress and typically goes away with rest or medication.
-
Unstable Angina: A more severe and unpredictable form of chest pain that can occur at rest or with minimal exertion. It often signals an impending heart attack and requires immediate medical attention.
2. Shortness of Breath
When the heart does not receive adequate blood supply, it can result in shortness of breath during physical activity or even at rest.
3. Fatigue
Patients with reduced blood flow to the heart may feel unusual fatigue or weakness, especially after physical activity.
4. Palpitations
The sensation of a racing or irregular heartbeat can occur when the heart struggles to pump blood effectively.
5. Sweating and Dizziness
Excessive sweating and dizziness can also be signs of compromised heart function due to inadequate blood supply.
In some cases, people with coronary artery disease may not have any symptoms (this is referred to as silent ischemia), and they may only discover their condition when an angiogram is performed for other reasons.
Diagnosis of Coronary Angioplasty
Coronary angioplasty is a medical procedure used to treat narrowed or blocked coronary arteries, which can lead to coronary artery disease (CAD). The diagnosis of coronary angioplasty involves several diagnostic steps and tests to determine the extent and location of the blockages. Here's a detailed look at the diagnostic process:
1. Medical History and Physical Examination
Your doctor will start by asking about your symptoms, risk factors, and family history of heart disease.
2. Electrocardiogram (ECG)
An ECG records the heart's electrical activity and can show signs of a heart attack, arrhythmias, or insufficient blood flow.
3. Stress Testing
This test assesses the heart's ability to handle physical stress. It involves exercising on a treadmill or stationary bike while being monitored for heart rate and rhythm. If you're unable to exercise, medications that simulate exercise may be used.
4. Echocardiogram
An ultrasound of the heart, which provides detailed images of the heart's structure and function, can help detect blockages and other abnormalities.
5. Coronary Angiography
This is the primary diagnostic test used to confirm coronary artery disease and determine the need for angioplasty. A catheter is inserted into an artery, usually in the groin or wrist, and a contrast dye is injected to highlight the coronary arteries on an X-ray image.
6. CT or MRI Scans
These non-invasive imaging tests provide detailed pictures of the heart and blood vessels, offering information about plaque buildup and blood flow.
Treatment Options for Coronary Angioplasty
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a minimally invasive procedure used to open narrowed or blocked coronary arteries, restoring blood flow to the heart. While the angioplasty itself is the primary treatment, various adjunctive treatments and management strategies may be considered to optimize outcomes. Below are the main treatment options associated with coronary angioplasty:
1. Medications
Medications may be used to manage symptoms, reduce heart strain, and prevent plaque buildup. These include:
-
Antiplatelets (Aspirin, Clopidogrel): Help prevent blood clots from forming.
-
Statins: Lower cholesterol levels and reduce the risk of plaque buildup.
-
Beta-Blockers: Help lower blood pressure and heart rate, reducing heart strain.
-
ACE Inhibitors: Lower blood pressure and reduce heart workload.
-
Nitroglycerin: Helps relieve chest pain by relaxing blood vessels and improving blood flow.
2. Coronary Angioplasty (PCI)
Percutaneous coronary intervention (PCI), commonly known as coronary angioplasty, involves inflating a balloon inside the narrowed coronary artery to widen it. Sometimes, a stent (a tiny mesh tube) is placed to keep the artery open. This procedure is minimally invasive and significantly improves blood flow to the heart, relieving symptoms like chest pain.
3. Bypass Surgery (CABG)
In cases where angioplasty is not possible or if multiple arteries are blocked, coronary artery bypass grafting (CABG) surgery may be performed. This involves using a blood vessel from another part of the body to bypass the blocked artery, restoring blood flow to the heart.
Prevention and Management of Coronary Artery Disease
Coronary Artery Disease (CAD) is a condition in which the blood vessels supplying blood to the heart become narrowed or blocked, usually due to the build-up of fatty deposits (atherosclerosis). CAD is a leading cause of heart attacks, chest pain, and heart failure. However, it is largely preventable and manageable with early intervention, healthy lifestyle choices, and, if necessary, medical treatment.
1. Lifestyle Changes
-
Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Reduce salt, sugar, and processed foods.
-
Exercise: Regular physical activity strengthens the heart, improves circulation, and helps manage weight and blood pressure.
-
Smoking Cessation: Smoking accelerates atherosclerosis and increases the risk of heart disease.
-
Weight Management: Maintain a healthy weight to reduce strain on the heart.
-
Limit Alcohol Consumption: Excessive alcohol can raise blood pressure and contribute to other heart disease risk factors.
2. Medical Management
-
Regular Check-ups: Ensure regular monitoring of cholesterol, blood pressure, and blood sugar levels.
-
Medication Adherence: Take prescribed medications as directed to control blood pressure, cholesterol, and blood clotting.
Complications of Coronary Angioplasty
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a procedure used to open narrowed or blocked coronary arteries. While it is generally safe and effective, it does carry some risks and complications, which may include:
-
Restenosis: Re-narrowing of the artery after the procedure.
-
Blood Clots: Formation of clots inside the stent, which can lead to a heart attack.
-
Heart Attack: In rare cases, angioplasty can trigger a heart attack.
-
Bleeding: At the catheter insertion site (groin or wrist).
-
Infection: As with any surgical procedure, there is a risk of infection.
Living with the Condition of Coronary Artery Disease
After coronary angioplasty, many patients can return to a normal lifestyle with proper management:
-
Regular Follow-ups: To monitor heart health and check for any signs of restenosis.
-
Exercise: Once cleared by a doctor, exercise can help improve cardiovascular health.
-
Emotional Well-being: It is common for people who have undergone heart procedures to experience anxiety or depression. Support from loved ones and professional counseling may be helpful.
Adhering to a heart-healthy lifestyle is the key to living with coronary artery disease. With proper care, most patients with coronary artery disease and those who have undergone angioplasty can continue to lead active, fulfilling lives.
Top 10 Frequently Asked Questions about Coronary Angioplasty
1. What is coronary angioplasty?
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a medical procedure used to treat narrowed or blocked coronary arteries (the blood vessels that supply blood to the heart). During the procedure, a small balloon is inflated inside the blocked artery to widen it, often followed by the placement of a stent to keep the artery open.
2. Why is coronary angioplasty performed?
Coronary angioplasty is typically performed to:
-
Relieve symptoms of coronary artery disease, such as chest pain (angina)
-
Improve blood flow to the heart muscle
-
Prevent heart attacks by restoring adequate blood supply to areas of the heart affected by a blockage
The procedure is commonly recommended when lifestyle changes, medications, or other treatments have not been effective in managing heart disease.
3. How is coronary angioplasty performed?
The procedure is performed under local anesthesia and may involve:
-
Insertion of a catheter: A small tube is inserted into the artery (usually through the groin or wrist) and guided to the coronary arteries using X-ray guidance.
-
Balloon inflation: A small balloon at the end of the catheter is inflated at the site of the blockage to widen the artery.
-
Stent placement: A stent (a small mesh tube) may be placed in the artery to keep it open after the balloon is deflated and removed.
The procedure typically takes 30 minutes to 2 hours, depending on the complexity of the blockage.
4. What is a coronary stent?
A coronary stent is a small, mesh-like device inserted into the artery during angioplasty. Its purpose is to keep the artery open and prevent it from narrowing again. Stents are usually made of metal or a combination of metal and polymers and may be drug-eluting (coated with medication) to help prevent restenosis (re-narrowing) of the artery.
5. What are the risks of coronary angioplasty?
While coronary angioplasty is generally safe, it carries some risks, including:
-
Bleeding or infection at the catheter insertion site
-
Damage to blood vessels or the artery
-
Heart attack or arrhythmias (irregular heart rhythms) during the procedure
-
Restenosis: Re-narrowing of the artery, even after stenting
-
Kidney damage (rare, especially from the contrast dye used during the procedure)
Your cardiologist will discuss these risks and take steps to minimize complications during the procedure.
6. What is the recovery time after coronary angioplasty?
The recovery time varies depending on the individual, but most people can return home the same day or the following day after the procedure.
-
Immediate recovery: You may need to rest for a few hours after the procedure to allow the catheter insertion site to heal.
-
Resuming normal activities: Most people can return to normal activities within 1 to 2 weeks, but heavy lifting or strenuous physical activities should be avoided for about 4 to 6 weeks.
Follow-up appointments are usually scheduled to monitor progress and ensure proper healing.
7. How long does a coronary stent last?
Coronary stents are designed to last a long time, often many years. Drug-eluting stents, which are coated with medication to prevent restenosis, have a success rate of 80-90% in keeping the artery open. However, some patients may experience re-narrowing (restenosis), which may require further intervention. Regular follow-up appointments are necessary to monitor the stent and heart health.
8. What lifestyle changes should I make after coronary angioplasty?
After angioplasty, it is important to make lifestyle changes to improve heart health and prevent further blockages:
-
Adopt a heart-healthy diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
-
Exercise regularly: Aim for at least 30 minutes of moderate exercise on most days, as recommended by your healthcare provider.
-
Quit smoking: Smoking cessation is crucial for heart health.
-
Control blood pressure, cholesterol, and diabetes: Manage any existing conditions with medication, lifestyle changes, or both.
-
Reduce stress: Practice relaxation techniques and manage stress effectively.
Following these changes helps improve overall heart health and reduces the risk of future heart problems.
9. How soon can I resume normal activities after coronary angioplasty?
Most patients can resume light activities within 1-2 weeks. However, it is recommended to avoid heavy lifting, vigorous exercise, and any activity that puts undue stress on the body for at least 4-6 weeks after the procedure. Your doctor will provide guidelines based on your individual recovery and health status.
10. Can coronary angioplasty completely cure heart disease?
While coronary angioplasty can effectively treat the symptoms of coronary artery disease by improving blood flow to the heart, it does not cure the underlying condition. Ongoing management, including lifestyle changes, medications, and regular check-ups, is essential to prevent further blockages and reduce the risk of future heart problems. Coronary angioplasty may also need to be repeated in some cases if restenosis occurs.


