Introduction to Adam's Apple Reshaping
Adam's Apple reshaping, also known as Chondrolaryngoplasty or Tracheal Shaving, is a surgical procedure performed to reduce the prominence of the thyroid cartilage (known as the Adam's Apple), typically to create a smoother, more feminine neck contour. The procedure is often sought after by transgender women undergoing gender-affirming surgeries, but it is also a cosmetic choice for those wishing to alter the appearance of their neck, whether they are cisgender men, women, or individuals in the early stages of gender transition.
What is Adam's Apple Reshaping?
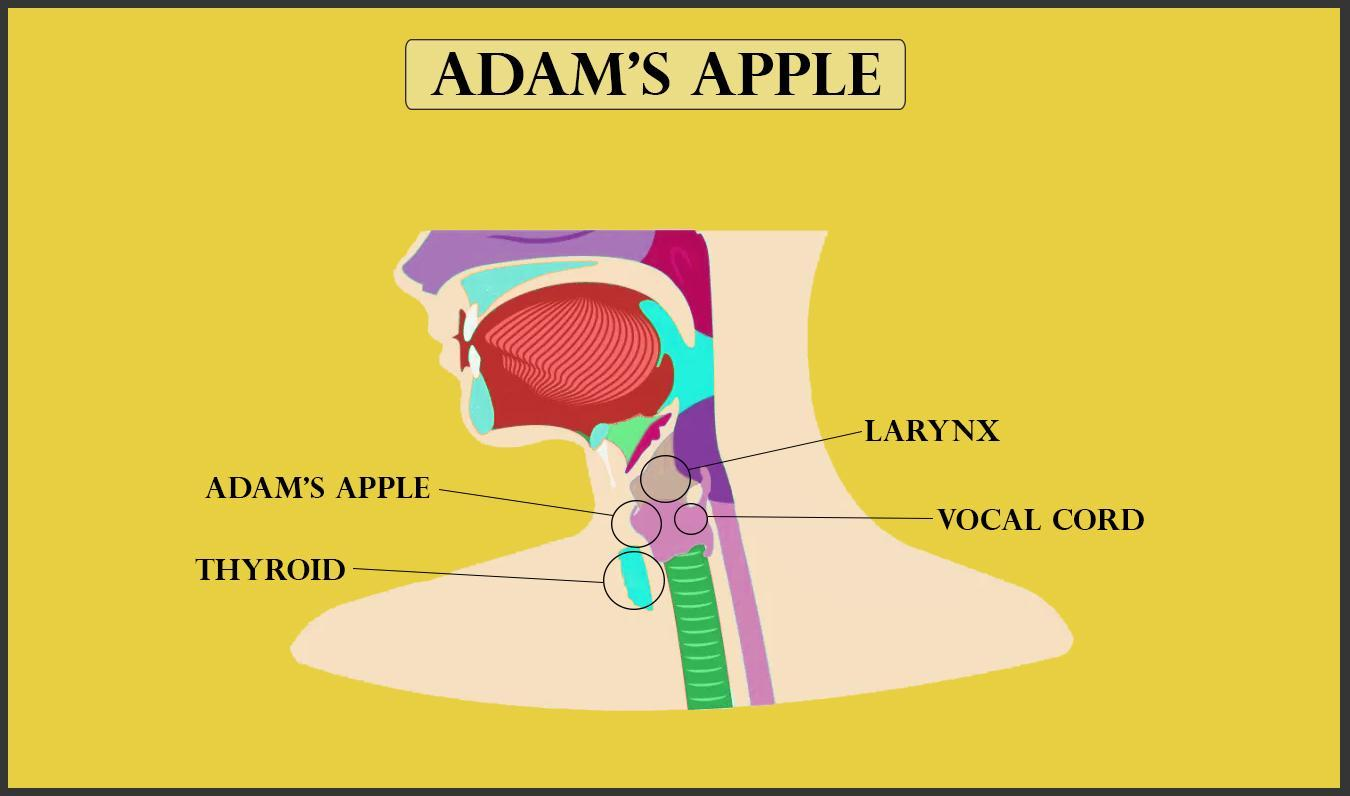
The Adam's Apple is the visible bump at the front of the neck formed by the thyroid cartilage that protects the vocal cords. This prominence is typically more noticeable in men, due to the increased size of the cartilage during puberty under the influence of testosterone. While it serves a functional role in protecting the airway, many individuals desire to reduce its size for cosmetic reasons or as part of gender affirmation surgery.
Adam's Apple reshaping involves shaving down or reshaping the thyroid cartilage, reducing its prominence while maintaining the overall function of the larynx and voice box. The surgery typically involves small, inconspicuous incisions, and it can be done under local anesthesia or general anesthesia, depending on the complexity and patient's preferences.
Why Choose Adam's Apple Reshaping?
-
Aesthetic Goals: Many individuals feel self-conscious about the size or shape of their Adam's Apple. This procedure allows for a smoother neck appearance, contributing to a more feminine neck contour for those desiring a more balanced facial profile.
-
Transgender Women's Surgery: Adam's Apple reshaping is a common part of gender-affirming surgery for transgender women, helping them align their physical appearance with their gender identity.
-
Post-Puberty Change: For cisgender men or women, a large Adam's Apple might be a source of discomfort or distress. In such cases, reshaping helps restore a more natural and symmetrical neck appearance.
In the following sections, we will delve deeper into the causes, risks, diagnosis, and treatment options related to Adam's Apple reshaping.
Causes and Risk Factors for Adam's Apple Prominence
A prominent Adam's apple is most often a normal anatomical feature-especially in men-but in some cases, it may appear enlarged due to underlying medical conditions, particularly thyroid enlargement (goiter) or nodular growths beneath the larynx. The thyroid gland sits directly under the Adam's apple, so its swelling can give the appearance of an increased prominence in this area.
What Causes a Prominent Adam's Apple?
The prominence of the Adam's Apple is primarily a result of the thyroid cartilage becoming more prominent during puberty, particularly in males due to higher testosterone levels. The growth of this cartilage is influenced by hormonal changes that occur during sexual maturation.
-
Hormonal Influence:
-
In men, testosterone causes the thyroid cartilage to grow significantly, forming the Adam's Apple. This is why men typically have a more visible bump in the neck.
-
In women, estrogen keeps the thyroid cartilage from becoming as prominent. As a result, women generally have a smoother neck with less visible cartilage.
-
-
Genetic Factors:
-
Genetics play a role in determining how much thyroid cartilage will develop. Some individuals may inherit a more pronounced laryngeal prominence due to their family genetics, regardless of sex.
-
-
Gender Dysphoria (Transgender Women):
-
For transgender women, gender dysphoria related to having a masculine or overly visible Adam's Apple can lead to a desire for reshaping as part of gender-affirming surgery.
-
Transgender women, who undergo hormone replacement therapy (HRT), may experience some reduction in the size of their Adam's Apple over time. However, if this is insufficient for their aesthetic goals, they often opt for surgical reshaping.
-
-
Age and Puberty:
-
As people age, skin laxity can make the Adam's Apple appear more prominent. In some cases, even a modestly sized laryngeal prominence can seem more noticeable with the natural effects of aging.
-
-
Trauma or Surgery:
-
Injury to the neck or past surgeries can lead to changes in the appearance of the Adam's Apple, either increasing or decreasing its prominence.
-
Symptoms and Signs of a Prominent Adam's Apple
A prominent Adam's apple, or laryngeal prominence, is typically a normal anatomical feature that is more visible in males due to puberty-related growth of the larynx. However, certain symptoms and signs can arise when the Adam's apple or surrounding structures are affected, indicating underlying conditions.
Common Symptoms Leading to Adam's Apple Reshaping
The decision to undergo Adam's Apple reshaping is often driven by personal dissatisfaction with the appearance of the neck, which can cause emotional and psychological distress. The symptoms are not typically medical but rather aesthetic concerns:
-
Visible Protrusion:
-
The most obvious symptom is a large, visible Adam's Apple, which can be self-consciousness-inducing, especially in women or transgender individuals.
-
Some people may feel their Adam's Apple is disproportionately large compared to their facial features, contributing to a sense of masculine appearance.
-
-
Psychosocial Effects:
-
A prominent Adam's Apple can be a source of psychological distress, social anxiety, or body image concerns, especially in individuals who feel uncomfortable with their neck's appearance.
-
For transgender women, this can be a source of gender dysphoria, where the discordance between their physical appearance and gender identity is accentuated by the prominence of the thyroid cartilage.
-
-
Physical Discomfort (Less Common):
-
In rare cases, an unusually large Adam's Apple might cause some physical discomfort, particularly when swallowing or during certain physical activities. However, discomfort is not a major factor in most cases.
-
When Should You Consider Surgery?
Surgery is typically considered when the psychological distress or aesthetic discomfort outweighs the risk of complications or recovery time. Individuals may seek surgery to:
-
Achieve a more feminine neck profile.
-
Align physical features with gender identity for transgender women.
-
Alleviate feelings of self-consciousness or social anxiety.
-
Achieve facial balance and harmony.
Diagnosis of Adam's Apple Reshaving
Diagnosis and pre-operative assessment before Adam's apple reshaping surgery (tracheal shave or chondrolaryngoplasty) are focused on evaluating patient motivations, anatomical suitability, surgical risk, and voice safety. Here's the typical workup for those considering Adam's apple reduction:
Preoperative Consultation and Evaluation
Before undergoing Adam's Apple reshaping, it is critical to undergo a thorough preoperative evaluation with a qualified plastic or facial surgeon who specializes in aesthetic neck surgeries.
-
Medical History:
-
The surgeon will take a comprehensive medical history, asking about previous surgeries, medical conditions (e.g., thyroid issues), and medications (especially blood thinners or hormones).
-
-
Neck Examination:
-
A physical examination of the neck is essential to evaluate the size and shape of the Adam's Apple and to understand the amount of reshaping needed.
-
The surgeon will also assess skin elasticity and the general condition of the neck to determine if there are any underlying conditions that may affect the outcome.
-
-
Voice Assessment:
-
If the procedure is being performed as part of gender-affirming surgery, a speech therapist or laryngologist may be consulted to assess baseline voice quality and to discuss potential risks to vocal cords post-surgery.
-
Voice assessment helps determine any potential risks to speech or vocal functionality due to nerve damage or cartilage manipulation.
-
-
Imaging:
-
In some cases, ultrasound or MRI scans may be used to assess the size and shape of the thyroid cartilage more accurately, helping surgeons plan for the procedure. This imaging is especially important if there is any suspicion of thyroid-related issues.
-
-
Psychological Evaluation:
-
For individuals undergoing surgery as part of gender-affirming care, a psychological evaluation may be conducted to ensure that the individual is ready for the physical and emotional impact of surgery and recovery.
-
Treatment Options for Adam's Apple Reshaping
The primary treatment for reshaping a prominent Adam's apple is a surgical procedure called a tracheal shave, or chondrolaryngoplasty. Non-surgical options have limited efficacy and are only cosmetic (e.g., makeup, changes in neck posture), while surgical approaches directly reduce the size of the thyroid cartilage for a smoother and less prominent neck profile.
Traditional Adam's Apple Reshaping (Chondrolaryngoplasty)
The main surgical goal of Adam's Apple reshaping is to reduce the size of the thyroid cartilage while maintaining normal laryngeal function. The procedure involves shaving down or reshaping the thyroid cartilage, particularly the visible portion that forms the Adam's Apple.
-
Incision Placement:
-
A small horizontal incision is typically made under the chin or at the base of the neck, in an inconspicuous location to minimize scarring.
-
-
Cartilage Shaving:
-
Using specialized instruments, the surgeon shaves down the thyroid cartilage. This may involve sculpting the cartilage to achieve the desired level of prominence, usually reducing the protrusion while leaving the surrounding laryngeal structures intact.
-
-
Suture and Closure:
-
After reshaping the cartilage, the incision is carefully sutured. The procedure typically lasts 1-2 hours, and recovery time varies depending on the individual's health and the complexity of the surgery.
-
-
Anesthesia Options:
-
The surgery can be performed under local anesthesia with sedation, though general anesthesia is often preferred for complete comfort during the procedure.
-
Minimally Invasive Techniques
In some cases, minimally invasive techniques such as endoscopic or robotic-assisted surgery are used for Adam's Apple reshaping. These methods utilize smaller incisions and provide better precision and quicker recovery.
-
Endoscopic Surgery:
-
Using a camera and specialized tools, the surgeon can shave the thyroid cartilage through small incisions made behind the ear or at the base of the neck.
-
-
Robotic Surgery:
-
Robotic-assisted surgery offers greater precision and better visualization of the neck structures, especially for delicate areas like the vocal cords.
-
Combined Gender-Affirming Surgery
For transgender women, Adam's Apple reshaping is often part of a broader package of gender-affirming surgeries. These surgeries may also include facial feminization, breast augmentation, or vocal cord surgeries to create a cohesive feminine appearance.
Prevention and Management of Adam's Apple Prominence
While it is not possible to prevent the natural development of the Adam's Apple, especially during puberty, there are various management techniques to cope with its appearance.
Preoperative Counseling and Psychological Support
-
Psychological Counseling:
-
If the surgery is part of gender-affirming care, psychological counseling helps patients prepare emotionally for the surgery, recovery, and long-term lifestyle changes.
-
-
Voice Therapy:
-
In some cases, voice therapy with a speech-language pathologist can help transgender individuals improve their voice quality before and after the surgery, as vocal changes may occur postoperatively.
-
Managing Recovery and Aftercare
-
Postoperative Care:
-
After surgery, the patient will be monitored in a recovery room before being discharged. Swelling and discomfort are common but manageable with pain medications and ice packs.
-
-
Avoiding Strain:
-
Patients should avoid straining their neck for a few weeks post-surgery. This includes avoiding lifting heavy objects, bending over for extended periods, and excessive talking.
-
-
Follow-up Appointments:
-
Follow-up appointments are crucial to monitor the healing process, remove sutures, and ensure there are no complications, such as infection or wound issues.
-
Complications of Adam's Apple Reshaving
Though chondrolaryngoplasty is considered relatively safe when performed by experienced surgeons, there are potential complications. Awareness and patient counseling are essential. Some risks are transient; others may be long-term.
Common / relatively mild complications
-
Transient hoarseness / voice weakness
Mild voice changes (hoarseness, fatigue) are among the most commonly reported postoperatively; often temporary and resolve with time and voice rest. -
Odynophagia / mild throat pain / swallowing discomfort
Discomfort in swallowing or throat soreness is common in the early postoperative period. -
Swelling, edema, bruising
Local swelling and bruising are expected; generally subside over days to weeks. -
Scar issues (hypertrophic scars, hyperpigmentation, visible scar)
Although surgeons aim to hide the incision in neck creases, some patients may develop thicker or more visible scars. Scar management therapies may be needed. -
Minor cartilage irregularities / asymmetry
Uneven shaving or healing can lead to contour irregularities, requiring revision or smoothing.
Less common / serious complications
-
Permanent or lasting voice change / vocal cord injury
If the procedure injures the anterior commissure, vocal fold attachment, or nerve supply, permanent changes in pitch, strength, or quality may occur.
Some studies have documented acoustic changes or vocal complications post-chondrolaryngoplasty.
Patients in online forums report occasional voice deterioration or loss of falsetto range. > "The risk is significant … losing notes off the top of your falsetto." -
Laryngeal / cartilage fracture
If too much cartilage is removed or if cartilage is brittle (e.g. ossified), structural compromise or fracture can occur. This is rare but serious, sometimes requiring reconstruction (e.g. plating). -
Hematoma / bleeding
Bleeding under the skin (hematoma) is a possible risk, especially in early postoperative period. A large hematoma may compress airway and require urgent drainage. -
Infection / cartilage chondritis
Superficial wound infection is possible; deeper infection involving cartilage (chondritis) is rare but serious. -
Airway compromise / breathing issues
If edema, hematoma or structural injury impinges on airway, breathing difficulties may arise (rare). -
Unmet aesthetic expectations / residual prominence
In some patients (~20%), the residual prominence is still visible, especially if vocal cords insert at a higher point or because cartilage removal was conservative for safety.
In the literature, complications are described as uncommon and mostly mild, but vigilance and careful technique are essential.
Living with the Condition / Postoperative Expectations Quality of Life
Because "Adam's apple prominence" is not a disease but an aesthetic attribute, "living with the condition" after reshaping mostly concerns recovery, voice adaptation, patient satisfaction, and lifestyle changes.
Recovery timeline & what to expect
-
First 1-2 days
Throat soreness, mild throat pain, swallowing discomfort, swelling, mild hoarseness (often from intubation) are common. -
First week
Incision site healing begins, some swelling and bruising decline, voice rest is emphasized. -
Weeks 2-4
Swelling continues to reduce, patients may begin gentle voice use, resume light activity, scar starts maturing. -
3-6 months
Final neck contour becomes more evident; scar color and appearance gradually settle; voice generally stabilizes; further adjustments may be considered. -
1 year and beyond
Scar fully matures; long-term cosmetic result and voice outcomes are clearer.
Voice & vocal adaptation
-
Most patients experience temporary voice changes, but many recover baseline voice quality if surgery is done carefully.
-
For those who do notice persistent mild changes (pitch, strength, range), voice therapy / speech therapy may help optimize outcomes.
-
Singers or voice professionals should be counselled preoperatively about risk to vocal performance-even when low in probability.
Patient satisfaction & psychosocial outcomes
-
Many patients report high satisfaction, improved confidence, and alignment with gender identity or aesthetic goals.
-
Some dissatisfaction arises from residual bump, visible scar, or subtle asymmetries-but revision surgery is an option.
-
It's important to manage expectations: complete "flatness" is rarely achievable; safety dictates preserving structural integrity.
Long-term care & monitoring
-
Observe for any late-onset complications (scar thickening, dysphonia, discomfort).
-
Scar management over years (sun protection, silicone, laser, etc.).
-
If revision is needed, assess timing, cartilage status, and possible increased risks from prior surgery.
Top 10 Frequently Asked Questions about Adam's Apple Reshaping/Reshaping
1. What is Adam's Apple Reshaping (Chondrolaryngoplasty)?
Adam's Apple Reshaping, medically called Chondrolaryngoplasty, is a
cosmetic surgical procedure aimed at reducing the size or prominence of the
Adam's apple. The Adam's apple is formed by the thyroid cartilage in the
neck, and it is often more prominent in males.
The procedure involves carefully shaving or reducing the cartilage to
achieve a smoother neck contour, while protecting the vocal cords and voice function. It
is commonly sought by transgender women, gender-nonconforming
individuals, or anyone who wishes to reduce the prominence for aesthetic
reasons.
2. Who is a suitable candidate for Adam's Apple Reshaping?
Ideal candidates include:
-
Individuals who feel self-conscious about a prominent Adam's apple.
-
Transgender women or non-binary individuals undergoing facial feminization procedures.
-
Adults with fully developed thyroid cartilage (typically 18 years and older).
-
Individuals in good general health with no major medical conditions that could interfere with healing.
Candidates should have realistic expectations about the results and understand the potential risks.
3. How is Adam's Apple Reshaping surgery performed?
The surgery is usually performed under general or local anesthesia with sedation. The steps include:
-
A small incision is made under the chin or at the base of the neck.
-
The thyroid cartilage is carefully exposed.
-
The surgeon shaves or trims the cartilage to reduce the prominence of the Adam's apple.
-
The incision is closed with fine sutures, often leaving a minimal or hidden scar.
The procedure generally takes 1-2 hours, depending on the technique and individual anatomy.
4. Will the surgery affect my voice?
The thyroid cartilage is located near the vocal cords, so surgeons take special care to preserve voice function.
-
If performed by a qualified surgeon, the risk of voice changes is minimal.
-
Temporary hoarseness or mild voice changes may occur immediately after surgery due to swelling but typically resolve within a few weeks.
-
Patients are usually advised to avoid straining the voice during recovery to ensure proper healing.
5. Is Adam's Apple Reshaping surgery painful?
Pain is usually mild to moderate after the procedure and can be managed with prescribed pain medications.
-
Most patients report discomfort primarily in the neck and throat area for a few days.
-
Swelling and bruising are common during the first 1-2 weeks.
-
Most individuals can resume normal activities within 1-2 weeks, though strenuous activity should be avoided for 3-4 weeks.
6. What is the recovery process after Adam's Apple Reshaping?
Recovery typically involves:
-
First few days: Rest, limited talking, and pain management.
-
1-2 weeks: Sutures are removed or dissolve; swelling and bruising gradually decrease.
-
3-4 weeks: Most patients return to normal daily activities.
-
1-2 months: Neck contour settles, and final results become noticeable.
Patients are advised to avoid strenuous activity or heavy lifting for several weeks and follow all post-operative instructions for optimal results.
7. Are there any risks or complications associated with Adam's Apple Reshaping?
While the procedure is generally safe, potential risks include:
-
Minor infection at the incision site.
-
Scarring, which is usually minimal or hidden.
-
Temporary swelling or bruising.
-
Rarely, voice changes if the vocal cords are affected.
-
Rare asymmetry or under/over correction of cartilage.
Choosing a board-certified surgeon experienced in chondrolaryngoplasty reduces these risks significantly.
8. How long does the Adam's Apple Reshaping surgery take?
The procedure typically takes 1 to 2 hours, depending on:
-
The prominence of the Adam's apple.
-
Whether it is combined with other procedures, such as facial feminization surgery.
-
The individual anatomy and surgical approach used (open vs minimally invasive).
Patients are usually able to go home the same day as surgery if performed on an outpatient basis.
9. When will I see the final results?
-
Initial results are visible immediately after the surgery, but swelling and bruising may obscure the final contour.
-
Most swelling resolves within 2-4 weeks, and the neck takes on a smoother, more natural contour.
-
Full healing and final aesthetic results may take 1-3 months, depending on individual healing and cartilage response.
-
Scars generally fade over time and can often be hidden in natural skin creases.
10. Is Adam's Apple Reshaping a permanent procedure?
Yes, the reduction of thyroid cartilage is permanent. Once the cartilage is reshaped, it does not grow back.
-
However, aging or weight changes can subtly affect neck appearance over time.
-
If performed with precision, the results are long-lasting and significantly improve the appearance of the neck for patients who wish to reduce a prominent Adam's apple.


