Introduction to Adrenalectomy
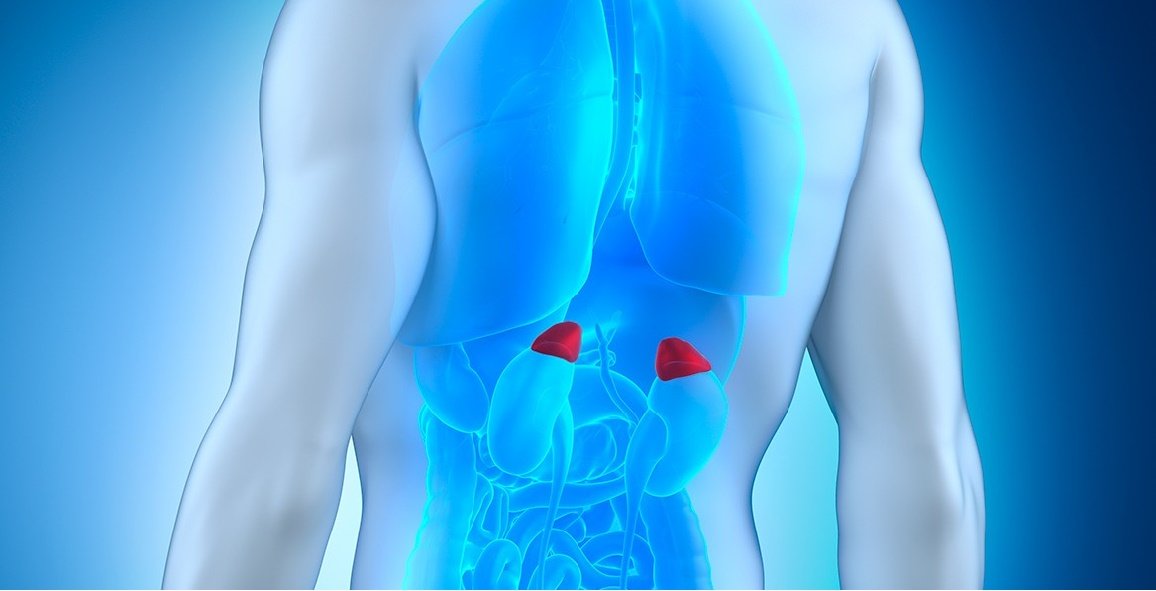
The adrenal glands, located on top of each kidney, are small but powerful organs responsible for producing critical hormones like cortisol, aldosterone, adrenaline, and sex steroids. These hormones regulate functions such as metabolism, blood pressure, stress response, and fluid balance in the body.
Adrenalectomy is the surgical removal of one (unilateral) or both (bilateral) adrenal glands. This procedure is typically performed when an adrenal gland is diseased, often due to a tumor that is producing excess hormones or has potential for malignancy. In some cases, a partial adrenalectomy may be performed, where only part of the gland is removed, to preserve some adrenal function.
Adrenalectomy can be a lifesaving surgery, especially in cases of hormone-secreting tumors such as pheochromocytoma, Cushing's syndrome, or primary hyperaldosteronism. The procedure is increasingly performed using minimally invasive techniques such as laparoscopy or robot-assisted surgery, offering quicker recovery times and reduced complications compared to traditional open surgery.
In this article, we will explore the causes, indications, symptoms, diagnosis, treatment options, complications, and life after adrenalectomy.
Causes and Indications / Risks of Adrenalectomy
Adrenalectomy, the surgical removal of one or both adrenal glands, is indicated primarily for adrenal tumors or disorders causing hormone imbalances. The surgery can be performed laparoscopically or as open surgery depending on tumor size, malignancy suspicion, and patient factors. It carries risks similar to other major surgeries, alongside adrenal-specific complications.
Causes and Indications for Adrenalectomy
Adrenalectomy is generally performed when there is a medical necessity to remove an adrenal tumor. Here are the common reasons for adrenalectomy:
-
Functional Adrenal Tumors
-
Pheochromocytoma: A tumor in the adrenal medulla that secretes excess catecholamines (epinephrine and norepinephrine), leading to episodes of high blood pressure, palpitations, headaches, sweating, and anxiety.
-
Cushing Syndrome (Hypercortisolism): Caused by an adrenal tumor or adrenal hyperplasia that produces excess cortisol, leading to weight gain, high blood pressure, osteoporosis, diabetes, and immunosuppression.
-
Primary Hyperaldosteronism (Conn's Syndrome): A tumor in the adrenal gland that produces excess aldosterone, leading to hypertension, low potassium, and fluid retention.
-
Adrenal Tumors Producing Sex Hormones: These tumors produce excessive androgens or estrogens, causing virilization or feminization symptoms.
-
-
Nonfunctional Tumors (with malignancy risk)
-
Some adrenal tumors, even if they are not hormonally active, may be large or show characteristics suggestive of malignancy. In such cases, removal is necessary, especially if the tumor exceeds certain size thresholds or shows irregular features.
-
-
Metastatic Adrenal Disease
-
Tumors that have spread from other organs, such as the kidneys or lungs, to the adrenal glands may require removal if they are isolated and manageable surgically.
-
-
Large Benign Masses
-
Benign adrenal tumors such as myelolipomas or adrenal cysts may need to be removed if they are large or causing symptoms like pain, discomfort, or mass effect.
-
-
Bilateral Adrenal Disease
-
In some conditions like bilateral adrenal hyperplasia or certain genetic disorders, both adrenal glands may need to be removed, leading to a lifelong need for hormone replacement therapy.
-
Risks and Considerations
Adrenalectomy is a relatively safe surgery, but like any surgery, it carries risks:
-
Complications from anesthesia: Rare but can include adverse reactions to anesthesia or issues during recovery.
-
Infection: Though uncommon, infections at the surgical site can occur.
-
Bleeding: There is always a risk of bleeding during surgery, especially if the tumor is vascular.
-
Hormonal Imbalance: Removal of the adrenal glands, particularly both, leads to adrenal insufficiency and requires lifelong hormone replacement therapy.
-
Damage to surrounding structures: The adrenal glands are located close to important structures like the kidneys, major blood vessels, and diaphragm, so there is a risk of injury to these areas during surgery.
-
Scar tissue formation: Especially after open surgery, scarring in the abdominal or retroperitoneal area can cause problems during recovery or future surgeries.
Symptoms and Signs of Adrenal Disease Leading to Adrenalectomy
Adrenal diseases that lead to adrenalectomy commonly involve hormone-secreting tumors or growths of the adrenal glands. These conditions can produce distinctive clinical signs depending on which hormone is being overproduced or underproduced.
Common Disorders Requiring Adrenalectomy
- Pheochromocytoma: Tumor producing excess catecholamines (adrenaline, noradrenaline).
- Symptoms: Severe headaches, palpitations, sweating, high blood pressure, anxiety, tremors, and panic attacks.
- Cushing's Syndrome (Hypercortisolism): Excess cortisol production from adrenal or pituitary sources.
- Symptoms: Weight gain (especially around the trunk), round/moon-shaped face, muscle weakness, purple stretch marks, hypertension, diabetes, mood changes, and osteoporosis.
- Primary Hyperaldosteronism (Conn's Syndrome): Overproduction of aldosterone causing salt and fluid imbalance.
- Symptoms: Hypertension resistant to treatment, low potassium (hypokalemia), frequent urination, muscle cramps, fatigue, and heart palpitations.
- Adrenocortical Carcinoma: Malignant tumor that may cause hormone excess or local mass effect.
- Symptoms: Abdominal/flank pain, weight changes, virilization (excess hair, acne), gynecomastia, menstrual irregularities, and abdominal enlargement.
- Adrenal Adenoma (Benign Tumor): May produce cortisol or aldosterone, or be nonfunctioning.
- Symptoms: High blood pressure, weight gain, and metabolic disturbances; some are asymptomatic.
Adrenal Insufficiency After Bilateral Removal
If both glands are affected and removed, adrenal insufficiency can occur.
Symptoms: Fatigue, weight loss, muscle weakness, low blood pressure, darkened skin, nausea, and electrolyte disturbances due to reduced cortisol and aldosterone production.
Diagnostic Steps for Adrenalectomy
Diagnostic steps for adrenalectomy involve a comprehensive combination of lab, imaging, and clinical evaluations to confirm adrenal disease, assess functional status, exclude other causes, and prepare for surgery. The process aims to identify hormone-secreting tumors, malignancy risk, and optimize patient safety.
-
Hormonal Tests:
-
To assess the function of the adrenal glands, patients may undergo blood tests to measure hormone levels:
-
Cortisol levels (including a dexamethasone suppression test)
-
Aldosterone and renin levels (for hyperaldosteronism)
-
Catecholamine levels (plasma metanephrines for pheochromocytoma)
-
DHEA, androgens, and estrogens (for sex hormone-secreting tumors)
-
-
-
Imaging:
-
CT or MRI scans are used to evaluate the size, shape, and characteristics of the adrenal tumor. These scans help differentiate benign from malignant lesions and assess for invasion into nearby tissues.
-
Adrenal vein sampling: Used to determine if one adrenal gland is producing excess hormones (e.g., for hyperaldosteronism).
-
Nuclear scans: In cases of pheochromocytoma or metastatic lesions, specific scans like MIBG or PET scans may be used.
-
-
Preoperative Assessment:
-
A thorough physical exam and medical history review are performed to assess general health and surgical risks.
-
Cardiovascular assessment is critical, especially for patients with pheochromocytoma or Cushing syndrome, which can affect heart function and blood pressure.
-
Patients will need to stop certain medications (such as blood thinners) before surgery.
-
Treatment Options for Adrenalectomy (Surgical Approaches)
Treatment options for adrenalectomy include several surgical approaches, with the choice dictated by tumor size, malignancy risk, anatomical considerations, and surgeon experience. Minimally invasive laparoscopic surgery is now the gold standard for most benign, small, or moderate-sized tumors, but open surgery remains essential for large, invasive, or malignant disease.
Surgical Approaches
-
Laparoscopic Adrenalectomy:
-
This is the preferred approach for most adrenal tumors, involving small incisions and minimally invasive techniques. It results in faster recovery and less postoperative pain compared to traditional open surgery.
-
-
Robotic-Assisted Surgery:
-
For complex cases or larger tumors, robotic-assisted surgery can provide enhanced precision and control. It's particularly useful for tumors located in difficult-to-reach areas.
-
-
Open Adrenalectomy:
-
This approach is used for larger tumors or when there is suspicion of malignancy. It involves a larger incision and requires a longer recovery period.
-
-
Partial Adrenalectomy:
-
In some cases, partial adrenalectomy may be performed to preserve adrenal function, especially in cases of bilateral adrenal hyperplasia or if only a portion of the gland is affected.
-
Prevention and Management of Adrenalectomy
Prevention and management of complications in adrenalectomy involve detailed preoperative preparation, careful intraoperative handling, and structured postoperative care to maintain hormonal stability, prevent adrenal crisis, and ensure safe recovery. The approach varies depending on whether the surgery is for pheochromocytoma, Cushing's syndrome, Conn's syndrome, or malignancy.
Preoperative Considerations
-
Optimization of health before surgery, including managing blood pressure, glucose levels, and electrolytes.
-
Preoperative medication adjustments: Especially in cases of pheochromocytoma, alpha-blockers may be used to reduce the risk of hypertensive crisis during surgery.
-
Informed consent: Patients should be educated about the potential risks and benefits of the surgery, including the possibility of requiring hormone replacement therapy post-surgery, especially after bilateral adrenalectomy.
Postoperative Care
-
Monitoring for complications such as bleeding, infection, or adrenal insufficiency.
-
Hormone replacement: After bilateral adrenalectomy, patients will require lifelong hormone replacement, including corticosteroids and mineralocorticoids.
-
Physical recovery: Most patients recover in 1-2 weeks for laparoscopic surgery, but open surgery may require a longer recovery period.
Complications of Adrenalectomy
Adrenalectomy is generally safe when performed by experienced endocrine surgeons, but as with any major surgery, it carries specific risks related to hormone fluctuations, anatomical proximity to vital organs, and systemic effects. Complications vary depending on surgical approach (laparoscopic, open, robotic), tumor type, and patient comorbidities.
Common Complications:
-
Infection: As with any surgical procedure, infection at the incision site is a potential risk.
-
Bleeding: Tumor removal can cause bleeding, particularly in large or vascular tumors.
-
Adrenal insufficiency: Occurs if both adrenal glands are removed or if there is insufficient adrenal function after surgery. Lifelong hormone replacement is necessary in these cases.
-
Electrolyte imbalances: Issues like low potassium or high sodium can occur post-surgery.
-
Pulmonary complications: These are common after open surgeries and may include atelectasis or pneumonia.
Rare but Serious Complications:
-
Injury to adjacent organs: Accidental injury to organs like the kidneys, liver, pancreas, or large blood vessels.
-
Adrenal crisis: If patients who undergo bilateral adrenalectomy do not receive adequate glucocorticoid replacement, they may experience a life-threatening adrenal crisis.
-
Nelson's syndrome: A rare condition that can occur after bilateral adrenalectomy for Cushing's disease, in which pituitary tumors may grow.
Living with the Condition of Adrenalectomy
Living after adrenalectomy is generally very good, especially if the underlying disease is cured and hormonal balance is maintained. Most people experience improved symptoms, normal activity levels, and a return to daily life, but some require lifelong hormone monitoring or replacement therapy. Lifestyle adjustments, regular checkups, and awareness of adrenal insufficiency symptoms are essential, particularly after bilateral adrenalectomy or surgery for hormone-secreting tumors.
Postoperative Care and Recovery
After the surgery, the patient will need to stay in the hospital for monitoring. Recovery typically involves:
-
Pain management: Using medication to control pain and discomfort during recovery.
-
Monitoring: Checking vital signs, hormone levels, electrolytes, and organ function.
-
Gradual mobilization: Encouraging light physical activity as recovery progresses.
Hormone Replacement
For patients undergoing bilateral adrenalectomy, lifelong hormone replacement therapy is required. This involves taking glucocorticoids (e.g., hydrocortisone) and mineralocorticoids (e.g., fludrocortisone) to compensate for the loss of adrenal function.
For those undergoing unilateral adrenalectomy, the remaining adrenal gland usually compensates, and hormone replacement is not needed, though regular follow-up is necessary.
Follow-Up and Long-Term Care
-
Regular blood tests: Hormone levels, electrolytes, and other tests should be monitored regularly to ensure proper function and medication adjustment.
-
Life-long monitoring: Especially in cases of bilateral adrenalectomy, patients must be vigilant about symptoms of adrenal insufficiency and take their hormone replacement as prescribed.
Lifestyle Adjustments
-
Diet: Maintain a balanced diet and ensure adequate sodium intake if you're on mineralocorticoid replacement.
-
Exercise: Gradually return to exercise as advised by your healthcare provider.
-
Stress management: It is essential to adjust steroid doses during stress, illness, or surgery to prevent adrenal crisis.
Top 10 Frequently Asked Questions about Adrenalectomy
1. What is an adrenalectomy?
An adrenalectomy is a surgical procedure to remove one or both
adrenal glands. The adrenal glands are small glands located above each
kidney that produce hormones, including adrenaline, cortisol, aldosterone, and
sex hormones.
The surgery is usually performed to treat tumors, hormone-producing adrenal
disorders, or cancer, or when a gland is enlarged or causing health
problems.
2. Why is adrenalectomy performed?
Adrenalectomy is typically recommended for:
-
Adrenal tumors: Both benign (adenomas) and malignant tumors.
-
Pheochromocytoma: A rare tumor that produces excess adrenaline.
-
Cushing's syndrome: Caused by overproduction of cortisol.
-
Primary hyperaldosteronism (Conn's syndrome): Overproduction of aldosterone causing high blood pressure.
-
Adrenal cancer or metastasis from other cancers.
The goal is to remove the diseased gland and restore normal hormone balance.
3. What are the different types of adrenalectomy?
There are mainly two types of adrenalectomy:
-
Open adrenalectomy:
-
Involves a larger incision in the abdomen, back, or side to access the adrenal gland.
-
Usually performed for large tumors or cancer.
-
-
Laparoscopic (minimally invasive) adrenalectomy:
-
Performed using small incisions and a camera.
-
Faster recovery, less pain, and smaller scars.
-
Robotic-assisted adrenalectomy is also an option in some centers for enhanced precision.
4. How is the adrenalectomy procedure performed?
-
The patient is placed under general anesthesia.
-
The surgeon makes either small laparoscopic incisions or a larger open incision depending on the type and size of the tumor.
-
The adrenal gland is carefully isolated and removed.
-
Surrounding tissues are preserved as much as possible, and the incision is closed.
The procedure usually takes 2-4 hours, depending on complexity.
5. What are the risks and complications of adrenalectomy?
Like any surgery, adrenalectomy carries risks, including:
-
Bleeding during or after surgery.
-
Infection at the incision site.
-
Damage to surrounding organs (kidneys, spleen, pancreas, liver).
-
Hormonal imbalances, especially if both glands are removed.
-
Blood pressure fluctuations during surgery (common with pheochromocytoma).
-
Rare complications include blood clots or anesthesia-related risks.
Proper preoperative evaluation and post-operative care reduce the likelihood of complications.
6. What is the recovery process after adrenalectomy?
-
Hospital stay: Usually 2-5 days for laparoscopic surgery, longer for open surgery.
-
Pain management: Pain is usually controlled with medications.
-
Diet: Patients can gradually resume normal diet as tolerated.
-
Activity: Light activity can be resumed within 1-2 weeks, with full recovery in 4-6 weeks for laparoscopic surgery or 6-8 weeks for open surgery.
-
Follow-up: Hormone levels are monitored postoperatively, especially if both adrenal glands were removed.
7. Will I need hormone replacement therapy after adrenalectomy?
-
Single adrenal gland removal: Usually, the remaining gland compensates, and hormone replacement may not be necessary.
-
Both adrenal glands removed (bilateral adrenalectomy): Lifelong hormone replacement therapy is required, including cortisol and aldosterone, to maintain essential body functions.
-
Hormone replacement therapy is carefully managed and monitored by an endocrinologist to prevent adrenal insufficiency.
8. Can adrenalectomy be performed for small tumors?
Yes, even small adrenal tumors that produce excess hormones (functioning tumors) may require surgery to prevent long-term complications like high blood pressure, heart disease, or metabolic problems.
-
Small, non-functioning tumors may be monitored with imaging unless they grow or become symptomatic.
9. Are there any alternatives to adrenalectomy?
Alternatives depend on the type of adrenal disorder:
-
Medical management: Certain hormone disorders can be treated with medication (e.g., alpha-blockers for pheochromocytoma).
-
Observation: Small, non-functioning tumors can sometimes be monitored with regular imaging.
-
However, surgical removal is often the definitive treatment for hormone-producing tumors or cancer.
10. What is the long-term outlook after adrenalectomy?
The long-term outlook is generally excellent, especially if the surgery is done for benign tumors or functioning adrenal glands.
-
Most patients experience improvement in blood pressure, hormone balance, and symptoms associated with hormone overproduction.
-
Lifelong follow-up may be required for cancer cases or bilateral adrenalectomy.
-
With appropriate hormone replacement therapy (if needed) and regular medical check-ups, most patients can return to normal activities and maintain a good quality of life.


