Introduction to Carotid Artery Surgery / Endarterectomy
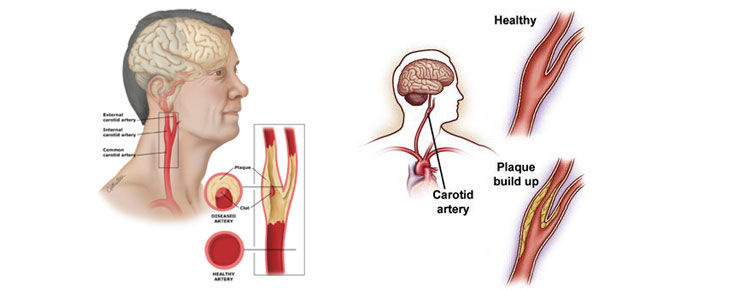
Carotid endarterectomy (CEA) is a highly effective surgical procedure designed to prevent strokes by removing plaque from the carotid arteries, which are the major blood vessels supplying the brain. When these arteries become narrowed due to atherosclerosis - a buildup of fatty deposits, cholesterol, and inflammatory material - blood flow to the brain is restricted, increasing the risk of transient ischemic attacks (TIAs) or stroke. Carotid endarterectomy is considered a standard treatment for patients with significant narrowing, particularly those who have experienced symptoms such as TIAs, minor strokes, or recurrent neurological deficits caused by insufficient blood flow to the brain.
The surgery involves a careful incision in the neck to access the affected carotid artery. The surgeon then removes the plaque to restore normal blood flow. In some cases, a patch may be sewn into the artery to maintain its width and prevent future narrowing. Carotid artery surgery not only reduces the risk of stroke but also improves cerebral perfusion, which can enhance cognitive function and overall neurological health. Over the past decades, advances in imaging, anesthesia, and surgical techniques have made the procedure safer and more effective, with high rates of long-term success when performed in specialized vascular centers.
Carotid endarterectomy is often recommended after careful evaluation of the patient's symptoms, imaging studies, and overall cardiovascular risk profile. For many patients, timely intervention can be life-saving, preventing debilitating strokes and providing improved quality of life. Understanding this procedure, its indications, and its potential risks is essential for anyone diagnosed with carotid artery disease.
Causes and Risk of Carotid Artery Surgery / Endarterectomy
Though the surgery itself is a treatment rather than a disease, the underlying cause prompting CEA is significant narrowing (stenosis) of the carotid artery, usually due to atherosclerosis. Key causes and risk factors include:
-
Atherosclerosis: the accumulation of fatty deposits (plaques) in the inner layer of arteries. In the carotid artery, the bifurcation (branching) is a common site of plaque build-up because of turbulent flow.
-
Age: older age increases risk of plaque formation and carotid narrowing.
-
Hypertension (high blood pressure), hyperlipidemia (high cholesterol/fats in blood), diabetes mellitus: all contribute to the damage of arterial walls and accelerate atherosclerosis.
-
Smoking: a powerful modifiable risk factor for vascular disease including carotid stenosis.
-
Male gender and family history of cardiovascular or cerebrovascular disease: risk tends to be higher.
-
Other vascular disease: presence of coronary artery disease or peripheral arterial disease increases the likelihood of carotid disease.
-
Plaque-specific characteristics: Some plaques are more unstable (for example ulcerated, with intraplaque hemorrhage, echolucent) and are more likely to cause embolic events or prompt surgical intervention.
In terms of risk related to the surgery, CEA is generally safe
in experienced hands but the risk of complications depends on patient factors:
advanced age, severe comorbidities (heart disease, kidney disease), prior
stroke, anatomical factors like contralateral carotid occlusion, or previous
neck surgery/radiation can increase surgical risk.
Thus, the "cause" for performing the surgery is essentially the presence of
significant carotid stenosis due to atherosclerosis in a patient whose risk of
stroke warrants intervention. The "risk" part refers both to the underlying
disease and to the operative risk of the procedure itself.
Symptoms and Signs of Carotid Artery Surgery / Endarterectomy
Since carotid endarterectomy is a treatment, the symptoms and signs to be aware of are those of carotid artery disease and its complications - which would prompt the evaluation for possible surgery.
Symptoms might include:
-
Transient ischemic attacks (TIAs) - brief episodes of neurological dysfunction such as sudden weakness or numbness of one side of the face or body, difficulty speaking or understanding speech, sudden visual loss in one eye (amaurosis fugax). These may last a few minutes to less than 24 hours.
-
Mild stroke: persistent deficits from reduced blood flow or an embolic event from the carotid plaque.
-
Sometimes no obvious symptoms - carotid stenosis may be discovered incidentally when imaging is done for another reason; such patients are termed "asymptomatic."
Signs on physical examination may include:
-
A carotid bruit: a whooshing or blowing sound heard over the carotid
artery in the neck with a stethoscope - though its sensitivity and
specificity are limited.
-
Neurological deficits: depending on stroke or TIA, there may be weakness,
sensory changes, speech disturbance.
-
In some cases: no obvious signs until imaging is done.
A carotid bruit: a whooshing or blowing sound heard over the carotid artery in the neck with a stethoscope - though its sensitivity and specificity are limited.
Neurological deficits: depending on stroke or TIA, there may be weakness, sensory changes, speech disturbance.
In some cases: no obvious signs until imaging is done.
It is important to note that although many patients with carotid stenosis are asymptomatic, the risk of stroke increases with higher degrees of narrowing, and that is why timing and decision-making for surgery become critical.
Diagnosis of Carotid Artery Surgery / Endarterectomy
Diagnosis in this context refers to identifying significant carotid stenosis (the indication for surgery) and assessing the patient's surgical risk and suitability for CEA. The major elements are:
Non-invasive imaging:
-
Carotid duplex ultrasonography (duplex US) - first line for assessing carotid arteries: measures velocity of blood flow and estimates degree of stenosis.
-
Computed Tomography Angiography (CTA) of neck/brain - gives detailed anatomical view of carotid arteries and atherosclerotic plaque.
-
Magnetic Resonance Angiography (MRA) - alternative when CTA is contraindicated (e.g., due to contrast allergy or renal issues).
Clinical evaluation:
-
History of neurological events (TIA, stroke), timing of events, severity of symptoms.
-
Assessment of risk factors (hypertension, diabetes, smoking, cholesterol, cardiovascular disease).
-
Examination for signs such as bruit, neurological deficits.
Surgical/operative evaluation:
-
Stroke work-up: brain imaging to assess prior infarcts, viability of brain tissue, and risk of reperfusion. Some centres may use transcranial Doppler or other advanced imaging to look for microemboli or impaired cerebrovascular reserve (which can indicate higher risk).
-
Cardiovascular evaluation: because many patients have co-existent heart disease, a full cardiac assessment is often undertaken to gauge operative risk.
-
Timing: For symptomatic patients, most guidelines emphasize performing CEA as soon as safely possible (ideally within 2 weeks of last event) to maximize benefit.
-
Risk stratification: The patient's anatomy (for example, contralateral carotid occlusion, prior neck radiation, high bifurcation) and comorbidities will influence whether surgery is feasible and safe.
Thus, the diagnosis phase is both about confirming the anatomical severity of carotid narrowing and establishing that the patient is a suitable candidate for surgery.
Treatment Options of Carotid Artery Surgery / Endarterectomy
When significant carotid stenosis is identified and a decision is made that intervention is warranted, the treatment options are broadly: medical management (best medical therapy), surgical management (CEA), or endovascular treatment (e.g., carotid artery stenting, CAS). Here we focus on CEA but also mention alternatives and place in context.
Best medical therapy (BMT):
-
This includes antiplatelet therapy (eg, aspirin), high-intensity statin therapy, blood pressure control, diabetes control, smoking cessation, and lifestyle modification. In many asymptomatic cases, intensive medical therapy may be the mainstay.
-
Recent data suggest that the annual risk of ipsilateral stroke in asymptomatic carotid stenosis patients under modern medical therapy may be around 1% per year.
Carotid Endarterectomy (CEA):
-
This is the surgical removal of plaque from the carotid artery. The procedure typically involves an incision in the neck, clamping of the artery (temporarily redirecting blood flow if needed), opening the artery, removing the plaque, often placing a patch (or performing eversion endarterectomy), then restoring blood flow.
-
Indications:
-
In symptomatic patients (i.e., those who have had a TIA or minor stroke) with high-grade stenosis (usually ≥70% to 99%) surgery is recommended because it significantly reduces stroke risk.
-
In patients with 50-69% symptomatic stenosis, the benefit is smaller and must be weighed.
-
In asymptomatic patients, CEA may be considered in select cases (for example ≥60-99% stenosis, low surgical risk, life expectancy >5 years) but benefit is more modest and the decision is more nuanced.
-
-
Timing matters: for symptomatic patients, performing CEA early (ideally within 14 days of last event) yields the greatest benefit.
Carotid artery stenting (CAS):
-
An endovascular alternative to CEA, where a stent is placed to keep the artery open rather than removing plaque via open surgery.
-
CAS may be considered in patients who are high surgical risk or have anatomical issues making surgery difficult. Some guidelines caution that CAS carries higher peri-procedural risk of stroke in older patients (>70 yrs) compared with CEA.
Choosing between treatments:
-
The choice depends on: symptom status, degree of stenosis, patient's surgical risk, anatomical considerations, timing since last neurological event, centre/surgeon experience, and patient preference.
-
The current trend emphasizes multidisciplinary decision-making and strong quality assurance (low peri-operative stroke/death rates) before performing CEA or CAS.
For your content: In this section you can describe the surgical technique of CEA (step-by-step), discuss pre-operative preparation, intra-operative steps, post-operative care and compare with CAS and medical therapy, including pros/cons of each.
Prevention and Management of Carotid Artery Surgery / Endarterectomy
Prevention in this context refers both to preventing carotid artery disease (thus avoiding need for surgery) and managing the condition (either pre-surgery or post-surgery) so that outcomes are optimized.
Preventive strategies for carotid artery disease:
-
Lifestyle modification: smoking cessation, healthy diet (low saturated fat, high in fruits/vegetables), regular physical activity, weight control.
-
Risk factor control:
-
Blood pressure: maintain within guideline-recommended levels.
-
Lipids: use statins and other lipid-lowering therapies to stabilize and reduce plaque progression.
-
Diabetes: ensure good glycaemic control.
-
-
Antiplatelet therapy: in patients at high cardiovascular risk (and in those with known carotid disease) low-dose aspirin may be used.
-
Screening / monitoring: Routine screening for carotid stenosis in asymptomatic general population is not recommended. However, in selected high-risk individuals (eg, existing vascular disease, previous stroke/TIA) targeted evaluation may be considered.
Management (pre- and post-operatively):
-
Pre-operative preparation: assessing and optimizing comorbidities (heart, kidney, lung), discontinuing or modifying medications that may increase bleeding risk, ensuring the patient has quit smoking, ensuring good control of hypertension and diabetes.
-
Post-operative care: after CEA, patients are monitored for complications (e.g., bleeding, nerve injury, stroke), may resume antiplatelet therapy, continue or start statins, preventive lifestyle measures. Regular follow-up imaging (e.g., carotid duplex) may be recommended to assess for restenosis.
-
Long-term management: Even after successful surgery, the atherosclerotic process remains systemic. Patients must remain on optimal medical therapy and lifestyle modification to prevent new plaque formation or disease progression elsewhere.
-
Patient education: teaching patients the signs/symptoms of stroke or TIAs, the importance of medication adherence, risk factor control and follow-up is critical.
In your blog, you could highlight "what you can do" sections: for example "10 Ways to Reduce Your Risk" or "What to ask your doctor if you're going for CEA".
Complications of Carotid Artery Surgery / Endarterectomy
As with any surgery, carotid endarterectomy carries potential complications - both specific to the procedure and general surgical risks. It's important to inform readers so they understand risk vs benefit when considering the surgery.
Common/less severe complications:
-
Bleeding or hematoma at the surgical site (neck).
-
Infection of incision.
-
Swelling around the neck incision, pain, discomfort.
-
Temporary nerve-injury symptoms: because several small nerves (to tongue, voice box, facial muscles) run near the carotid artery, patients may have hoarseness, numbness around the wound, difficulty swallowing or moving the tongue; these often resolve.
-
Patch-site complications (if a patch is used to close the artery) such as localized narrowing or thrombosis.
Major/serious complications:
-
Stroke: paradoxically, surgery to prevent stroke carries a small risk of causing one-either during the procedure (embolism, clamping, reperfusion) or in the peri-operative period. An experienced surgical team tries to keep this risk very low (ideally <3-4% in good centres).
-
Heart attack (myocardial infarction): because many patients undergoing CEA have underlying coronary disease.
-
Re-stenosis or occlusion: the treated carotid artery may gradually narrow again (although with modern patch and operative techniques this is relatively uncommon).
-
Nerve-injury lasting longer term: e.g., permanent damage to recurrent laryngeal nerve, hypoglossal nerve, accessory nerve.
-
Hyperperfusion syndrome: rare but serious, when the brain receives too much blood too quickly after a long-standing severe stenosis, leading to headache, seizures, intracerebral haemorrhage.
-
Death: very low incidence in well-selected patients and skilled centres, but a recognized risk especially in patients with comorbidities.
In your blog you can also mention "what factors increase risk of complications" (older age, kidney disease, previous stroke, contralateral carotid occlusion, high bifurcation, high surgical risk) and "how complication risk is minimized" (experienced surgeon, good centre volume, pre-operative optimization, timely surgery).
Living with the Condition of Carotid Artery Surgery / Endarterectomy
This section addresses what patients can expect - both before and after surgery - and how their life may change, what follow-up is needed, and what lifestyle adjustments are recommended.
Before surgery:
-
Patients may face anxiety about the risk of stroke and the need for surgery. They should have counselling about the benefits, risks, timing, and alternatives (medical therapy, stenting).
-
Pre-operative instructions: quitting smoking, controlling risk factors, understanding the procedure and recovery time, arranging for support and care at home post-op.
After surgery - short term:
-
Recovery time: Many patients stay in hospital 1-2 days (depending on centre), and may return to most normal activities within 1-2 weeks (but driving and heavy activity may be delayed based on surgeon advice).
-
Wound care: monitoring the incision in the neck, avoiding strain, following instructions about showering, avoiding heavy lifting until cleared.
-
Medication: Resuming antiplatelets (or starting dual antiplatelet/anticoagulants if indicated), statins, controlling blood pressure and diabetes.
-
Follow-up imaging: Carotid duplex ultrasound at intervals (e.g., 1 month, then every 6 months for 2 yrs, then yearly) may be done to monitor for restenosis.
After surgery - long term:
-
Lifestyle matters: Even though the plaque in that one carotid artery has been removed, the atherosclerotic process remains systemic; patients must adopt/maintain healthy lifestyle and risk factor control to prevent disease elsewhere (heart, peripheral arteries, other carotid).
-
Awareness: Patients must know signs of stroke/TIA and act urgently if symptoms occur - even after surgery.
-
Emotional/quality-of-life aspects: Some patients may experience temporary voice or swallowing changes, numbness, or discomfort, which generally improve. Some may feel guilty or anxious about their pre-operative risk factors (eg smoking) and may need support to adapt to longer-term changes.
-
Return to normal activities: Depending on individual health, many patients can expect good outcomes - the goal of CEA is to reduce future stroke risk and improve long-term survival and quality of life. Some limitations may persist depending on other vascular or neurological disease.
-
Coordination of care: Regular check-ups with vascular surgeon, neurologist or stroke specialist, primary care physician, and monitoring of cardiovascular risk factors is important.
In your blog you may wish to include a "Patient story" or "What to expect" timeline (Day 0, Day 1, Week 1, Month 1, Year 1) to make this relatable and help patients understand the journey.
Top 10 Frequently Asked Questions about Carotid Artery Surgery / Endarterectomy
1. What is Carotid Artery Surgery / Endarterectomy?
Carotid endarterectomy is a surgical procedure to remove plaque (fatty deposits) from the carotid arteries in the neck. Plaque buildup can narrow these arteries (carotid stenosis) and reduce blood flow to the brain, increasing the risk of stroke.
During surgery, the artery is opened, plaque is carefully removed, and the artery is repaired to restore normal blood flow.
2. Why Is Carotid Endarterectomy Needed?
Carotid surgery is recommended for patients with:
-
Significant carotid artery narrowing (usually ≥70%).
-
History of transient ischemic attacks (TIA) or mini-strokes.
-
High risk of stroke due to plaque accumulation.
-
Symptoms such as sudden weakness, numbness, difficulty speaking, or vision changes.
The goal is stroke prevention by improving blood flow to the brain.
3. How is Carotid Artery Surgery Performed?
The surgery is typically performed under general or local anesthesia and involves:
-
Making an incision in the neck to access the carotid artery.
-
Temporarily clamping the artery to stop blood flow.
-
Removing the plaque from the inner lining of the artery.
-
Repairing the artery, either by direct closure or using a patch to widen it.
-
Closing the incision and monitoring blood flow to the brain.
The procedure usually takes 1-2 hours, depending on the complexity.
4. Who is a Good Candidate for Carotid Endarterectomy?
Candidates include patients with:
-
Moderate to severe carotid artery stenosis.
-
History of stroke or TIA.
-
Plaque buildup causing symptoms of poor blood flow.
-
No medical conditions that make surgery extremely risky.
Your vascular surgeon will evaluate your medical history, imaging studies (ultrasound, CT angiography), and overall health to determine suitability.
5. What Are the Risks of Carotid Artery Surgery?
While generally safe, carotid surgery carries some risks:
-
Stroke or heart attack (rare but serious).
-
Bleeding at the surgical site.
-
Infection in the incision area.
-
Nerve injury, causing temporary or rarely permanent weakness, numbness, or hoarseness.
-
Re-narrowing of the artery over time.
Most complications are minimized by careful surgical technique and proper monitoring.
6. How Should I Prepare for Carotid Surgery?
Preparation includes:
-
Fasting for 6-8 hours before surgery.
-
Stopping certain medications, especially blood thinners, as advised by your doctor.
-
Undergoing preoperative tests such as blood tests, ECG, chest X-ray, and carotid imaging.
-
Arranging for someone to accompany you home after discharge if performed as an outpatient procedure.
Following these instructions helps ensure a safe and smooth procedure.
7. What Is the Recovery Process Like?
-
Hospital Stay: Usually 1-2 days after surgery.
-
First Few Days: Mild neck discomfort, bruising, or swelling is common.
-
Weeks 1-2: Resume light activities and avoid strenuous exercise.
-
Follow-Up: Regular checkups and imaging to monitor artery health.
Most patients return to normal activities within 2-4 weeks, depending on recovery and overall health.
8. Are There Non-Surgical Alternatives to Carotid Endarterectomy?
Yes, alternatives may include:
-
Medical management: Blood thinners, cholesterol-lowering drugs (statins), and blood pressure control.
-
Lifestyle changes: Healthy diet, exercise, smoking cessation.
-
Carotid artery stenting: A minimally invasive procedure where a stent is placed to open the narrowed artery.
However, for patients with high-grade stenosis or symptoms, surgery is often the most effective way to prevent stroke.
9. Will Carotid Surgery Prevent a Stroke?
Carotid endarterectomy significantly reduces the risk of stroke, especially in patients with symptomatic high-grade stenosis.
While it does not eliminate all risk, the procedure restores proper blood flow to the brain and lowers the chance of future strokes, particularly in patients who have already experienced TIA or minor strokes.
10. How Long Do the Results Last?
-
Carotid endarterectomy typically provides long-lasting results, often preventing stroke for many years.
-
In some cases, arteries may re-narrow (restenosis) over time, which can be monitored with regular ultrasound or imaging tests.
-
Maintaining a heart-healthy lifestyle and managing risk factors such as hypertension, diabetes, and high cholesterol improves long-term success.


