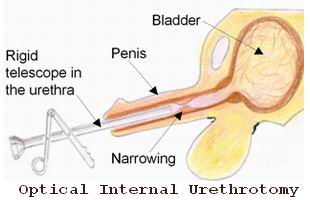
Introduction to Optical Internal Urethrotomy (OIU)
Optical Internal Urethrotomy (OIU) is a minimally invasive surgical procedure used to treat urethral strictures, a condition characterized by the narrowing of the urethra. This narrowing obstructs the normal flow of urine and can lead to a variety of symptoms such as a weak urine stream, pain during urination, and frequent urinary tract infections (UTIs).
OIU involves the insertion of an endoscope (specifically a cystoscope) into the urethra to visualize the stricture and a cutting instrument (such as a laser or knife) is then used to make an incision to widen the narrow segment of the urethra. This allows for the restoration of normal urine flow.
This procedure is most commonly performed in individuals with short or localized strictures of the urethra. It is often the preferred treatment for non-complex strictures that have not responded to conservative treatments like dilation.
Benefits of Optical Internal Urethrotomy:
-
Minimally Invasive: Performed through the urethra, meaning there are no external incisions.
-
Quick Recovery: Most patients can resume normal activities within a few days.
-
Outpatient Procedure: Often done on an outpatient basis, meaning no overnight hospital stay is required.
-
High Success Rate: Effective for short strictures and offers significant relief from symptoms.
Causes and Risk Factors for Urethral Strictures
Urethral strictures can arise from multiple factors, each of which contributes to the narrowing of the urethra. Understanding the causes and associated risks is important for both prevention and effective treatment.
2.1 Trauma or Injury to the Urethra
One of the most common causes of urethral strictures is physical trauma to the urethra. Trauma can occur as a result of:
-
Accidents or Pelvic Injuries: Direct injury to the pelvic region or blunt force trauma can damage the urethra, leading to scarring.
-
Medical Procedures: Urethral strictures can develop after invasive procedures such as urethral catheterization (especially long-term catheter use), prostate surgery, or transurethral resection (TURP).
-
Sexual Trauma: Forced or rough sexual activity may also cause injury to the urethra, especially if the trauma is repeated or severe.
2.2 Chronic Infections and Inflammatory Conditions
-
Chronic Urinary Tract Infections (UTIs): Untreated or recurrent infections can cause inflammation and scarring of the urethra, eventually leading to strictures.
-
Sexually Transmitted Infections (STIs): Infections like gonorrhea or chlamydia can lead to scarring in the urethra.
-
Balanitis Xerotica Obliterans (BXO): This chronic inflammatory condition causes scarring of the glans penis and can extend into the urethra, leading to strictures.
2.3 Congenital Conditions
-
Congenital Urethral Strictures: Some individuals are born with a narrow urethra, which may predispose them to developing strictures over time.
-
Posterior Urethral Valves (PUV): This is a congenital abnormality in males where extra tissue obstructs the urethra, which can cause damage and lead to stricture formation.
2.4 Iatrogenic Causes
Iatrogenic causes are those induced by medical treatment or procedures:
-
Catheterization: Prolonged or improper use of urinary catheters can cause trauma to the urethra, leading to strictures. This is particularly common in individuals with spinal cord injuries or those who require long-term catheter use.
-
Surgical Procedures: Prior surgeries, especially those involving the prostate, bladder, or urethra, may leave behind scarring that can result in narrowing of the urethra.
2.5 Risk Factors
-
Male Gender: Men are more commonly affected by urethral strictures because of the longer length of the male urethra.
-
Age: Older individuals may be more susceptible to urethral strictures due to changes in the urethra over time.
-
History of Surgery: Individuals who have previously undergone surgeries such as prostate surgery or circumcision are at higher risk for developing strictures.
Symptoms and Signs of Urethral Strictures
The symptoms of urethral strictures can be subtle at first, but as the stricture progresses, they can cause significant discomfort and affect the quality of life. Common signs and symptoms include:
3.1 Urinary Symptoms
-
Weak or Interrupted Urine Stream: A narrowing of the urethra leads to difficulty urinating and a reduced or intermittent urine flow. The urine stream may become weaker over time, making it more difficult to empty the bladder completely.
-
Spraying or Split Stream: When the urethra is narrowed, the urine may spray or split in multiple directions rather than coming out in a single stream.
-
Straining to Urinate: Increased effort is required to pass urine, which can be exhausting and uncomfortable.
-
Frequent Urination: The individual may feel the need to urinate more frequently, even if little urine is passed each time.
-
Urgency and Hesitancy: A sudden urge to urinate or difficulty starting urination is common in people with urethral strictures.
3.2 Pain and Discomfort
-
Painful Urination (Dysuria): Urinary pain or a burning sensation may occur, especially if the stricture is caused by inflammation or infection.
-
Pelvic or Perineal Pain: Some individuals may experience pain in the lower abdomen, pelvic area, or perineum due to the obstruction of the urethra.
3.3 Blood in the Urine (Hematuria)
-
Gross Hematuria: Blood in the urine that is visible to the naked eye may occur, especially if the stricture has caused trauma or infection. The urine may appear pink, red, or brown.
-
Microscopic Hematuria: Blood in the urine that is only detectable through lab tests (urinalysis).
Diagnosis of Urethral Strictures
A thorough diagnosis is essential for determining the severity and location of the stricture, as well as identifying the appropriate treatment plan. Diagnostic tools include:
4.1 Physical Examination
The doctor will begin by evaluating symptoms and asking about the patient’s medical history, including any history of urinary tract infections, previous surgeries, or trauma. A physical examination may include palpating the abdomen to check for any signs of bladder distention.
4.2 Uroflowmetry
-
Uroflowmetry is used to measure the rate of urine flow and determine whether there is a blockage in the urinary tract. A reduced flow rate is indicative of a stricture.
4.3 Retrograde Urethrogram (RUG)
-
RUG is a diagnostic test in which a contrast dye is injected into the urethra, and X-rays are taken to visualize the shape, size, and location of the stricture. This test is essential for locating the stricture.
4.4 Cystoscopy
-
Cystoscopy is a procedure in which a small camera (cystoscope) is inserted through the urethra to directly visualize the inside of the urethra and bladder. This allows the urologist to assess the severity of the stricture and decide on the best course of treatment.
4.5 Urethral Dilation
-
In some cases, a urethral dilation procedure may be performed to assess the degree of narrowing and determine if dilation is a viable treatment option. This involves the insertion of progressively larger dilators into the urethra.
Treatment Options for Urethral Strictures
Several treatment options are available for managing urethral strictures, depending on the severity, location, and cause of the narrowing.
5.1 Optical Internal Urethrotomy (OIU)
-
Procedure: OIU involves inserting a cystoscope into the urethra to visualize the stricture, followed by using a cutting instrument (such as a laser or scalpel) to make an incision and widen the urethra.
-
Indications: Best for short, localized strictures in individuals without significant scarring or other complications. It is effective in most cases but may not be suitable for long or complex strictures.
5.2 Urethral Dilation
-
Procedure: Urethral dilation involves the insertion of progressively larger tubes or catheters into the urethra to widen the stricture. This is a temporary solution, and strictures may recur over time.
5.3 Urethroplasty
-
Procedure: Urethroplasty is a more invasive surgical procedure that involves removal of the stricture and reconstruction of the urethra using tissue from another part of the body. This method is generally reserved for long, complex, or recurrent strictures.
5.4 Laser Urethrotomy
-
Procedure: Laser urethrotomy uses a laser to cut through the scar tissue causing the stricture. This method can be more precise than traditional cutting instruments and is used in some cases for more difficult-to-reach strictures.
Prevention and Management of Urethral Strictures
6.1 Preventive Measures
-
Avoiding Trauma: Limiting unnecessary catheterization and ensuring proper technique during urethral procedures can reduce the risk of injury and subsequent strictures.
-
Managing Infections: Promptly treating urinary tract infections (UTIs) and sexually transmitted infections (STIs) can help prevent inflammation and scarring that lead to strictures.
6.2 Long-Term Management
-
Regular Monitoring: Regular check-ups with a urologist can help detect any recurrence of the stricture early. This may include routine cystoscopies and uroflowmetry tests.
-
Self-Catheterization: Some patients may be taught how to perform self-catheterization to help keep the urethra open and prevent re-narrowing.
-
Lifestyle Adjustments: Staying hydrated, maintaining good hygiene, and avoiding smoking can improve overall urinary health and reduce the likelihood of further issues.
Complications of Optical Internal Urethrotomy
Though OIU is generally safe, complications can arise:
-
Infection: As with any surgical procedure, there is a risk of infection, particularly urinary tract infections.
-
Bleeding: Minor bleeding is common during the procedure, but significant bleeding is rare.
-
Recurrence of the Stricture: The stricture may recur over time, requiring further treatments.
-
Urethral Perforation: In rare cases, the urethra may be accidentally perforated during the procedure.
Living with Urethral Strictures Post-Treatment
After undergoing OIU, patients can expect a quick recovery, but long-term management is essential.
8.1 Psychological and Emotional Support
-
Living with a urethral stricture and undergoing repeated treatments can be emotionally challenging. Support groups, counseling, and stress management techniques can be beneficial.
8.2 Recovery and Follow-Up Care
-
Post-Operative Care: Following the procedure, patients should follow all instructions for aftercare, including drinking plenty of fluids, avoiding strenuous activities, and taking prescribed medications to prevent infections.
-
Follow-Up Appointments: Regular visits to the urologist are necessary to monitor for any recurrence of symptoms or stricture formation.
Top 10 Frequently Asked Questions about Optical Internal Urethrotomy (OIU)
1. What is Optical Internal Urethrotomy (OIU)?
Optical Internal Urethrotomy (OIU) is a minimally invasive surgical procedure used to treat urethral strictures (narrowing of the urethra). It involves using a special instrument called a urethrotome, which is inserted through the urethra to cut or incise the scar tissue causing the blockage. This procedure restores normal urine flow and alleviates symptoms like difficulty urinating.
2. Why is Optical Internal Urethrotomy performed?
OIU is typically performed to treat urethral strictures, which can cause:
-
Painful urination
-
Weak urine flow
-
Difficulty starting urination
-
Urinary retention
Strictures can result from injury, infection, previous surgery, or underlying conditions like urethral scarring due to chronic inflammation.
3. How is Optical Internal Urethrotomy performed?
The procedure is usually performed under local or general anesthesia, depending on the patient's condition. The surgeon uses a cystoscope (a thin tube with a camera) to visualize the inside of the urethra and insert the urethrotome. The instrument is then used to cut the scar tissue or stricture, allowing the urethra to expand and improve urine flow.
4. Is Optical Internal Urethrotomy a painful procedure?
OIU is generally considered minimally painful, especially when local anesthesia is used. After the procedure, patients may experience mild discomfort, a burning sensation during urination, or slight bleeding, but these symptoms typically resolve within a few days. Severe pain is uncommon.
5. What are the benefits of Optical Internal Urethrotomy?
The benefits of OIU include:
-
Minimally invasive: The procedure is performed through the urethra without the need for incisions.
-
Quick recovery: Most patients can return to normal activities within a few days.
-
Effectiveness: It successfully restores urine flow and relieves symptoms in most cases.
-
Reduced complication rates: Compared to open surgery, OIU carries fewer risks of complications.
6. What are the risks or complications of Optical Internal Urethrotomy?
While OIU is generally safe, possible risks include:
-
Infection: Post-procedure urinary tract infections (UTIs) are a common risk.
-
Bleeding: Some blood in the urine is normal, but excessive bleeding may require further treatment.
-
Stricture recurrence: In some cases, the stricture may return, requiring additional treatment.
-
Injury to the urethra: Rarely, the urethra may be damaged during the procedure.
7. How long does it take to recover from Optical Internal Urethrotomy?
Recovery from OIU is generally quick. Most patients can return to normal activities within 3-7 days. Some mild discomfort, including a burning sensation during urination, may persist for a few days. It's important to drink plenty of fluids and follow post-procedure care instructions to reduce the risk of complications.
8. How effective is Optical Internal Urethrotomy in treating urethral strictures?
OIU is effective for treating mild to moderate urethral strictures. Success rates vary, but around 70-80% of patients experience significant improvement in urinary flow after the procedure. However, recurrence of the stricture can occur, particularly in more severe cases. Repeat treatments may be necessary for long-term relief.
9. When should I consider Optical Internal Urethrotomy?
OIU is considered when:
-
The stricture is located in an area accessible through the urethra (usually near the meatus or bulbous urethra).
-
There is difficulty urinating, or the stricture causes urinary retention.
-
Conservative treatments, such as dilation or medication, have not been effective.
-
The stricture is not too long or complex, and surgery would be too invasive.
10. Are there any alternatives to Optical Internal Urethrotomy?
Yes, alternatives include:
-
Dilation: A non-surgical procedure where the urethra is gradually widened using a balloon.
-
Urethroplasty: A more complex surgery where the stricture is excised and the urethra is reconstructed, often used for long or recurrent strictures.
-
Self-catheterization: For patients with severe strictures who need to manage urinary retention.


