Introduction to Cardiac Pacing and Electrophysiology
Cardiac pacing and electrophysiology are key areas of cardiology that deal with the electrical activity of the heart. Understanding these aspects is crucial for diagnosing and managing heart rhythm disorders, known as arrhythmias. These disorders, which include conditions such as bradycardia (slow heart rate), tachycardia (fast heart rate), and atrial fibrillation, can significantly affect cardiovascular health and overall quality of life.
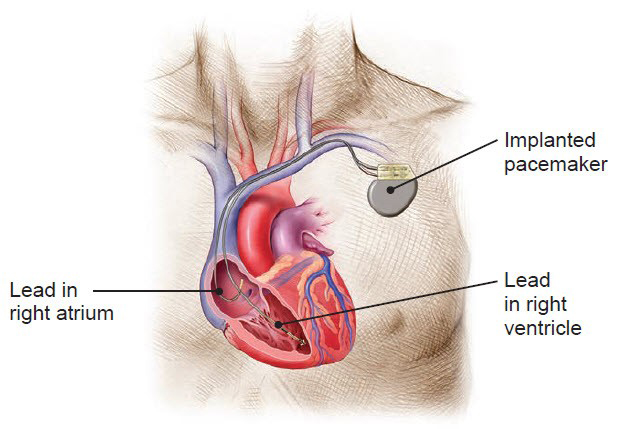
Cardiac pacing refers to the use of a pacemaker or implantable cardioverter-defibrillator (ICD), devices that help regulate the heart's rhythm by delivering electrical impulses. These devices are implanted into the body to correct abnormal heart rhythms and prevent life-threatening events like sudden cardiac arrest.
Electrophysiology, on the other hand, involves studying the electrical conduction system of the heart. Through techniques like electrophysiology studies (EPS) and catheter ablation, electrophysiologists can identify and treat arrhythmias by mapping the electrical pathways within the heart and selectively removing or isolating problematic areas.
Together, cardiac pacing and electrophysiology are essential tools in the treatment of heart rhythm disorders, improving outcomes for millions of patients worldwide. With rapid advancements in technology and therapeutic options, cardiac pacing and electrophysiology continue to evolve, providing more precise and less invasive solutions for managing arrhythmias.
Causes and Risk Factors of Cardiac Arrhythmias
Arrhythmias can arise from a wide range of causes and risk factors, from underlying heart diseases to lifestyle choices. Understanding these risk factors helps with early detection and timely intervention.
1. Underlying Heart Conditions
-
Coronary Artery Disease: Blockage or narrowing of the heart's arteries, often leading to heart attacks and disrupting the heart's electrical system.
-
Heart Failure: When the heart is unable to pump blood efficiently, it can alter electrical conduction, leading to arrhythmias.
-
Valvular Heart Disease: Damaged or diseased heart valves can affect blood flow and electrical pathways, triggering arrhythmias.
-
Hypertension (High Blood Pressure): Chronic high blood pressure can cause structural changes in the heart, leading to arrhythmias.
-
Congenital Heart Defects: Some individuals are born with structural abnormalities in their heart's electrical pathways, predisposing them to arrhythmias.
2. Electrolyte Imbalances
-
Low or high levels of potassium, calcium, or magnesium in the blood can interfere with the heart's electrical impulses, triggering arrhythmias.
-
Imbalances often result from conditions like kidney disease, dehydration, or medication use.
3. Medications
-
Certain drugs, including antiarrhythmic medications, diuretics, and antidepressants, can cause or worsen arrhythmias.
-
Stimulants (like caffeine, nicotine, and recreational drugs) can also provoke arrhythmias.
4. Lifestyle Factors
-
Excessive Alcohol Consumption: Can cause atrial fibrillation and other arrhythmias.
-
Smoking: Damages blood vessels and raises blood pressure, increasing arrhythmia risk.
-
Obesity: Increases the likelihood of hypertension, heart failure, and arrhythmias.
-
Physical Inactivity: Weakens the heart muscle and impairs circulation, making arrhythmias more likely.
5. Genetics
-
Inherited Arrhythmia Syndromes: Conditions such as long QT syndrome, Brugada syndrome, and familial atrial fibrillation predispose individuals to arrhythmias from a young age.
6. Other Risk Factors
-
Age: The risk of arrhythmias increases with age due to natural wear and tear on the heart's electrical system.
-
Chronic Stress: Increased adrenaline from prolonged stress can trigger arrhythmias.
Symptoms and Signs of Cardiac Arrhythmias
The symptoms of arrhythmias vary depending on the type of arrhythmia, its severity, and how long it lasts. Symptoms can range from mild to severe and can sometimes be life-threatening.
1. Common Symptoms
-
Palpitations: The feeling of a fast, fluttering, or pounding heartbeat, especially during rest or physical activity.
-
Dizziness or Lightheadedness: Occurs when the heart fails to pump blood effectively.
-
Fatigue: Chronic fatigue from poor circulation due to arrhythmias.
-
Shortness of Breath: Often occurs with tachycardia (rapid heart rate) or heart failure.
-
Chest Pain or Discomfort: May indicate a heart attack or severe arrhythmia, particularly ventricular tachycardia or atrial fibrillation.
2. Severe Symptoms
-
Fainting (Syncope): A sudden loss of consciousness due to insufficient blood flow to the brain.
-
Swelling in the Legs, Abdomen, or Neck: Indicates poor circulation and heart failure.
-
Sudden Cardiac Arrest: A life-threatening emergency caused by a ventricular arrhythmia, where the heart stops beating.
Diagnosis of Cardiac Arrhythmias
Diagnosing arrhythmias involves a combination of clinical assessment, electrophysiology testing, and imaging studies.
1. Medical History & Physical Examination
-
Symptoms Review: Understanding the frequency, duration, and severity of palpitations, dizziness, or fainting episodes.
-
Physical Exam: Checking for signs like swollen legs, irregular pulse, or heart murmurs.
2. Electrocardiogram (ECG or EKG)
-
The first and most common test to assess the electrical activity of the heart. It records the heart rate, rhythm, and electrical impulses.
-
Variations in the ECG can pinpoint specific arrhythmias such as atrial fibrillation, ventricular tachycardia, and heart block.
3. Holter Monitor
-
A portable ECG device worn for 24-48 hours to record the heart's rhythm over time, especially useful for intermittent arrhythmias.
4. Electrophysiology Study (EPS)
-
A minimally invasive test where catheters are inserted into the heart to map electrical signals, identify arrhythmias, and help guide treatment decisions.
5. Echocardiogram
-
An ultrasound of the heart to assess heart function, valve disease, and structural abnormalities.
6. Tilt Table Test
-
Used to diagnose vasovagal syncope and orthostatic hypotension, which can cause fainting episodes.
Treatment Options for Cardiac Arrhythmias
Treatment options depend on the type and severity of the arrhythmia. The goal is to restore normal rhythm, improve symptoms, and prevent complications.
1. Medications
-
Antiarrhythmic Drugs: These control heart rate and rhythm (e.g., amiodarone, flecainide).
-
Beta-Blockers: Reduce heart rate and prevent arrhythmias (e.g., metoprolol).
-
Calcium Channel Blockers: Used to control atrial arrhythmias.
-
Blood Thinners: For patients with atrial fibrillation to reduce stroke risk (e.g., warfarin, apixaban).
2. Cardioversion
-
Electrical Cardioversion: A controlled shock delivered to the heart to restore normal rhythm, especially useful for atrial fibrillation or atrial flutter.
-
Pharmacological Cardioversion: Using antiarrhythmic drugs to restore normal rhythm.
3. Catheter Ablation
-
A procedure where radiofrequency energy or cryotherapy is used to destroy small areas of heart tissue causing abnormal rhythms.
4. Pacemakers
-
Used to treat bradycardia (slow heart rate) or heart block by delivering electrical impulses to the heart to maintain a normal rhythm.
5. Implantable Cardioverter-Defibrillators (ICD)
-
Used for patients at risk of sudden cardiac arrest from ventricular arrhythmias. The ICD detects dangerous arrhythmias and delivers a shock to restore normal rhythm.
6. Surgical Treatment
-
Maze Procedure: A surgical treatment for atrial fibrillation that creates scar tissue to block abnormal electrical signals in the atria.
Prevention and Management of Cardiac Arrhythmias
Prevention focuses on addressing risk factors and adopting healthy lifestyle changes:
-
Regular Exercise: Improves heart health and circulation.
-
Diet: A heart-healthy diet low in salt and rich in fruits, vegetables, and whole grains.
-
Avoiding Stimulants: Limiting caffeine, alcohol, and drugs that can trigger arrhythmias.
-
Managing Stress: Meditation, yoga, or relaxation techniques to prevent arrhythmia episodes.
-
Monitoring Symptoms: Regular ECGs or Holter monitoring if you have been diagnosed with arrhythmias.
-
Medication Adherence: Consistent use of prescribed antiarrhythmic medications or anticoagulants.
Complications of Cardiac Arrhythmias
If left untreated, arrhythmias can lead to:
-
Stroke: Particularly in atrial fibrillation due to blood clots forming in the atria.
-
Heart Failure: Chronic arrhythmias may weaken the heart muscle.
-
Sudden Cardiac Arrest: Caused by ventricular arrhythmias, often requiring an ICD.
-
Venous Thromboembolism: Blood clots can form in the veins due to poor blood circulation, causing deep vein thrombosis (DVT) or pulmonary embolism (PE).
Living with Cardiac Arrhythmias and Implantable Devices
Living with an arrhythmia or device such as a pacemaker or ICD can be managed with lifestyle changes and medical support:
-
Pacemaker/ICD Care: Regular follow-ups for device checks, avoiding strong electromagnetic fields, and understanding how to respond to device alarms.
-
Lifestyle Modifications: Staying active, managing weight, eating a heart-healthy diet, and avoiding smoking.
-
Psychological Support: Living with a chronic arrhythmia or device may cause anxiety or depression. Support groups or counseling can be helpful.
With proper management, patients can continue to lead a normal, active life.
Top 10 Frequently Asked Questions about Cardiac Pacing and Electrophysiology
1. What is cardiac pacing?
Cardiac pacing refers to the use of a pacemaker device to regulate the heart's rhythm. A pacemaker is a small device implanted under the skin that sends electrical impulses to the heart to maintain a regular heart rate. It is typically used for patients with bradycardia (slow heart rate) or other arrhythmias (irregular heart rhythms).
2. What is electrophysiology?
Electrophysiology is the study of the electrical activity of the heart. It involves diagnosing and treating arrhythmias (abnormal heart rhythms) through procedures like electrophysiology studies (EPS) and ablation. This branch of cardiology helps identify the root causes of arrhythmias and offers treatments to restore a normal heart rhythm.
3. How does a pacemaker work?
A pacemaker is a small device that monitors the heart's natural rhythm and sends electrical impulses when necessary to maintain a regular heartbeat. It can be set to pace the heart at a specific rate or respond to the heart's natural electrical signals. It is typically implanted under the skin near the collarbone and connected to the heart via leads (wires).
4. Who needs a pacemaker or electrophysiology procedure?
A pacemaker may be needed for individuals who experience:
-
Bradycardia (slow heart rate)
-
Heart block (a condition where electrical signals are delayed or blocked in the heart)
-
Atrial fibrillation or other arrhythmias
Electrophysiology procedures, including ablation, may be recommended for individuals with: -
Supraventricular tachycardia (SVT)
-
Atrial fibrillation (AFib)
-
Ventricular arrhythmias
A cardiologist or electrophysiologist will evaluate the patient's symptoms, heart condition, and overall health to determine the need for treatment.
5. What is an electrophysiology study (EPS)?
An electrophysiology study (EPS) is a diagnostic procedure used to evaluate the electrical activity of the heart. During this study, thin catheters are inserted through blood vessels and positioned inside the heart to record electrical signals and identify abnormal pathways or areas causing arrhythmias. EPS helps guide treatment options, including ablation or the placement of a pacemaker.
6. What is cardiac ablation, and when is it used?
Cardiac ablation is a procedure used to treat certain arrhythmias by destroying or isolating the abnormal electrical pathways in the heart. It is often performed after an electrophysiology study to treat conditions like atrial fibrillation, supraventricular tachycardia, or ventricular arrhythmias. The procedure involves using heat (radiofrequency) or cold (cryoablation) to destroy the abnormal tissue causing the arrhythmia.
7. What are the risks and complications of pacemaker implantation or electrophysiology procedures?
Both pacemaker implantation and electrophysiology procedures are generally safe, but there are risks, including:
-
Infection at the implantation site
-
Bleeding or bruising
-
Damage to blood vessels or the heart
-
Blood clots leading to stroke (in rare cases)
-
Device malfunction or lead displacement
-
Reaction to anesthesia
Your cardiologist will discuss these risks and take measures to minimize complications.
8. What is the recovery time after a pacemaker implant or electrophysiology procedure?
-
Pacemaker implantation: Most patients can go home the same day or after an overnight stay. Activity restrictions (e.g., no lifting or strenuous activity for a few weeks) are typically recommended to allow the device to settle.
-
Electrophysiology procedures (including ablation): Recovery typically takes a few days to a week. Most patients can resume normal activities within 1-2 weeks. Follow-up appointments are essential to check for complications or necessary adjustments to the device or treatment.
9. How long does a pacemaker last, and how is it maintained?
A pacemaker typically lasts 5 to 15 years depending on the model and how often it is used. Regular follow-ups are essential to monitor the battery life, device settings, and the heart's response. Pacemakers are programmed and adjusted during these visits to ensure optimal function. If the battery runs low or the device needs adjustment, it may need to be replaced.
10. Can I live a normal life with a pacemaker or after an electrophysiology procedure?
Yes, most patients with a pacemaker or those who have undergone electrophysiology procedures can lead a normal, active life. While certain restrictions, like avoiding heavy lifting or strenuous activities immediately after surgery, may apply, most people return to normal routines, including work, exercise, and daily activities. It's essential to follow your doctor's advice, attend regular check-ups, and avoid activities that might interfere with the pacemaker, such as using strong electromagnetic fields.


