Introduction to Retinal Detachment
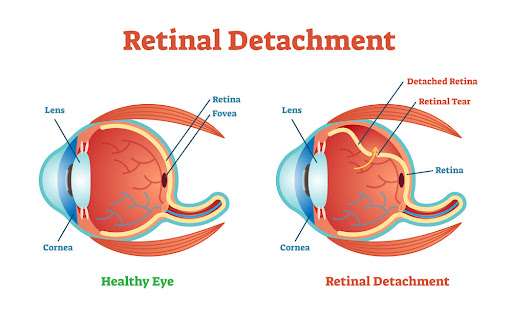
Retinal detachment is a medical emergency that occurs when the retina, a light-sensitive tissue at the back of the eye, detaches from its underlying supportive tissue. The retina is crucial for vision as it converts light into electrical signals that are sent to the brain. A detached retina can result in permanent vision loss if not treated promptly.
Retinal detachment can lead to partial or complete vision loss in the affected eye, and often, the condition worsens if left untreated. Early intervention, however, can result in good recovery and preserved vision.
The Retina and Its Function
The retina is located at the back of the eye and acts like the film in a camera, receiving light and sending images to the brain. The retina contains cells that are sensitive to light, known as photoreceptor cells. These cells help transform light signals into electrical impulses, which travel through the optic nerve to the brain for processing.
When the retina detaches, it is no longer able to function properly, leading to a loss of vision. The condition is often caused by a tear or hole in the retina, through which fluid can seep underneath, causing the retina to pull away from its supporting tissue.
Why Retinal Detachment Requires Immediate Attention
Retinal detachment is considered a sight-threatening emergency, as it can result in complete vision loss within days if not treated. If a detachment is detected early and reattached surgically, it is possible to restore vision, especially if the central part of the retina (the macula) is not severely affected.
Causes and Risk Factors for Retinal Detachment
Retinal detachment can occur due to various factors, ranging from age-related changes in the eye to underlying medical conditions. Understanding the causes and risk factors can help individuals take preventive measures or recognize early signs of the condition.
Causes of Retinal Detachment
-
Aging: As individuals age, the vitreous gel that fills the eye naturally shrinks and pulls away from the retina. This process, called posterior vitreous detachment (PVD), can lead to retinal tears, which are the precursor to retinal detachment.
-
Retinal Tears or Holes: Tears or holes in the retina allow the fluid from the vitreous to seep underneath, leading to detachment. These tears are usually caused by the pulling of the vitreous gel on the retina.
-
Vitreous Degeneration: Over time, the vitreous gel may break down or become more liquefied, increasing the chances of it pulling away from the retina and causing tears.
-
Trauma or Eye Injury: Any injury to the eye or head, such as a blow to the face or a car accident, can cause retinal tears or detachment. Sports-related injuries are also a common cause of retinal detachment, particularly in high-contact sports.
-
Diabetic Retinopathy: In patients with diabetes, the high blood sugar levels cause damage to the blood vessels in the retina. This damage can lead to the growth of scar tissue, which can pull the retina and cause it to detach.
-
Inflammation in the Eye: Conditions such as uveitis (inflammation of the middle layer of the eye) can lead to scarring and retinal detachment.
-
Genetic Conditions: Certain inherited disorders, such as Marfan syndrome, Stickler syndrome, and Ehlers-Danlos syndrome, increase the risk of retinal detachment due to abnormalities in the eye's connective tissues.
Risk Factors for Retinal Detachment
-
Myopia (Nearsightedness): People who are severely nearsighted (high myopia) are at a higher risk of retinal detachment due to the shape of their eyes and the increased likelihood of retinal tears.
-
Family History: A family history of retinal detachment can significantly increase the risk of the condition. Those with relatives who have had retinal detachment are more likely to develop it themselves.
-
Previous Retinal Detachment: If one eye has experienced retinal detachment, the risk of detachment in the other eye is higher.
-
Eye Surgery: People who have undergone cataract surgery or other eye surgeries may have an increased risk of retinal detachment.
-
Advanced Age: The risk of retinal detachment increases with age, particularly after 50, due to natural changes in the vitreous gel and the retina.
Symptoms and Signs of Retinal Detachment
Retinal detachment often presents with sudden and alarming symptoms. It is important to recognize these symptoms early, as prompt treatment can save vision.
Early Symptoms of Retinal Detachment:
-
Sudden Appearance of Floaters: Floaters are tiny specks or cobweb-like shapes that float across your field of vision. These are common and can be associated with retinal tears or detachment.
-
Flashes of Light: Flashes of light, especially in the peripheral vision, are another early warning sign of retinal detachment. This can occur due to the vitreous gel tugging on the retina.
-
Loss of Peripheral Vision: A shadow or curtain-like effect may form in your peripheral vision, indicating that the retina is detaching.
-
Blurred Vision: Vision may become blurry in one eye, particularly if the macula (the center of the retina responsible for sharp vision) becomes affected.
-
Dark or Shadowy Area in Vision: A significant symptom of retinal detachment is the feeling that a dark or shadowy area is moving across the vision, often from the side to the center of the eye.
Advanced Symptoms:
If the retinal detachment progresses, the vision loss can become more pronounced and involve the central visual field. Without prompt treatment, vision loss can become permanent.
Diagnosis of Retinal Detachment
Early and accurate diagnosis of retinal detachment is crucial to prevent permanent vision loss. Ophthalmologists use a combination of patient history, symptom assessment, and specialized eye examinations to confirm the condition.
Ophthalmologic Evaluation
-
Visual Acuity Testing: Determines baseline vision and monitors postoperative outcomes.
-
Pupil Examination: Checks for afferent pupillary defect if macula is involved.
-
Slit-Lamp Examination: With dilated pupils, allows detailed view of the vitreous, retina, and retinal tears.
-
Indirect Ophthalmoscopy: Gold standard for detecting retinal tears and detachment.
-
Scleral Depression: Helps visualize peripheral retina.
Imaging Studies
-
Optical Coherence Tomography (OCT): Detects subtle macular detachments.
-
Ultrasound B-Scan: Used when vitreous hemorrhage obscures direct visualization.
-
Fundus Photography: Documentation and follow-up of retinal status.
Timely diagnosis allows urgent surgical planning to prevent permanent vision loss.
Treatment Options for Retinal Detachment
Retinal detachment is a medical emergency that requires immediate intervention to prevent permanent vision loss. The treatment options for retinal detachment are primarily focused on reattaching the retina to its normal position and ensuring the preservation of vision. Below are the common treatment options available for retinal detachment:
1. Scleral Buckling Surgery
A scleral buckle is a flexible band placed around the eye to gently push the eye wall toward the detached retina. This helps close the tear or hole, allowing the retina to reattach. The surgery may also involve the use of cryotherapy (freezing) or laser to seal the retina.
2. Vitrectomy
In a vitrectomy, the surgeon removes the vitreous gel from the eye and replaces it with a gas bubble or silicone oil. The gas bubble holds the retina in place while it reattaches. This procedure is often used for more severe or complex cases of retinal detachment.
3. Pneumatic Retinopexy
This procedure involves injecting a gas bubble into the eye to push the retina back into place. It is typically used for small detachments and requires laser or cryotherapy to seal any retinal tears or holes.
4. Laser Therapy (Photocoagulation)
Laser therapy is often performed after surgery to ensure the retina remains attached. The laser is used to create small burns around the tear or hole, which helps seal the retina to the underlying tissue.
Prevention and Management of Retinal Detachment
While not all cases of retinal detachment can be prevented, certain steps can reduce the risk, especially for those at higher risk due to factors like age, myopia, or previous eye injuries. Early diagnosis and prompt treatment are crucial in managing the condition effectively. Here, we'll discuss prevention strategies as well as approaches for managing retinal detachment once diagnosed.
Prevention Tips:
-
Regular Eye Exams: Early detection is key, especially for those at higher risk due to age or medical history.
-
Protective Eyewear: Wear sunglasses to protect the eyes from UV light, and use protective glasses during activities that might cause eye injury.
-
Control Medical Conditions: Managing conditions like diabetic retinopathy or high myopia can reduce the risk of retinal detachment.
-
Prompt Treatment of Retinal Tears: If retinal tears are diagnosed early, laser treatment or cryotherapy can help prevent detachment.
Managing Retinal Detachment:
-
Follow-up Care: After surgery, regular follow-up visits are essential to ensure the retina stays attached and that complications do not arise.
-
Avoiding Pressure on the Eye: After surgery, patients are often advised to avoid activities that can increase pressure in the eye, such as heavy lifting or vigorous exercise.
Complications of Retinal Detachment
Retinal detachment is a serious medical condition that occurs when the retina, the thin layer of tissue at the back of the eye, separates from its underlying support tissue. If left untreated, retinal detachment can lead to permanent vision loss. Various complications can arise from this condition, some of which include:
Early Complications
-
Re-detachment
-
Infection (endophthalmitis)
-
Hemorrhage
-
Elevated intraocular pressure
-
Inflammation
Late Complications
-
Cataract formation (especially after vitrectomy)
-
Macular pucker (epiretinal membrane formation)
-
Persistent visual field defects
-
Permanent vision loss if macula was involved or detachment prolonged
Complications underscore the importance of early treatment and careful postoperative follow-up.
Living with the Condition of Retinal Detachment
Recovery after retinal detachment surgery varies from patient to patient. Post-surgical care is crucial to ensure the best possible outcome. Here are some factors to consider:
Post-Surgery Care:
-
Positioning: Patients may be asked to maintain a specific head position to allow the gas bubble (used in vitrectomy or pneumatic retinopexy) to keep the retina in place.
-
Avoiding Physical Strain: Patients should avoid heavy lifting and strenuous activities for a few weeks after surgery.
-
Follow-Up Appointments: Regular visits to the ophthalmologist are critical for monitoring the healing process and ensuring the retina remains attached.
-
Vision Recovery: Full recovery may take weeks or months, depending on the severity of the detachment and the type of surgery performed.
Adjusting to Vision Changes:
After surgery, patients may need time to adjust to their new vision. Some may experience temporary vision blurriness, which can gradually improve. If cataracts or other vision issues arise after surgery, additional treatments may be needed.
Top 10 Frequently Asked Questions about Retinal Detachment
1. What is Retinal Detachment?
Retinal detachment occurs when the retina, the light-sensitive layer at the back of the eye, pulls away from its normal position. This detachment can cause vision problems, as the retina is responsible for sending visual signals to the brain. It requires immediate medical attention to prevent permanent vision loss.
2. What Are the Causes of Retinal Detachment?
The primary cause of retinal detachment is often age-related changes in the eye, such as the shrinking of the vitreous gel inside the eye. Other causes include trauma or injury to the eye, severe nearsightedness (myopia), previous eye surgeries (like cataract surgery), and certain medical conditions like diabetic retinopathy.
3. What Are the Symptoms of Retinal Detachment?
Common symptoms of retinal detachment include a sudden increase in floaters (small spots or lines in your field of vision), flashes of light, or a shadow or curtain-like effect over a part of your vision. These symptoms may be signs of a retinal tear or detachment, and immediate medical consultation is necessary.
4. How is Retinal Detachment Diagnosed?
Retinal detachment is diagnosed through a comprehensive eye examination. The doctor may use a special eye exam called funduscopy, which allows them to view the retina. They may also use imaging tests such as ultrasound or optical coherence tomography (OCT) to get a detailed view of the retina and confirm the detachment.
5. What Are the Treatment Options for Retinal Detachment?
The treatment for retinal detachment depends on its severity and type. The most common treatments are:
-
Laser Surgery: To seal retinal tears before detachment occurs.
-
Cryopexy (Freezing): A technique used to treat small retinal tears.
-
Pneumatic Retinopexy: A gas bubble is injected into the eye to help reattach the retina.
-
Scleral Buckling: A procedure where a silicone band is placed around the eye to push the retina back into place.
-
Vitrectomy: Surgical removal of the vitreous gel and replacement with a gas or silicone oil to reattach the retina.
6. Is Retinal Detachment Preventable?
While retinal detachment cannot always be prevented, certain risk factors can be managed. Regular eye exams, especially for individuals at higher risk (like those with a family history, high myopia, or diabetes), can help detect issues early. Wearing protective eyewear during physical activities and seeking prompt treatment for any eye injuries can also reduce the risk.
7. Can Retinal Detachment Lead to Permanent Vision Loss?
If left untreated, retinal detachment can lead to permanent vision loss in the affected eye. The longer the retina remains detached, the higher the risk of permanent damage. Early diagnosis and treatment are crucial for preventing severe vision loss.
8. What is the Recovery Time After Retinal Detachment Surgery?
Recovery time varies depending on the type of surgery performed. After procedures like pneumatic retinopexy or vitrectomy, patients may need to remain in a specific head position for a period to help the retina reattach. Vision recovery can take several weeks to months, and patients may need to follow up regularly with their eye doctor to monitor healing progress.
9. What Are the Risks or Complications of Retinal Detachment Surgery?
Although retinal detachment surgery is generally safe, there are risks involved. Potential complications include:
-
Infection or bleeding inside the eye.
-
Cataract formation, particularly after vitrectomy.
-
Increased eye pressure or glaucoma.
-
Retinal re-detachment, which may require additional surgeries.
10. Can Retinal Detachment Affect Both Eyes?
Retinal detachment typically affects one eye, but it is possible for the condition to occur in both eyes, either simultaneously or at different times. If you've had retinal detachment in one eye, your risk of developing it in the other eye is increased, and your eye doctor may recommend regular monitoring.


