Introduction to Knee Joint Replacement
Knee joint replacement is a surgical procedure designed to relieve pain and improve function in a knee joint that has been damaged by arthritis, injury, or other degenerative conditions. The knee joint is a complex structure where the femur (thigh bone), tibia (shin bone), and patella (kneecap) come together to allow smooth movement. When the cartilage that cushions these bones wears down due to age, wear-and-tear, or disease (such as osteoarthritis or rheumatoid arthritis), it can lead to severe pain, stiffness, and loss of mobility.
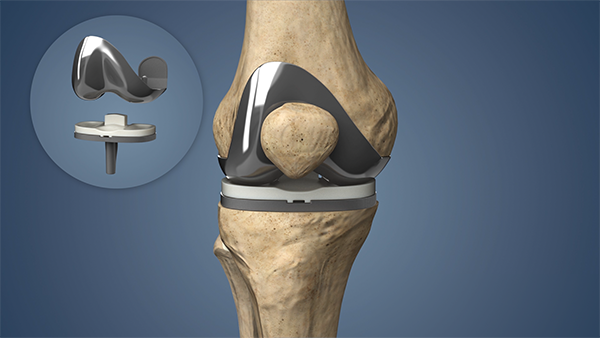
In knee joint replacement surgery, the damaged portions of the knee are removed and replaced with artificial components made from metal, plastic, and ceramic materials. These prosthetic components are designed to mimic the natural movement of the knee, reducing pain and improving mobility. The procedure is typically recommended when other non-surgical treatments, such as physical therapy, medications, or injections, no longer provide relief. Knee joint replacement can be performed in one of two ways: a total knee replacement (TKA), where the entire knee joint is replaced, or a partial knee replacement (PKR), where only the damaged portion of the knee is replaced.
While knee replacement surgery has become increasingly common and highly successful, it is generally recommended for individuals who are experiencing significant pain, have limited function, and have not responded to conservative treatments. With advancements in surgical techniques, including minimally invasive options and robotic-assisted procedures, knee joint replacement has become safer, with shorter recovery times and better long-term outcomes, allowing many patients to return to their normal activities and enjoy an improved quality of life.
Causes and Risk Factors for Knee Joint Replacement
The need for knee replacement is often the result of chronic knee pain or dysfunction that does not improve with conservative treatments. Several factors can lead to knee joint damage, and these factors often worsen over time, making surgery necessary. Below are the primary causes and risk factors for knee joint replacement surgery.
Causes of Knee Joint Damage
The need for knee replacement typically arises due to knee joint degeneration caused by various conditions, with the most common being osteoarthritis. Below are some of the main causes:
1. Osteoarthritis (OA)
Osteoarthritis is the most common cause of knee pain and joint damage in adults, particularly those over 50. In OA, the cartilage that cushions the knee joint gradually deteriorates, causing pain, stiffness, and limited range of motion. As the cartilage wears away, the bones may rub against each other, leading to further damage and inflammation.
2. Rheumatoid Arthritis (RA)
Rheumatoid arthritis is an autoimmune disease that causes inflammation in the joints, including the knee. Over time, the inflammation can damage the cartilage, leading to deformities and pain. RA can affect both knees and is a common reason for early knee replacement surgery.
3. Post-Traumatic Arthritis
This type of arthritis develops after an injury, such as a knee fracture or torn ligaments. Even after the injury heals, the cartilage may not repair properly, leading to post-traumatic arthritis and the need for knee replacement.
4. Knee Injuries
Severe knee injuries, such as a torn ligament or meniscus, can result in long-term joint instability and degeneration, ultimately requiring knee replacement. These injuries often lead to cartilage damage that cannot heal on its own.
5. Abnormal Knee Alignment
Conditions such as bow-leggedness (genu varum) or knock-knees (genu valgum) can lead to uneven wear on the knee joint, increasing the risk of developing arthritis in the knee and ultimately requiring a knee replacement.
Risk Factors for Knee Joint Replacement
Several factors increase the likelihood of needing knee replacement surgery. These include:
-
Age: Older individuals are more likely to develop knee arthritis due to the natural wear and tear of the joint over time.
-
Obesity: Excess weight puts added stress on the knee joint, accelerating wear and tear.
-
Family History: Genetics can play a role in the development of knee arthritis and the need for joint replacement.
-
Gender: Women are more likely to develop osteoarthritis and require knee replacement, especially after menopause.
-
Previous Knee Injury: People who have had knee fractures or ligament tears are at a higher risk for developing arthritis in the joint.
Symptoms and Signs of Knee Joint Damage
The decision to undergo knee replacement surgery is usually based on the severity of symptoms and the impact on daily life. Key symptoms that indicate the need for knee replacement surgery include:
1. Chronic Knee Pain
Persistent knee pain that does not improve with rest, medications, or physical therapy is one of the primary signs that knee replacement may be necessary. This pain often worsens with activity, such as walking or climbing stairs, and may be present even during rest or at night.
2. Limited Range of Motion
As the knee joint deteriorates, it becomes harder to bend or straighten the knee fully. This can make simple activities like getting in and out of a car or sitting and standing difficult.
3. Swelling and Inflammation
Ongoing swelling and inflammation around the knee joint are common in individuals with arthritis. This swelling can make the knee feel warm to the touch and may restrict movement.
4. Knee Deformity
In some cases, the knee joint may become misaligned due to arthritis or injury. This can cause the knee to appear deformed, such as being bow-legged or knock-kneed, making it difficult to walk properly.
5. Instability and Weakness
Many patients report that their knee feels unstable or may "give out" when standing or walking. This instability is often due to the weakening of the muscles around the knee joint, caused by long-term wear and tear.
Diagnosis of Knee Joint Issues
Before knee replacement surgery is recommended, a comprehensive evaluation is conducted to assess the condition of the knee and determine the extent of the damage. This process includes:
1. Physical Examination
A physician will examine the knee to check for signs of damage, such as tenderness, swelling, or deformities. They will assess the knee's range of motion, stability, and alignment.
2. Imaging Tests
-
X-rays: The most common imaging test used to evaluate the extent of damage to the knee joint. X-rays can show how much the cartilage has worn away and whether the bones are rubbing against each other.
-
MRI or CT scans: These tests may be used for a more detailed view of the knee's soft tissues, including cartilage, ligaments, and tendons.
3. Medical History Review
The physician will discuss your medical history, including any past injuries, surgeries, or existing conditions such as arthritis or previous knee trauma. They will also assess your general health to ensure that you are fit for surgery.
Treatment Options for Knee Joint Replacement
Knee joint replacement surgery is a common and effective procedure for individuals experiencing severe knee pain, often due to conditions like osteoarthritis, rheumatoid arthritis, or traumatic knee injuries. The goal of the surgery is to relieve pain, improve mobility, and restore function in the knee. Here are the main treatment options for knee joint replacement:
1. Non-Surgical Treatment Options
Before opting for knee replacement surgery, several non-invasive treatments can be explored to manage knee pain and improve function.
-
Physical Therapy: A physical therapist can design a customized exercise program to strengthen the muscles around the knee and improve flexibility and range of motion.
-
Medications: Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage pain and inflammation.
-
Corticosteroid Injections: These injections provide temporary relief by reducing inflammation in the knee joint.
-
Hyaluronic Acid Injections: This treatment involves injecting a gel-like substance into the knee to lubricate the joint and reduce friction, improving mobility and reducing pain.
-
Braces or Supports: Using knee braces or other assistive devices, such as canes, can help alleviate stress on the knee joint and improve stability.
2. Surgical Treatment Options
If non-surgical treatments do not provide relief, knee replacement surgery may be recommended. There are different types of knee replacement procedures:
-
Total Knee Replacement (TKR): This is the most common type of knee replacement surgery, where the entire knee joint is replaced with a prosthetic implant. It is ideal for patients with advanced arthritis or significant knee damage.
-
Partial Knee Replacement: This procedure replaces only the damaged portion of the knee joint, preserving the healthy parts. It is suitable for patients with limited knee damage and can offer a quicker recovery.
-
Robotic-Assisted Knee Replacement: Robotic surgery allows for greater precision in implant placement, leading to improved outcomes and faster recovery times. This technique is becoming increasingly popular for its ability to provide more accurate alignments.
-
Revision Knee Replacement: In cases where a previous knee replacement has failed, a revision surgery may be necessary to replace the original prosthetic implant.
Prevention and Management of Knee Joint Damage
Preventing and managing knee joint damage involves a combination of lifestyle changes, targeted exercises, protective strategies, and, when necessary, medical interventions. Here are evidence-based approaches for both prevention and management as of 2025.
1. Maintain a Healthy Weight
Carrying excess weight puts more stress on the knee joints, accelerating wear and tear. Maintaining a healthy weight can help protect your knees.
2. Regular Exercise
Engage in low-impact exercises like swimming, walking, or cycling to keep the muscles around the knee strong without putting undue stress on the joint.
3. Proper Posture and Ergonomics
Be mindful of your posture when sitting, standing, and walking. Proper ergonomics can reduce stress on the knees and prevent further damage.
4. Healthy Diet
A balanced diet rich in nutrients, especially those that support bone and joint health, such as calcium and vitamin D, can help maintain healthy cartilage and bone.
Complications of Knee Joint Replacement
Knee joint replacement is generally successful, but like any major surgery, it carries a risk of complications. The most common and significant complications include blood clots, infection, implant loosening, wear, instability, nerve damage, and ongoing pain.
1. Infection
Infection at the surgical site is a risk after knee replacement surgery. Patients are typically given antibiotics before and after the procedure to reduce this risk.
2. Blood Clots
Blood clots, especially in the legs (deep vein thrombosis), can form after surgery. Patients are usually prescribed blood thinners and encouraged to move the legs frequently to reduce the risk.
3. Implant Problems
While rare, knee implants can wear out or become loose over time, requiring revision surgery.
4. Nerve or Blood Vessel Damage
Nerve or blood vessel damage during surgery is a rare but serious complication that can result in permanent numbness or weakness.
5. Persistent Pain or Stiffness
Some patients may experience ongoing discomfort or limited movement after surgery, despite the procedure's success.
Living with Knee Joint Replacement
After knee replacement surgery, most patients experience significant pain relief and improvement in function. However, recovery is a gradual process, and the following steps are crucial for successful rehabilitation:
-
Hospital Stay: Most patients stay in the hospital for 1–2 days after surgery. During this time, they will begin physical therapy to start regaining knee mobility.
-
Physical Therapy: Physical therapy plays a crucial role in recovery. It helps patients regain strength, mobility, and flexibility in the knee joint. Therapy typically begins within 24 hours of surgery.
-
Resuming Normal Activities: Most patients can resume light daily activities within a few weeks. However, it may take several months to return to more strenuous activities.
-
Long-Term Care: Regular follow-up appointments with your surgeon are important to monitor the progress of your recovery and the condition of the implant. Maintaining a healthy lifestyle with regular exercise is key to long-term success.
Top 10 Frequently Asked Questions about Knee Joint Replacement
1. What is knee joint replacement surgery, and when is it necessary?
Knee joint replacement surgery, also known as total knee arthroplasty (TKA), is a procedure in which a damaged knee joint is replaced with an artificial one, typically made of metal, plastic, or ceramic. This surgery is typically recommended for individuals with severe osteoarthritis, rheumatoid arthritis, or those who have experienced significant knee trauma that causes chronic pain, stiffness, or disability. If nonsurgical treatments such as medication, physical therapy, or injections have not alleviated pain and the condition severely limits daily activities, knee replacement surgery becomes a viable option.
When is it necessary?
-
Persistent pain even after other treatments
-
Difficulty in performing daily activities such as walking, climbing stairs, or getting out of chairs
-
Limited range of motion or instability in the knee joint
-
Severe damage to the knee joint visible on X-rays or MRI
2. What are the types of knee replacement surgery available?
There are three main types of knee replacement surgery:
-
Total Knee Replacement (TKR): This is the most common type of knee replacement surgery, where the entire knee joint is replaced with an artificial joint. The femur (thigh bone), tibia (shin bone), and patella (kneecap) are all involved.
-
Partial Knee Replacement (PKR): In this procedure, only one part of the knee joint that is damaged is replaced, while the rest of the knee joint is preserved. This is typically recommended for individuals with arthritis limited to a specific compartment of the knee.
-
Unicompartmental Knee Arthroplasty (UKA): This is a form of partial knee replacement that targets only the worn-out compartment of the knee. It's generally recommended for patients who have arthritis in only one area of the knee and still have a good range of motion in the rest of the joint.
3. What is the recovery process like after knee replacement surgery?
The recovery time after knee replacement surgery varies, but on average, patients can expect the following timeline:
-
First Few Days Post-Surgery: Hospital stay (typically 2 to 3 days). Pain management and physical therapy to begin restoring mobility and preventing complications like blood clots.
-
First Few Weeks: Swelling and bruising around the knee may occur, but most patients are encouraged to begin walking with the help of a walker or crutches. Physical therapy plays a crucial role in recovery during this time to improve flexibility and strength.
-
1-3 Months: Many patients can gradually return to daily activities and light work, but high-impact activities should still be avoided.
-
6 Months to a Year: Full recovery, including strengthening of the muscles around the knee and a return to more strenuous activities, may take up to a year. Some patients may still experience mild discomfort during high-intensity activities.
4. How long does knee replacement last?
A knee replacement can last anywhere from 15 to 20 years, depending on factors like the patient's age, activity level, and general health. Modern implants are designed to be durable, but over time, wear and tear can occur, especially in younger, more active individuals. In such cases, revision surgery (replacing the implant) might be required later in life. To ensure a longer lifespan for the implant, it's essential to follow post-surgery care instructions and avoid excessive stress on the joint.
5. What are the potential risks and complications of knee replacement surgery?
Like any major surgery, knee replacement carries some risks and complications, including:
-
Infection: Although rare, infections can occur in the surgical site or deep in the knee joint.
-
Blood Clots: Patients are at risk of developing deep vein thrombosis (DVT) after surgery. Blood-thinning medications and early mobilization are crucial in preventing this.
-
Implant Loosening or Wear: Over time, the artificial knee joint can become loose or wear out, requiring revision surgery.
-
Nerve or Blood Vessel Damage: Although uncommon, there is a risk of nerve or blood vessel injury during the procedure.
-
Stiffness or Range of Motion Problems: Some patients may experience difficulty in achieving the full range of motion post-surgery, which can be improved with physical therapy.
6. How long does the surgery take, and what type of anesthesia is used?
Knee replacement surgery typically lasts about 1 to 2 hours. However, the total time spent in the operating room, including preparation and anesthesia, can extend to 3-4 hours.
-
Anesthesia options include:
-
General Anesthesia: The patient is fully asleep during the procedure.
-
Spinal Anesthesia: The patient is awake but numbed from the waist down.
-
Epidural or Nerve Block: Local anesthesia combined with sedation to reduce pain.
-
Your anesthesiologist will discuss the best option based on your health, medical history, and personal preferences.
7. What should I expect during my hospital stay after surgery?
After surgery, patients typically stay in the hospital for 2-3 days, depending on their recovery progress. During this time, the medical team will monitor vital signs, manage pain, and assist with initial physical therapy. You will be encouraged to start moving as soon as possible to prevent complications like blood clots and to begin strengthening the knee. Early mobilization is key, and you may use assistive devices such as crutches or a walker.
8. When can I return to work and driving after knee replacement surgery?
-
Return to Work: Most patients can return to work in about 4-6 weeks if their job is sedentary. However, those in physically demanding roles may need up to 3 months for full recovery.
-
Driving: Most patients can drive about 4 to 6 weeks post-surgery, as long as they are off pain medications and can move their leg comfortably, especially when operating the brake and accelerator.
9. What activities can I do after knee replacement surgery?
After knee replacement surgery, most patients can return to low-impact activities such as:
-
Walking: A great exercise to improve mobility and strength.
-
Swimming: A low-impact way to enhance flexibility without stressing the knee.
-
Cycling: Once your knee is strong enough, cycling can help with muscle strengthening.
Avoid high-impact activities such as running, jumping, or contact sports, as these can wear out the artificial joint faster.
10. How can I manage pain after knee replacement surgery?
Pain management is an essential part of recovery. In the early stages, pain may be managed with a combination of:
-
Medications: Prescription painkillers, including opioids and nonsteroidal anti-inflammatory drugs (NSAIDs), may be used in the first few weeks.
-
Physical Therapy: Rehab exercises help strengthen muscles, improve flexibility, and reduce pain in the long term.
-
Ice and Elevation: Using ice packs and elevating the leg can help manage swelling and discomfort.
-
Assistive Devices: Crutches or a walker can help take the load off the knee as it heals.


