Introduction to New Treatment in Sight for Ovarian Cancer
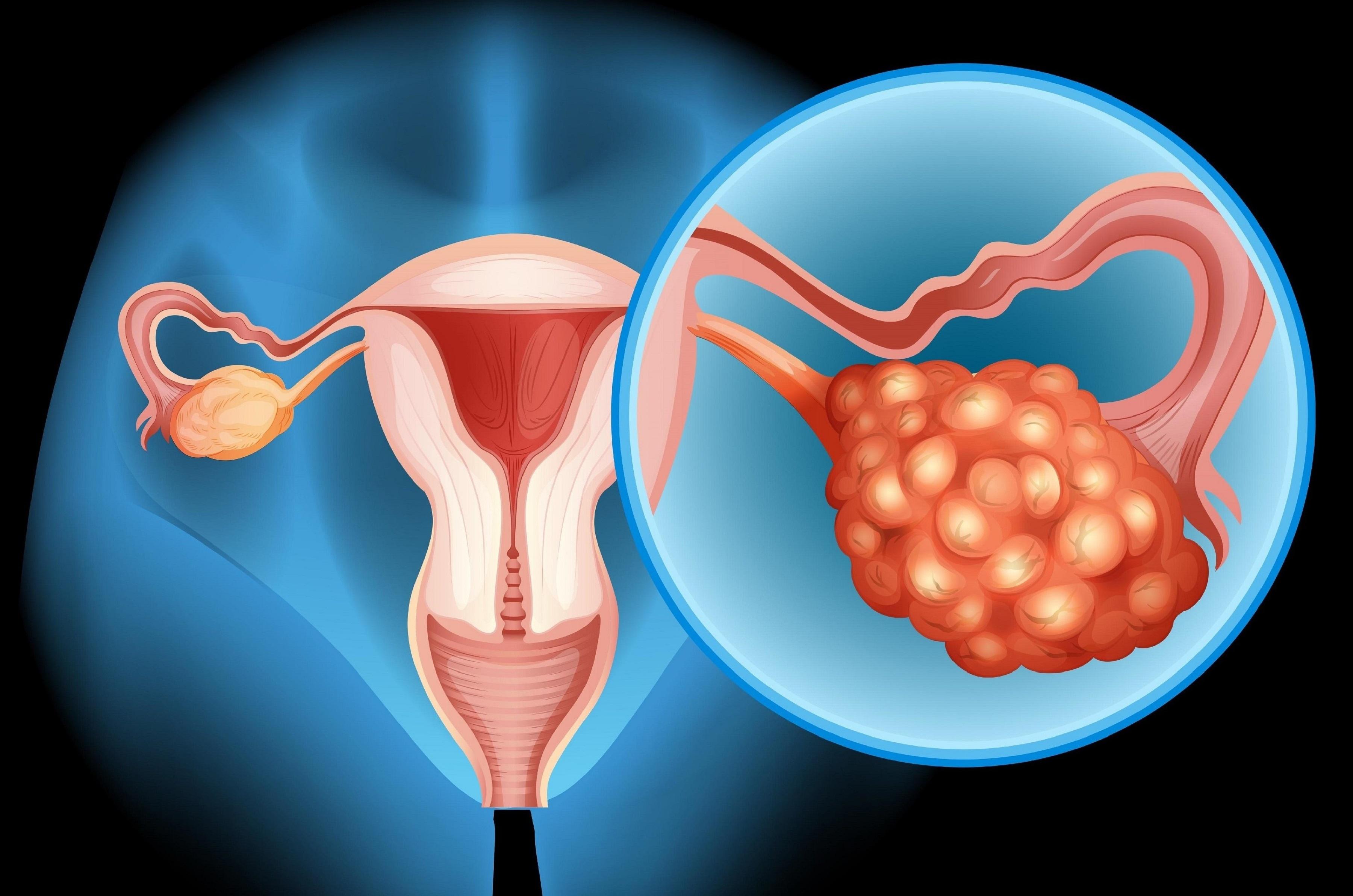
Ovarian cancer is one of the most challenging gynecological malignancies worldwide. Often diagnosed at an advanced stage due to subtle early symptoms, it remains a leading cause of cancer-related deaths in women. However, recent advancements in oncology research have unveiled promising new treatments, which are reshaping management strategies and offering hope to patients.
The new treatments focus on precision medicine, targeted therapy, immunotherapy, and advanced surgical techniques. Unlike conventional chemotherapy, which affects both healthy and cancerous cells, these innovative approaches aim to selectively target cancer cells, reduce side effects, and improve survival rates. With ongoing clinical trials and FDA approvals, the landscape of ovarian cancer treatment is evolving rapidly.
Recent studies highlight the role of molecular profiling, genetic testing, and personalized therapy in tailoring treatment plans for each patient. These advancements are especially critical for patients with platinum-resistant ovarian cancer, who historically had limited options.
Causes and Risk of Ovarian Cancer
Understanding what predisposes an individual to ovarian cancer is crucial—not only for early detection and prevention, but also because many of the same molecular pathways that drive risk may become therapeutic targets in cancer treatment.
Epidemiology & Overview
-
Ovarian cancer is the most lethal gynecologic malignancy globally, largely because it is diagnosed late in many cases.
-
It frequently presents in women after menopause, often in their 50s or 60s, although earlier onset can occur, particularly in hereditary cases.
-
Genetic predisposition plays a significant role: mutations in BRCA1 and BRCA2, and other genes involved in homologous recombination repair, substantially increase lifetime risk.
Risk Factors
Here is a breakdown of known risk factors:
Nonmodifiable / Inherent Factors
-
Genetic mutations / inherited syndromes
BRCA1 and BRCA2 mutations confer markedly higher risk of ovarian (and breast) cancer.
Mutations in other DNA-repair pathway genes (RAD51C, RAD51D, BRIP1, PALB2) may also contribute.
Lynch syndrome (mismatch repair gene defects) may modestly increase risk. -
Age / Menopause
Risk increases with age, especially after menopause.
The more ovulatory cycles a woman has in her lifetime (i.e. early menarche, late menopause), the higher the cumulative risk. -
Family history of ovarian or breast cancer
-
Prior personal cancer history in certain contexts
Modifiable / Environmental / Lifestyle Factors
-
Reproductive history
Nulliparity (never having children) is associated with higher risk.
Later age at first childbirth.
Use of oral contraceptives (combined estrogen-progestin) has been shown to have a protective effect. -
Hormone replacement therapy (HRT)
Long-term estrogen therapy (especially unopposed estrogen) may increase risk. -
Endometriosis (in certain subtypes)
-
Obesity, high BMI, inflammation (some data suggest correlation)
-
Smoking (especially for certain histologic subtypes, e.g. mucinous)
-
Environmental exposures (e.g. talcum powder use near the genital tract, asbestos, etc.), though evidence remains mixed
-
Prior pelvic irradiation (rare)
Molecular & Cellular Underpinnings (Pathogenesis)
Many of the risk factors above translate into molecular vulnerabilities in ovarian cells:
-
Defects in DNA repair / Homologous Recombination Deficiency (HRD):
Many ovarian cancers, especially high-grade serous types, harbor defects in homologous recombination repair (due to BRCA or related genes). These defects make cancer cells more vulnerable to DNA-damaging therapies and PARP inhibitors. -
Genomic Instability & Mutational Burden:
High-grade serous ovarian cancer is notorious for genomic instability, TP53 mutations, copy number alterations, and heterogeneity. -
Oncogenic signaling pathways
Aberrant activation of pathways like PI3K/AKT, RAS / MAPK, and others contribute to uncontrolled growth, survival, and therapy resistance.
In low-grade serous ovarian carcinoma (LGSOC), mutations in KRAS, BRAF, or upstream regulators are frequent, making the MAPK pathway a key driver. -
Tumor Microenvironment & Immune Evasion
Ovarian tumors often cultivate an immunosuppressive microenvironment (regulatory T cells, myeloid-derived suppressor cells) and express immune checkpoints (e.g. PD-L1).
Emerging research identifies cryptic antigens—hidden protein fragments normally not exposed to the immune system—that may be re-expressed in tumor cells and serve as novel immunotherapy targets. -
Resistance mechanisms and clonal evolution
Under therapeutic pressure, resistant subclones can emerge.
Use of liquid biopsy / circulating tumor DNA (ctDNA) is becoming important for tracking resistance.
Because many of the above molecular drivers are actionable, the same factors that contribute to risk and progression are the very ones researchers are targeting in new therapies.
Symptoms and Signs of Ovarian Cancer
Ovarian cancer is notoriously called a “silent disease” because early symptoms are subtle or nonspecific. By the time more overt signs appear, the disease is often already advanced. However, recognizing the warning signs early can lead to better outcomes.
Common Symptoms Clinical Features
-
Abdominal / Pelvic Discomfort
Persistent bloating
Abdominal swelling or distension (ascites)
Early satiety (fullness after eating small amounts)
Pressure or pain in pelvic region -
Gastrointestinal Symptoms
Change in bowel habits (constipation, diarrhea)
Urinary symptoms: increased frequency or urgency
Indigestion, gas, or nausea -
Systemic / Constitutional Symptoms
Unexplained weight loss or gain (especially abdominal girth)
Loss of appetite
Fatigue, low energy
Menstrual irregularities (in premenopausal women) -
Later / Advanced Signs
Ascites causing abdominal distension
Pelvic mass on clinical exam
Back pain or leg swelling (due to spread or lymph node involvement)
Gastrointestinal obstruction (in late disease)
Pleural effusion or respiratory symptoms (if metastasis)
Because these symptoms are common to many benign conditions (e.g. irritable bowel syndrome, gastrointestinal disorders), ovarian cancer is often overlooked or misdiagnosed in early stages.
Red Flag Features That Merit Investigation
-
Symptoms that are new, persistent, and progressive over weeks to months (rather than transient).
-
Combination of multiple symptoms (bloating + early satiety + urinary frequency).
-
Family history of ovarian or breast cancer, or known BRCA mutation carriers.
-
Presence of ascites, unexplained weight gain in the abdominal area, or an adnexal mass on imaging or pelvic exam.
Early detection remains one of the biggest challenges in ovarian cancer, which is why research into better biomarkers and imaging is critical.
Diagnosis of Ovarian Cancer
Diagnosing ovarian cancer is a multistep process involving clinical evaluation, imaging, tissue sampling, and molecular testing. The goal is not only to confirm disease presence, but also to subtype the tumor, assess extent, and identify biomarkers that guide treatment choice.
Clinical & Initial Evaluation
-
Detailed history (symptom onset, risk factors, family/personal cancer history)
-
Physical pelvic and abdominal examination
-
Baseline blood tests: complete blood count, liver/kidney function, CA-125, HE4, and other tumor markers (though none are perfectly sensitive or specific)
Imaging Modalities
-
Transvaginal ultrasound (TVUS): Often the first imaging test to assess ovarian morphology, cysts, or suspicious masses.
-
Contrast-enhanced CT scan (abdomen, pelvis, thorax): To evaluate spread, lymph nodes, ascites, peritoneal implants.
-
MRI (in selected cases) to better characterize masses.
-
PET-CT / PET-CT with FDG: May be useful in selected cases for distant metastases assessment or recurrence.
Surgical / Biopsy Confirmation
-
Laparoscopy / exploratory laparotomy: Provides direct visualization and enables biopsy or tumor debulking with histopathologic assessment.
-
Histopathology is required to classify tumor subtype (serous, endometrioid, clear cell, mucinous, germ cell, etc.).
-
Immunohistochemistry (IHC) and molecular testing help differentiate primary ovarian cancer from metastases, and reveal actionable markers (e.g. BRCA, HRD, microsatellite instability).
Molecular & Genetic Testing
Given the evolving targeted therapy landscape, molecular profiling is increasingly standard:
-
Germline genetic testing (BRCA1/2, HRD genes)
-
Somatic mutation analysis of the tumor (BRCA, TP53, PI3K pathway, KRAS/BRAF in low-grade subtypes)
-
Homologous recombination deficiency (HRD) scoring
-
RNA sequencing / gene expression profiling in research settings
-
Liquid biopsy / ctDNA monitoring in recurrence or resistance scenarios
Emerging Diagnostic Innovations
-
Biomarker panels combining CA125, HE4, CA72.4, other proteins or lipids, sometimes enhanced by machine learning algorithms, can raise sensitivity, especially for early-stage disease.
-
Cryptic antigen discovery: New immunotherapy research has identified cryptic antigens—hidden protein fragments—that may serve as tumor-specific immune targets.
-
Imaging innovations / artificial intelligence: Deep learning-based automated grading and staging, spectroscopic imaging, and other advanced modalities are under investigation.
With diagnosis and tumor characterization in hand, the next step is treatment—especially newer, cutting-edge options.
Treatment Options: “New Treatments in Sight”
Treatment of ovarian cancer typically involves a multimodal approach — surgery + systemic therapy — but the frontier now lies in integrating targeted therapies, immunotherapies, and smart combinations that exploit tumor biology.
Standard-of-Care Backbone
These remain foundational:
-
Cytoreductive surgery / debulking — aim to remove as much tumor as possible
-
Platinum-based chemotherapy (e.g. carboplatin + paclitaxel)
-
Bevacizumab (anti-VEGF therapy) — extends progression-free survival in some settings
-
PARP inhibitors (e.g. olaparib, niraparib) especially in BRCA-mutated or HRD-positive disease; maintenance therapy after response to platinum is standard in many settings
Yet, limitations exist: acquired resistance, toxicity, and disease relapse.
Emerging & Novel Therapies
Here are some of the most promising new approaches:
1. Avutometinib + Defactinib (for KRAS-mutated Low-Grade Serous Ovarian Cancer)
-
In May 2025, the FDA granted approval for the combination of avutometinib (a MEK inhibitor) with defactinib (a FAK inhibitor) for KRAS-mutated recurrent low-grade serous ovarian cancer (LGSOC) in patients who've had prior therapy.
-
LGSOC is more indolent but is relatively resistant to chemotherapy; it often harbors mutations in the MAPK pathway (KRAS/BRAF).
-
Mechanism: Avutometinib inhibits MEK signaling, and defactinib inhibits focal adhesion kinase (FAK), potentially impairing survival and resistance pathways.
-
In clinical trials (e.g. RAMP-201), patients with measurable disease, prior systemic therapy, and KRAS mutation were treated; results showed meaningful responses and a manageable safety profile.
This is among the first approvals directly aimed at a molecularly defined ovarian cancer subtype beyond the BRCA/HRD paradigm.
2. Antibody-Drug Conjugates (ADCs)
-
Mirvetuximab soravtansine (targeting folate receptor a, or FRa)
This ADC links a monoclonal antibody targeting FRa to a cytotoxic payload.
It is indicated for FRa-positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer after prior treatment(s).
Common side effects include ocular toxicity (keratopathy), fatigue, GI effects, and neuropathy. -
Raludotatug deruxtecan (DS-6000)
An investigational ADC targeting CDH6 (cadherin-6) conjugated to deruxtecan (a topoisomerase I inhibitor).
In 2025 it received Breakthrough Therapy Designation from the FDA for platinum-resistant ovarian, peritoneal, or fallopian tube cancers that express CDH6 and have been treated with bevacizumab.
The ADC strategy allows delivery of potent cytotoxic agents directly to tumor cells expressing the target antigen, minimizing systemic toxicity.
3. Combination Targeted Approaches / Precision Medicine
-
A recent preclinical study from Weill Cornell used a pairing of two experimental agents (not yet named in the public excerpt) to inhibit tumor growth and block drug-induced resistance in genetically diverse ovarian cancer models.
-
The emerging paradigm is shifting from monotherapy to rational combinations that co-target multiple pathways (e.g. angiogenesis + PARP + immunotherapy).
-
Strategies targeting lipid metabolism, small-molecule kinase inhibitors, and gene therapy are also being researched.
4. Immunotherapy & Novel Immune Targets
-
The immunosuppressive tumor microenvironment in ovarian cancer has been a major barrier to checkpoint inhibitor success.
-
Researchers at the Mayo Clinic have identified a new immunotherapy target, a cryptic antigen, which might help the immune system better recognize ovarian tumor cells.
-
Combining immunotherapy with ADCs or targeted agents is an area of active investigation, aiming to overcome immune “cold” tumor challenges.
5. Overcoming Resistance & Biomarker-Guided Switching
-
Monitoring circulating tumor DNA (ctDNA) after treatment can help detect minimal residual disease (MRD) or emerging resistance mutations earlier.
-
Spatial transcriptomic / proteomic assays are being developed to map heterogeneity within tumors and guide targeted therapy to resistant sub-populations.
-
Adaptive therapy strategies seek to switch drugs or combine agents before overt resistance emerges, prolonging effective control.
Choosing the Right Therapy
Key considerations:
-
Tumor subtype (high-grade vs low-grade, epithelial vs non-epithelial)
-
Biomarker status (BRCA mutation, HRD, FRa expression, CDH6, KRAS, etc.)
-
Prior treatment history and resistance patterns
-
Patient's performance status and comorbidities
-
Ongoing clinical trials available
Because the "new treatments in sight" often depend on molecular features, precision medicine / genomic profiling is increasingly essential in decision-making.
Prevention and Management of Ovarian Cancer
While many risk factors are nonmodifiable, there are strategies for risk reduction, early intervention, and management in the disease course.
Prevention and Early Intervention
-
Genetic counseling and testing for individuals with family history or known high-risk genes (e.g. BRCA).
-
Risk-reducing salpingo-oophorectomy (removal of fallopian tubes and ovaries) is highly effective in BRCA mutation carriers after childbearing.
-
Use of oral contraceptives has a protective effect when used long term.
-
Tubal ligation / salpingectomy (removal/ligation of fallopian tubes) may reduce risk, possibly by interrupting pathways of malignant cell migration.
-
Lifestyle modifications: maintaining healthy weight, avoiding smoking, reducing inflammatory exposures.
Management / Control of Disease
-
Close surveillance in high-risk individuals (imaging, biomarker follow-up)
-
Symptom-directed care: addressing pain, ascites, gastrointestinal symptoms
-
Integration of supportive / palliative care early to manage quality-of-life issues
-
Clinical trial enrollment as new therapies mature
-
Switching or combining therapies upon signs of progression
-
Nutrition, physical activity, psychological support to maintain resilience
Given the tendency of ovarian cancer to relapse, management often becomes a chronic, adaptive process rather than a finite cure.
Complications of Ovarian Cancer & Its Treatments
Both the disease and its treatments carry significant risks of complications. Recognizing and managing these is crucial for patient well-being.
Disease-Related Complications
-
Ascites causing abdominal distension, discomfort, early satiety
-
Bowel obstruction from peritoneal carcinomatosis
-
Pleural effusion / respiratory compromise
-
Metastatic spread to liver, lungs, or distant organs
-
Compression of pelvic structures, urinary obstruction
-
Cachexia / weight loss / malnutrition
Treatment-Related Adverse Effects
-
Chemotherapy toxicities: myelosuppression, neuropathy, GI effects, alopecia
-
Bevacizumab (anti-angiogenesis): hypertension, bleeding, GI perforation risk
-
PARP inhibitors: anemia, fatigue, nausea, risk of secondary malignancies (rare)
-
ADCs: off-target toxicities depending on payload (e.g. ocular toxicity, neuropathy)
-
MEK / FAK inhibitors (e.g.avutometinib/defactinib) side effects: fatigue, elevated enzymes, rash, GI symptoms, visual disturbances (based on reported safety profile).
-
Immunotherapy: immune-related adverse events (colitis, pneumonitis, hepatitis, endocrinopathies)
-
Complications of surgery: bleeding, infection, adhesions, bowel injury
Proactive monitoring, dose adjustments, symptomatic management, and multidisciplinary care are critical to mitigate these complications.
Living with Ovarian Cancer (Quality of Life, Survivorship)
A diagnosis of ovarian cancer, especially in advanced or recurrent settings, profoundly affects not just physical health but psychological, social, and emotional domains. As treatments improve and patients live longer, quality of life (QoL) and survivorship care become increasingly important.
Symptom & Side Effect Management
-
Pain control, ascites drainage, antiemetics, nutritional support
-
Monitoring and treating side effects of systemic therapies
-
Rehabilitation / physiotherapy to preserve strength and mobility
Psychological & Social Support
-
Counseling, mental health support, peer support groups
-
Navigating financial, social, and caregiver burdens
-
Support for partners and family members
Lifestyle & Wellness
-
Diet & nutrition tailored to patient tolerance
-
Gentle exercise programs (as feasible)
-
Stress reduction techniques (mindfulness, yoga, meditation)
Follow-up & Surveillance
-
Periodic imaging, tumor marker monitoring, clinical visits
-
Monitoring for late effects of therapy (e.g. organ toxicity)
-
Genetic / hereditary cancer follow-up in familial cases
Hope, Participation & Advocacy
-
Encourage patient engagement in clinical trials, where new options may be available
-
Shared decision-making: balancing benefits vs toxicity
-
Leveraging new diagnostics (liquid biopsy) and new therapies as they become available
Top 10 Frequently Asked Questions about New Treatments for Ovarian Cancer
1. What is the significance of the FDA's approval of Avmapki Fakzynja Co-pack for ovarian cancer?
In May 2025, the U.S. Food and Drug Administration (FDA) granted accelerated approval to Avmapki Fakzynja Co-pack, a combination therapy of avutometinib and defactinib, for the treatment of KRAS-mutated recurrent low-grade serous ovarian cancer (LGSOC) in adults who have received prior systemic therapy. This marks the first FDA-approved treatment for this specific subtype of ovarian cancer, offering a new therapeutic option for patients with limited treatment responses.
2. How does the combination of avutometinib and defactinib work?
Avutometinib is a MEK1/2 inhibitor that disrupts the MAPK signaling pathway, while defactinib is a focal adhesion kinase (FAK) inhibitor that affects cell adhesion and migration. Together, they target key mechanisms involved in tumor growth and metastasis in KRAS-mutated LGSOC, leading to improved patient outcomes.
3. What are the challenges in treating low-grade serous ovarian cancer (LGSOC)?
LGSOC is a rare and indolent subtype of ovarian cancer that often presents at an advanced stage. It is characterized by mutations in the MAPK pathway, including KRAS, BRAF, and ERBB2. These tumors are typically resistant to standard chemotherapy, highlighting the need for targeted therapies like the recently approved combination of avutometinib and defactinib.
4. What other novel therapies are being explored for ovarian cancer?
Researchers are investigating various innovative treatments for ovarian cancer, including:
-
Antibody-Drug Conjugates (ADCs): These therapies deliver cytotoxic agents directly to cancer cells, minimizing damage to healthy tissues. For instance, sofituzumab vedotin targets MUC16, a protein overexpressed in ovarian cancer cells.
-
PARP Inhibitors: Drugs like niraparib have shown significant antitumor activity in metastatic ovarian cancer, particularly in patients with BRCA mutations.
-
Immunotherapies: Investigational treatments targeting immune checkpoints are being tested to enhance the body's immune response against ovarian cancer cells.
5. How does the new blood test improve early detection of ovarian cancer?
A recent study developed a blood test that identifies specific combinations of proteins and lipid molecules shed into the bloodstream by tumor cells. Using machine learning, the test analyzes these biomarkers to detect ovarian cancer with up to 93% accuracy, including early-stage cases. This advancement could lead to earlier diagnosis and better patient outcomes.
6. What is the role of the Cancer Genome and Tissue Bank launched by IIT-Madras?
IIT-Madras has established a Cancer Genome and Tissue Bank aimed at collecting and analyzing genetic and tissue data from Indian cancer patients. This initiative seeks to facilitate the development of personalized cancer therapies tailored to the genetic diversity of the Indian population, potentially leading to more effective treatments for ovarian cancer and other malignancies.
7. What are the potential benefits of combining inavolisib with palbociclib and fulvestrant?
Inavolisib is a selective inhibitor of mutant PI3Ka, and when combined with palbociclib, a CDK4/6 inhibitor, and fulvestrant, an estrogen receptor antagonist, it has shown promise in treating hormone receptor-positive, HER2-negative breast cancer. While primarily studied in breast cancer, this combination approach may offer insights into treating ovarian cancer subtypes with similar molecular profiles.
8. How does the new imaging system 'OVASEEK' aid in early detection?
The OVASEEK imaging system is designed to detect early disease changes in fallopian tubes that standard tests may miss. By identifying subtle alterations at an early stage, this system could enhance early detection rates of ovarian cancer, leading to improved survival outcomes.
9. What is the significance of spatial transcriptomics in ovarian cancer research?
Spatial transcriptomics is a technique that analyzes gene expression within the context of tissue architecture. Recent studies have utilized this method to identify multidrug-resistant phenotypes in ovarian cancer, providing insights into tumor heterogeneity and potential therapeutic targets.
10. What are the prospects for personalized medicine in ovarian cancer treatment?
Advancements in multi-omics data analysis, including genomics, proteomics, and transcriptomics, are paving the way for personalized treatment strategies in ovarian cancer. Machine learning frameworks are being developed to suggest individualized treatment regimens based on a patient's unique molecular profile, potentially improving therapeutic efficacy and patient outcomes.


