Introduction to Rhinoplasty
Rhinoplasty, commonly known as a “nose job,” is a surgical procedure performed to reshape or reconstruct the nose for aesthetic enhancement, functional improvement, or both. It is one of the most popular cosmetic surgeries worldwide, chosen by individuals who are dissatisfied with the size, shape, or symmetry of their nose, or those who suffer from breathing difficulties due to structural abnormalities.
Rhinoplasty can address a variety of concerns: a prominent hump, wide nostrils, crooked nose, bulbous tip, or post-traumatic deformities. Beyond aesthetics, it is also a corrective surgery for conditions such as deviated septum, nasal fractures, or congenital defects that impair breathing.
With advancements in surgical techniques, rhinoplasty has become safer and more precise, with natural-looking results and shorter recovery times. It can be performed as open rhinoplasty (external incision for better visibility) or closed rhinoplasty (incisions inside the nostrils with no external scar).
Causes and Risk of Rhinoplasty
Rhinoplasty, often referred to as a “nose job,” is a surgical procedure designed to reshape or reconstruct the nose. It may be performed for cosmetic reasons to enhance appearance or for functional reasons to correct breathing difficulties and structural abnormalities. While it is one of the most common cosmetic surgeries worldwide, understanding the causes behind why people undergo rhinoplasty and the risks associated with it is essential for anyone considering the procedure.
Causes / Indications for Rhinoplasty
-
Cosmetic Reasons
-
Desire to change the shape, size, or proportions of the nose for better facial harmony
-
Correction of bumps, humps, depressions, asymmetry, or a wide/flat/twisted nose
-
Refinement of the nasal tip, narrowing wide nostrils, or changing angle
-
-
Functional Reasons
-
Correcting nasal airway obstruction caused by a deviated septum, enlarged turbinates, or internal valve collapse
-
Improving breathing difficulties not responsive to medical treatment
-
-
Post-Traumatic or Reconstructive Indications
-
Repair after nasal fractures, accidents, sports injuries, or burns
-
Reconstruction following tumor removal or congenital defects (e.g., cleft lip nose deformity)
-
-
Revision (Secondary) Rhinoplasty
-
Correction of unsatisfactory results or complications from prior nasal surgery
-
Risk Factors Associated with Rhinoplasty
-
Medical Risks
-
Pre-existing health conditions (bleeding disorders, uncontrolled hypertension, diabetes)
-
History of keloid or hypertrophic scarring
-
Smoking (impairs healing, increases risk of infection)
-
-
Surgical Risks
-
Complex or multiple prior nasal surgeries
-
Thin or fragile nasal skin (may affect healing or mask asymmetries)
-
Unrealistic patient expectations
-
-
Psychological Considerations
-
Body dysmorphic disorder or underlying mental health issues may complicate satisfaction
-
Note: The risk profile can be minimized by thorough evaluation, choosing an experienced surgeon, and following preoperative/postoperative instructions.
Symptoms and Signs Indicating Rhinoplasty
Rhinoplasty is not always performed purely for cosmetic reasons. Many patients pursue the procedure because of medical or functional issues that affect breathing, facial balance, or overall health. Recognizing the symptoms and signs that may indicate a need for rhinoplasty helps patients seek timely medical advice and evaluate whether surgery is the right option for them.
Cosmetic Signs
-
Disproportionate nose (too large/small for face)
-
Visible humps or depressions on the bridge
-
Bulbous, droopy, or upturned tip
-
Wide, flared, or asymmetrical nostrils
-
Crooked or twisted nasal structure
Functional Signs
-
Persistent nasal blockage or difficulty breathing (especially after trauma or failed medical management)
-
Snoring or sleep disturbances due to nasal structure
-
Recurrent sinus infections linked to septal deviation
Post-Traumatic or Congenital
-
Nasal deformity following injury (fracture, cartilage collapse)
-
Obvious birth defects (cleft nasal deformity, absent nasal structures)
Revision Needs
-
Unsatisfactory appearance after previous surgery
-
Continued functional problems post-surgery
Warning: Any new nasal deformity, persistent obstruction, or sudden changes in nasal shape after injury should prompt early medical evaluation.
Diagnosis of Rhinoplasty Candidates
Rhinoplasty is not a one-size-fits-all procedure. Identifying suitable candidates requires a comprehensive medical, functional, and psychological evaluation. Surgeons must carefully distinguish between patients who will truly benefit from rhinoplasty and those who may need alternative therapies or counseling. Diagnosis involves a combination of clinical examination, imaging, and patient expectations assessment.
Comprehensive Clinical Evaluation
-
Medical and Surgical History
-
Assess history of trauma, prior surgeries, breathing issues, medical problems
-
-
Physical Examination
-
External assessment: nasal shape, skin type, symmetry, tip, nostrils
-
Internal assessment: septal alignment, turbinates, nasal valves, mucosa
-
Facial analysis: relationship of nose to chin, lips, forehead
-
-
Imaging & Investigations
-
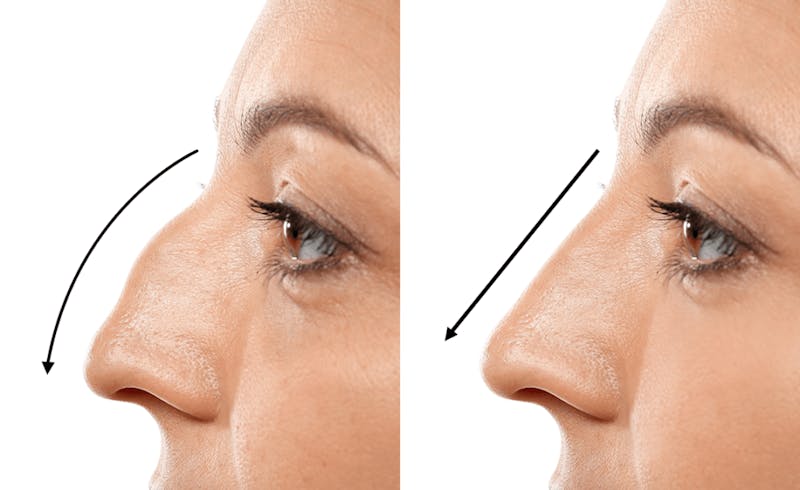
Photographic documentation: standardized photos (frontal, lateral, oblique, base view) for planning and comparison
-
CT Scan or X-rays: rarely, for complex trauma or sinus issues
-
3D Imaging/Simulation: computer-assisted planning may help visualize possible outcomes
-
-
Functional Testing
-
Nasal endoscopy: for internal blockages or anatomical issues
-
Breathing tests: rhinomanometry or acoustic rhinometry if functional issues suspected
-
-
Laboratory Testing
-
Basic blood work, coagulation profile, and screening as required by anesthesia protocol
-
-
Psychological Assessment
-
Screen for body dysmorphic disorder, unrealistic expectations, or psychological contraindications
-
Preoperative Consultation
-
Discuss goals, risks, benefits, alternatives, and limitations
-
Set realistic expectations (no “perfect” nose—aim for natural harmony)
-
Provide detailed pre-op and post-op instructions
Treatment Options of Rhinoplasty
Rhinoplasty (commonly called a “nose job”) is a surgical procedure designed to reshape, reconstruct, or improve the function of the nose. Treatment options vary depending on whether the goal is medical (functional improvement), cosmetic (aesthetic refinement), or both. The approach also depends on patient anatomy, health status, and desired outcomes.
Types of Rhinoplasty
-
Open Rhinoplasty
-
Involves a small incision across the columella (the tissue between the nostrils), allowing the skin to be lifted and the surgeon to directly visualize the nasal structures.
-
Provides precision, especially for complex reshaping, but leaves a tiny, usually unnoticeable scar.
-
-
Closed (Endonasal) Rhinoplasty
-
All incisions are made inside the nostrils; no external scar.
-
Preferred for less extensive corrections, quicker healing, less swelling.
-
-
Secondary / Revision Rhinoplasty
-
For patients with prior nasal surgery seeking correction or improvement.
-
More complex due to scar tissue, altered anatomy.
-
-
Functional / Septorhinoplasty
-
Combines aesthetic reshaping with correction of internal blockages (septal deviation, turbinate hypertrophy).
-
-
Non-Surgical Rhinoplasty
-
Temporary corrections using injectable fillers (hyaluronic acid) to smooth out minor bumps or asymmetries.
-
Not suitable for major changes; not permanent.
-
The Surgical Procedure
-
Anesthesia: Usually general anesthesia; local anesthesia with sedation in select cases
-
Incision and Reshaping: Bone and cartilage are reshaped, removed, or augmented; septum straightened if needed
-
Closure and Splinting: Incisions closed, nasal splint applied to maintain shape and protect
-
Duration: Typically 1–3 hours, outpatient basis
Recovery
-
Swelling and bruising are common and peak in 2–3 days, gradually resolving over 2–4 weeks
-
Most patients return to work/school in 7–10 days, but full results may take 6–12 months to appear
Prevention and Management of Rhinoplasty Complications
Rhinoplasty, while highly effective in reshaping the nose for cosmetic or functional purposes, carries risks like any surgical procedure. Complications may include infection, bleeding, breathing difficulties, scarring, dissatisfaction with results, or anesthesia-related risks. Preventing and managing these complications requires careful planning, surgical precision, and attentive post-operative care.
Prevention Strategies
-
Careful preoperative assessment and surgical planning
-
Choose a qualified, experienced facial plastic or ENT surgeon
-
Strict adherence to pre-op instructions (smoking cessation, medication management)
-
Optimize underlying health conditions before surgery
Postoperative Management
-
Keep the head elevated to minimize swelling
-
Cold compresses for the first 48 hours
-
Take prescribed antibiotics, painkillers, and anti-inflammatory medications as advised
-
Avoid strenuous activity, nose blowing, or heavy lifting for several weeks
-
Protect nose from trauma and sun exposure
-
Attend all follow-up appointments for monitoring
Patient Education
-
Provide realistic expectations for swelling, bruising, and timeline for final results
-
Warn about normal healing phases (numbness, mild asymmetry, temporary breathing difficulty)
Complications of Rhinoplasty
Rhinoplasty is one of the most commonly performed cosmetic and reconstructive surgeries worldwide. While it can significantly improve facial aesthetics, breathing, and self-confidence, it also carries potential risks and complications, like any surgical procedure. These complications may be short-term, long-term, functional, or aesthetic.
Common Risks
-
Bleeding (Epistaxis): Usually minor, rarely severe
-
Infection: Rare, prevented with antibiotics and sterile technique
-
Swelling and Bruising: Temporary, resolves over weeks
-
Pain and Discomfort: Manageable with medications
Specific Complications
-
Unsatisfactory Aesthetic Outcome: Residual asymmetry, persistent hump, tip issues, or visible scars
-
Breathing Difficulties: Internal scarring, collapse of nasal valves, septal perforation
-
Nasal Obstruction or Whistling: Due to septal perforation or poor healing
-
Numbness: Especially at the tip, usually temporary
-
Septal Hematoma or Abscess: Rare, but serious if not managed
-
Skin Discoloration or Thickening: Especially in patients with darker or thicker skin
-
Keloid or Hypertrophic Scarring: Rare, but more common in predisposed individuals
-
Need for Revision Surgery: Occurs in 5–15% of cases
How to Minimize Risks
-
Select a highly skilled surgeon
-
Follow all pre- and post-op instructions
-
Attend regular follow-ups for early detection and management of complications
Living with the Condition of Rhinoplasty
Undergoing rhinoplasty (nose surgery) can be both a physical and emotional journey. While the procedure aims to enhance appearance or correct medical issues such as breathing difficulties, living with the results requires adjustment, patience, and lifestyle adaptation.
Recovery and Adjustment
-
First week: Expect swelling, bruising, congestion, and mild discomfort. Most people can return to light activities after 1 week.
-
First month: Swelling reduces; shape and breathing improve. Avoid contact sports or activities that risk injury.
-
Long-term: Minor swelling may persist for several months, especially at the tip. Final results become visible by 6–12 months.
Psychological and Emotional Adjustment
-
It’s normal to experience a range of emotions (relief, anxiety, impatience) as you adjust to your new appearance.
-
Support from friends, family, or support groups can help during recovery.
-
For some, counseling or patient forums may be beneficial, especially if adjusting to a changed facial feature.
Lifestyle Modifications
-
Avoid sun exposure to protect healing skin and minimize pigmentation
-
Maintain a healthy diet, stay hydrated, and avoid smoking to aid recovery
-
Use gentle facial cleansers and moisturizers; avoid glasses on the nose for 3–4 weeks if possible
Follow-up Care
-
Attend all scheduled check-ups for suture removal, progress monitoring, and to address any concerns early
Top 10 Frequently Asked Questions about Rhinoplasty
1. What is rhinoplasty and why is it performed?
Rhinoplasty is a surgical procedure that reshapes or resizes the nose for cosmetic or functional reasons. Patients may seek rhinoplasty to enhance facial harmony, correct a prominent bump or crooked nose, refine the tip, change nostril size, or fix injuries. Functionally, rhinoplasty may also correct breathing difficulties caused by structural problems, such as a deviated septum or birth defect.
There are two main approaches:
-
Cosmetic Rhinoplasty: Improves appearance and confidence.
-
Functional Rhinoplasty: Restores or improves breathing.
Rhinoplasty can be performed on both men and women, and is one of the most commonly requested plastic surgeries worldwide.
2. Who is a good candidate for rhinoplasty?
Ideal candidates for rhinoplasty are:
-
Physically healthy, with no serious medical conditions that could affect healing.
-
Nonsmokers, or willing to quit before and after surgery, since smoking delays healing.
-
Individuals whose facial growth is complete (usually age 16–18+).
-
People who have a realistic expectation about what the surgery can achieve.
-
Those bothered by the shape, size, symmetry, or function of their nose.
-
Patients with injuries or congenital defects impacting nasal appearance or breathing.
Before surgery, a thorough medical evaluation and discussion of goals with a board-certified surgeon are essential.
3. What issues can rhinoplasty address?
Rhinoplasty is a highly customizable surgery and can address:
-
Humps or depressions on the bridge of the nose.
-
A nose that is too large, small, wide, or narrow.
-
A crooked or deviated nose (from injury or genetics).
-
A bulbous, drooping, or upturned tip.
-
Asymmetric or overly large nostrils.
-
Breathing problems due to internal blockages or a deviated septum.
-
Previous injuries, birth defects, or unsatisfactory results from prior surgeries (revision rhinoplasty).
4. How is rhinoplasty performed? What techniques are used?
Rhinoplasty can be performed using two primary approaches:
1. Open Rhinoplasty:
-
A small incision is made across the columella (the skin between the nostrils).
-
Allows the surgeon to lift the nasal skin and have a clear view of the underlying structures.
-
Preferred for complex cases, revisions, or major reshaping.
2. Closed (Endonasal) Rhinoplasty:
-
All incisions are made inside the nostrils, leaving no external scars.
-
Suitable for less complex reshaping.
During the procedure, the surgeon may:
-
Remove, reshape, or graft cartilage and bone.
-
Refine the nasal tip.
-
Straighten the septum for better airflow.
-
Alter nostril shape or size.
The surgery typically lasts 1–3 hours and is done under general or local anesthesia with sedation.
5. What is recovery like after rhinoplasty?
Recovery after rhinoplasty is a gradual process:
-
First week: Expect swelling, bruising (especially under the eyes), mild pain or stuffiness, and a splint on the nose. Most swelling and bruising peak at 2–3 days, improving over the first week.
-
Splint and stitches: Usually removed after 7–10 days.
-
Returning to normal activities: Most patients can resume work or school in 1–2 weeks, but should avoid strenuous exercise for 3–4 weeks.
-
Swelling: Subtle swelling (especially at the tip) can last several months. The final result is often seen after 6–12 months.
-
Tips for smoother recovery: Sleep with your head elevated, avoid blowing your nose, protect the nose from injury, and follow all surgeon instructions.
6. What are the risks or complications of rhinoplasty?
While rhinoplasty is generally safe with an experienced surgeon, it carries certain risks:
-
Infection, bleeding, or poor wound healing.
-
Adverse reactions to anesthesia.
-
Scarring (external scar in open technique, usually minimal and fades).
-
Persistent swelling or bruising.
-
Numbness around the nose.
-
Difficulty breathing through the nose.
-
Asymmetry or dissatisfaction with the cosmetic result.
-
Rarely, septal perforation (hole in the septum) or the need for revision surgery.
Careful surgical planning and following post-operative care instructions minimize these risks.
7. How long do rhinoplasty results last?
Rhinoplasty results are typically permanent.
The reshaped nasal bone and cartilage retain their new form for life. Natural aging
can lead to some changes over decades, but the improved shape and function remain.
It’s important to note:
-
Revision surgery is rare but possible if healing doesn’t go as planned.
-
Protect your nose from injury after surgery, especially during the first year.
8. Will insurance cover rhinoplasty?
-
Functional rhinoplasty (to correct breathing issues, injury, or congenital defects) may be covered by insurance, either in full or partially.
-
Cosmetic rhinoplasty (for appearance only) is usually not covered.
-
If both cosmetic and functional issues are addressed, only the functional portion may be eligible for coverage.
-
Always check with your surgeon and insurance provider for details and required documentation.
9. How do I choose the right surgeon for rhinoplasty?
Choosing a skilled, board-certified plastic or facial surgeon is crucial for a successful outcome. Look for:
-
Board certification in plastic surgery, otolaryngology, or facial plastic surgery.
-
Experience with rhinoplasty (ask to see before-and-after photos).
-
Good patient reviews and hospital affiliations.
-
Willingness to discuss your goals, show you 3D simulations, and explain risks honestly.
A detailed consultation and mutual understanding of expectations help ensure a satisfying result.
10. What are alternatives to surgical rhinoplasty?
Non-surgical rhinoplasty (liquid rhinoplasty) uses injectable fillers (like hyaluronic acid) to temporarily smooth out bumps or correct minor asymmetry.
-
Benefits: Minimally invasive, quick, and no downtime.
-
Limitations: Results last 6–18 months; cannot reduce nose size, fix breathing issues, or provide major structural change.
-
Risks: Bruising, swelling, or rare vascular complications.
Surgical rhinoplasty remains the only way to achieve lasting, dramatic changes.


