Introduction to Vitrectomy & Retinal Detachment
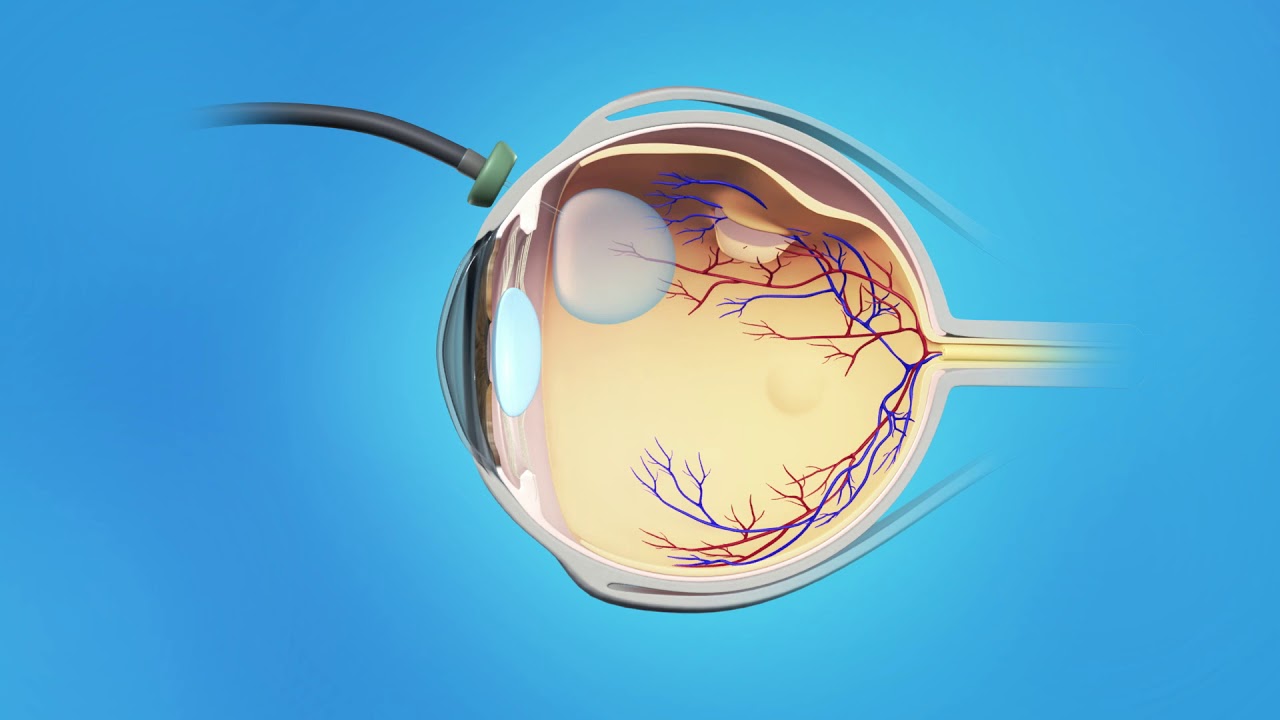
Vitrectomy and retinal detachment are two closely linked subjects in the field of ophthalmology. Vitrectomy is a highly specialized surgical technique, often used as the last line of defense against severe eye diseases, especially those involving the retina-the delicate, light-sensitive layer at the back of the eye responsible for vision.
Retinal detachment is a critical medical emergency. It occurs when the retina peels away from its underlying tissue, much like wallpaper coming off a wall. This loss of connection deprives the retina of oxygen and nutrients, leading to permanent vision loss if not treated quickly. Many causes of retinal detachment require prompt surgical repair, and vitrectomy is one of the most important procedures in this context.
Over the past few decades, advances in vitrectomy technology, microsurgical instruments, and retinal imaging have dramatically improved outcomes for patients with retinal diseases. Today, people who would have been rendered blind in previous generations can regain much of their vision thanks to these life-changing interventions.
Causes and Risk of Retinal Detachment / Vitrectomy Indications
Retinal detachment is a serious eye condition in which the retina-the light-sensitive tissue at the back of the eye-pulls away from its normal position. If untreated, it can lead to permanent vision loss. A vitrectomy is one of the main surgical procedures used to repair retinal detachment, as well as other vitreoretinal diseases. Understanding the causes, risks, and surgical indications is essential for both prevention and timely intervention.
Causes & Risk Factors of Retinal Detachment
Key reasons and risk enhancers include:
-
Posterior Vitreous Detachment (PVD): As we age, the vitreous shrinks and liquefies; it can pull away from the retina, sometimes causing tears. This is a leading cause of rhegmatogenous detachment.
-
High Myopia (Nearsightedness): Longer eyeball shape stresses retinal tissue, increasing risk of tears/detachment.
-
Previous Eye Surgery: Cataract removal or lens replacement can predispose to vitreous shifts and retinal breaks.
-
Trauma or Injury: Blunt or penetrating eye injury can directly cause retinal tears or detach the retina.
-
Lattice Degeneration / Thin Retina Areas: Areas of weak retina are more prone to forming holes or tears.
-
Family History / Previous Detachment: If one eye had detachment, risk increases in the other.
-
Retinal Diseases / Vascular Conditions: Conditions like diabetic retinopathy, proliferative vitreoretinopathy (PVR), or retina scarring can produce traction forces.
Indications for Vitrectomy (When It Is Used)
Vitrectomy is indicated when:
-
Retinal detachment is complex (multiple tears, large detachments, or involvement of macula).
-
Tractional forces are involved (scar tissue pulling on retina).
-
Vitreous hemorrhage (bleeding into the vitreous) obscures view or prevents proper treatment.
-
Conventional methods (scleral buckle, pneumatic retinopexy) are unsuitable or insufficient.
-
Combined pathologies: retinal tears, macular holes, epiretinal membranes, etc.
-
Recurrent detachments after prior surgery.
Thus, vitrectomy is often reserved for challenging cases or when direct internal manipulation of the retina is needed.
Symptoms and Signs of Retinal Detachment / Pre-Vitrectomy Presentation
Retinal detachment is a vision-threatening condition that requires immediate recognition and treatment. In most cases, the first warning signs are subtle, but they can progress rapidly to significant vision loss if untreated. Understanding the symptoms and clinical signs helps patients seek prompt care and allows ophthalmologists to plan timely surgical interventions such as vitrectomy.
Symptoms of Retinal Detachment
Patients often notice:
-
Sudden appearance of floaters: small dots, lines, or webs drifting in the visual field.
-
Flashes of light (photopsias): usually in the peripheral vision.
-
A dark “curtain” or shadow moving across vision (from periphery toward center).
-
Sudden blurring or decreased vision in part of the visual field.
-
Distorted vision (metamorphopsia).
-
Loss of peripheral vision first, possibly progressing to central if not treated.
These are typically painless; retinal detachment does not cause discomfort in most cases.
Signs Seen on Ophthalmic Examination
During eye examination (dilated fundus exam, imaging), doctors may find:
-
Elevation and wrinkling of the retina.
-
Retinal breaks or holes (flaps or tears).
-
Subretinal fluid beneath detached portions.
-
Tractional membranes or scar tissue pulling on retina.
-
Associated vitreous opacities, hemorrhages, or pigmentation changes.
If vitrectomy is being considered, signs of vitreous traction, hemorrhage, or obscured view may guide the decision.
Diagnosis of Retinal Detachment & Pre-Surgical Evaluation
Retinal detachment is a sight-threatening emergency where the retina separates from the underlying retinal pigment epithelium (RPE). Without timely intervention, it can lead to permanent vision loss. Diagnosis requires careful clinical assessment and imaging, while pre-surgical evaluation ensures the best treatment approach is chosen and complications are minimized.
Clinical Diagnosis
-
Dilated Fundus Examination: Using indirect ophthalmoscope, slit-lamp with special lenses. Ophthalmologist inspects periphery for tears, detachment.
-
Scleral Depression: To view retinal periphery thoroughly.
-
Fundus Photography / Wide-field Imaging: To document the detachment.
-
Ultrasound (B-scan): Especially when media (e.g. vitreous hemorrhage) obstructs a view of the retina. Useful to detect retinal detachment behind opaque media.
-
Optical Coherence Tomography (OCT): For macular involvement, details of retina thickness, and associated changes.
Preoperative Assessment
-
Visual acuity, intraocular pressure, pupil reflexes.
-
Lens status: Is there a cataract, or is the patient pseudophakic (has artificial lens)?
-
Ocular health: Cornea, anterior chamber, any inflammation, glaucoma history.
-
Medical fitness: Systemic evaluation (blood tests, general health) to ensure patient can tolerate surgery and anesthesia.
-
Patient counseling: Understand risks, benefits, postoperative positioning, potential outcomes.
The preoperative work guides surgical planning (e.g. choice of gas vs oil tamponade, extent of vitrectomy).
Treatment Options for Retinal Detachment / Vitrectomy Procedure
Retinal detachment is a serious eye condition that requires prompt treatment to prevent permanent vision loss. The primary goal of treatment is to reattach the retina and restore as much vision as possible. The choice of treatment depends on the type, location, and severity of the detachment, as well as the overall health of the eye.
Overview of Treatment Strategies
Retinal detachments are typically treated with surgery, and the choice depends on the type, extent, location, and other eye conditions. The main surgical options include:
-
Pneumatic Retinopexy: Injection of gas bubble into vitreous cavity, with laser/cryotherapy to seal the retinal tear. Often used for small detachments in the upper retina.
-
Scleral Buckle: A silicone band is sewn around the outside of the eye (sclera), indenting the eye wall toward the retina to close the tear and support reattachment.
-
Vitrectomy (often combined with laser/cryotherapy and tamponade): The vitreous is removed so the surgeon can directly access the retina, flatten it, seal tears, and insert internal tamponade (gas or oil).
In many cases, combination therapy is used (e.g., vitrectomy + scleral buckle) depending on complexity.
The Vitrectomy Procedure - Step by Step
Here is a typical sequence for a pars plana vitrectomy (the standard posterior vitrectomy approach):
-
Anesthesia & Preparation: Local (regional) anesthesia with sedation or general anesthesia depending on case.
-
Incisions (Trocars): Small (23G, 25G, or 27G) cannulas are placed in the pars plana region (a region just behind the iris/sclera junction) for instrument access.
-
Core Vitrectomy: Removal of central vitreous gel.
-
Induction of Posterior Vitreous Detachment (if not already present): To reduce traction on retina.
-
Peripheral Vitrectomy & Traction Release: Clear vitreous skirt and relieve vitreoretinal tractions, remove membranes if present.
-
Drain Subretinal Fluid (if needed): Make a small retinotomy (opening in retina) to drain fluid under detached retina.
-
Seal Retinal Tears: Use laser photocoagulation or cryotherapy around the edges of tears or breaks to create a scar that bonds the retina to the underlying retinal pigment epithelium.
-
Tamponade Insertion: A bubble of gas (e.g. SF6, C3F8) or silicone oil is inserted into the vitreous cavity to press the retina against the eye wall while healing occurs.
-
Closing the Incisions: Some incisions seal themselves; others may require sutures.
-
Postoperative Positioning: The patient may need to maintain a specific head posture to keep the gas/oil bubble pressing on the correct area of retina.
The length of surgery can range from ~30 minutes to several hours, depending on complexity.
Postoperative Care & Recovery
-
Eye patching / protective shield initially.
-
Use of eye drops: Antibiotics, steroids, anti-inflammatories to prevent infection, control inflammation, manage intraocular pressure.
-
Head positioning: Especially when gas bubble is used, to press the retina in the correct place.
-
Activity restrictions: Avoid heavy lifting, strenuous exercise, sudden head movements, and flying (if gas bubble present).
-
Follow-up visits: Frequent checks to monitor retinal reattachment, intraocular pressure, corneal clarity, cataract formation.
-
If silicone oil used, a second surgery may be required to remove the oil later.
Timing & Prognosis
-
Urgency matters: The sooner surgery is done after detachment (especially before the macula is involved), the better the visual prognosis.
-
Macula status: If macula (central retina) is still attached, outcomes are better; once it's detached, full recovery is less certain.
-
Extent, duration, and complexity of detachment, presence of PVR, scarring, and the general eye health influence success rates.
Prevention and Management of Retinal Detachment / Vitrectomy Aftercare
Retinal detachment is a condition where prevention plays a limited role since many risk factors are beyond control. However, early detection, lifestyle management, and adherence to aftercare following procedures like vitrectomy can significantly reduce the risk of recurrence and protect long-term vision.
Prevention & Early Detection
-
Routine eye exams, especially in high-risk individuals (high myopia, previous retinal tear, family history).
-
Identify and treat retinal breaks or tears early (with laser or cryotherapy) before they detach.
-
Protect eyes from trauma (sports, accidents).
-
Educate patients to promptly report symptoms like flashes, floaters, or dark “curtain” shadows.
-
Manage underlying conditions (diabetes, hypertension) to reduce vascular stress on the retina.
Postoperative Management for Best Outcomes
-
Strict adherence to postoperative positioning and care as directed by surgeon.
-
Use all prescribed medications (eye drops, anti-inflammatories, antibiotic) without missing doses.
-
Attend all follow-up visits for early detection of complications (e.g. recurrent detachment, elevated pressure).
-
Monitor and manage intraocular pressure (IOP).
-
Gradually resume normal activities when approved (walking, light work), but avoid strenuous exertion.
-
If silicone oil was used, plan the oil removal surgery as advised.
-
Maintain general eye health: avoid smoking, control systemic health (diabetes, blood pressure), good nutrition.
Complications of Vitrectomy & Retinal Detachment Surgery
Though modern vitreoretinal surgery is highly refined, there are risks and complications to be aware of:
-
Recurrent retinal detachment: Despite surgery, detachment may recur.
-
Proliferative vitreoretinopathy (PVR): Scarring and membrane formation that pulls retina out again.
-
Cataract formation: Common, especially if lens is intact; many patients develop or accelerate cataract post-vitrectomy.
-
Elevated intraocular pressure / glaucoma.
-
Bleeding / intraocular hemorrhage.
-
Endophthalmitis (infection inside the eye).
-
Corneal edema / damage.
-
Macular edema or distortion.
-
Gas- or tamponade-related issues: Gas bubble may affect vision temporarily, require strict head positioning, restrict air travel, and may cause pressure changes. Silicone oil may require removal later and itself can cause complications.
-
Ptosis, double vision, hemorrhage at incision sites, or wound leak.
Proper surgical technique, experienced surgeons, and vigilant postoperative monitoring help minimize these risks.
Living with Vitrectomy & Retinal Detachment - Patient Perspective
Recovering from retinal detachment and adapting to life after vitrectomy can be both physically and emotionally challenging. While the surgical procedure often restores the retina and preserves vision, the journey doesn’t end once the operation is over. Patients must adjust to lifestyle changes, monitor their eye health closely, and learn how to cope with new visual realities.
What to Expect Immediately After Surgery
-
Blurred vision initially; possibly worse than before surgery due to swelling, media clarity, or gas bubble.
-
Some discomfort, redness, tearing; use of medicated drops.
-
The gas bubble may impose vision restrictions (you may see shadows, blurred areas).
-
You may be asked to maintain specific head posture (face-down or other orientation) for days/weeks.
-
Some delay in returning to work, driving, or regular activities.
Medium-Term Recovery (Weeks to Months)
-
Gradual clearing of media, absorption of gas bubble (if used), or adjustment to new intraocular environment.
-
Improvement in vision, though may not fully return to previous levels depending on pre-op damage and duration of detachment.
-
Monitoring for onset or progression of cataract.
-
Regular visits to retina specialist to ensure retina remains attached and eye health is maintained.
Long-Term Outlook & Adaptation
-
Many patients regain functional vision, though perfect vision is not guaranteed.
-
In some, contrast, night vision, or subtle distortions may persist.
-
If silicone oil used, its eventual removal may further improve vision.
-
Lifelong vigilance: patients must watch for symptoms in the other eye as well.
-
Protect eyes, maintain ocular and systemic health (control systemic disease).
-
Use of low-vision aids or rehabilitation if needed in residual vision impairment.
Psychological & Lifestyle Aspects
-
Anxiety about vision recovery is normal-clear, realistic counseling helps.
-
Support from family and caregivers during the initial recovery period is beneficial.
-
Patience is crucial: visual recovery may take months.
-
Avoid stressing or rushing the eye-follow restrictions, protect the eye, and adhere to postoperative guidelines.
Top 10 Frequently Asked Questions about Vitrectomy Retinal Detachment
1. What is vitrectomy and how is it related to treating retinal detachment?
A vitrectomy is a surgical procedure in which the vitreous gel filling the eye is
partially or completely removed to allow better access to the the retina.
In cases of retinal detachment, vitrectomy allows the surgeon to remove tractional
membranes, drain subretinal fluid, seal retinal tears (with laser or cryotherapy), and
replace the removed vitreous with a gas bubble or silicone oil to help reattach the
retina.
2. What causes retinal detachment and what are common warning signs?
Causes / Risk factors:
-
A tear or break in the retina (rhegmatogenous type) allowing fluid to pass behind the retina and lift it.
-
Tractional detachment from scar tissue pulling on the retina (e.g., diabetic retinopathy)
-
Exudative detachment due to fluid leakage under the retina (without a tear) from inflammation, tumors, etc.
-
Risk factors include high myopia (nearsightedness), prior eye surgery (e.g. cataract surgery), trauma, family history, and weak or thinning retinal areas.
Warning signs / symptoms:
-
Sudden appearance of floaters (spots, threads) in the field of vision
-
Flashes of light (photopsia)
-
A “curtain” or shadow gradually advancing over part of the visual field
-
Sudden blurred vision or loss of peripheral vision.
If someone experiences these symptoms, prompt evaluation by an eye specialist is essential to reduce the risk of permanent vision loss.
3. Who is a candidate for vitrectomy in retinal detachment?
Vitrectomy is often recommended when:
-
The retinal detachment involves complex tears or is not amenable to simpler procedures (e.g. pneumatic retinopexy).
-
There is traction on the retina from membranes or scar tissue.
-
There is significant vitreous hemorrhage obscuring view of retina.
-
Previous repair attempts have failed or there is recurrent detachment.
-
The detachment includes involvement of the macula (central retina) or is large.
However, the decision is individualized and depends on factors like how long the retina has been detached, the part of retina involved, patient age, presence of other ocular diseases, and surgical risk.
4. What does the vitrectomy procedure involve?
The general steps in a vitrectomy procedure are:
-
The eye is prepared under sterile conditions.
-
Small incisions (micro-incisions) are made through the sclera (white of the eye). Many modern vitrectomies are minimally invasive and sutureless.
-
The vitreous gel is cut and suctioned out (called “vitreous shaving”).
-
The surgeon examines the peripheral retina (often using scleral depression) to identify all retinal breaks or tears and treat them (with laser photocoagulation or cryotherapy).
-
Subretinal fluid is drained (if present) and the retina is reattached.
-
A tamponade agent (gas bubble, air, or silicone oil) is placed inside the eye to press the retina in place while healing occurs.
-
The incisions are checked for leaks (may or may not require sutures) and the eye is patched or shielded.
Typical surgical time may vary, often ranging from 45 minutes to 2 hours depending on complexity.
5. What is the recovery period like and what should patients expect after surgery?
-
Many patients go home the same day of surgery (outpatient basis) if there are no complications.
-
Immediately after surgery, the eye may be red, swollen, and uncomfortable for several days to weeks. Vision initially may be blurrier than before surgery.
-
Eye drops (antibiotics, anti-inflammatory) are prescribed to prevent infection and reduce inflammation.
-
Activities such as heavy lifting, strenuous exercise, bending over, or swimming are generally restricted for several weeks (as per surgeon's instructions).
-
If a gas bubble was used, the patient may need to maintain certain head positioning (e.g. face down or sideways) for a period (a few days to weeks) to keep the bubble in the correct place for tamponade effect.
-
Patients should avoid air travel or rapid altitude changes while the gas bubble remains in the eye.
-
If silicone oil is used, a second surgery may later be needed to remove it once the retina is stable.
-
Visual recovery can be gradual over weeks to months - full improvement may take time, depending on how long the retina was detached and whether the macula was affected.
6. What are the risks or complications associated with vitrectomy for retinal detachment?
While vitrectomy is generally considered safe in expert hands, like all surgeries it carries some risks:
-
Infection (endophthalmitis)
-
Bleeding (intraocular hemorrhage)
-
Elevated or decreased intraocular pressure (glaucoma or hypotony)
-
Cataract formation or acceleration of an existing cataract, especially in older patients
-
Retinal re-detachment or development of new retinal tears / breaks
-
Failure to fully restore vision (especially if the macula was detached or long durations of detachment)
-
In cases where silicone oil is used, potential complications related to the oil (e.g. emulsification)
Because of these risks, careful preoperative evaluation and postoperative follow-up are essential.
7. How soon should vitrectomy or retinal detachment repair be performed?
Timeliness is critical. A retinal detachment is a surgical emergency: the sooner the repair is done, the better chances of preserving vision.
If the macula is still attached (“macula-on” detachment), urgent surgery is preferred to prevent it from detaching.
Delays in repair, especially when the macula is detached (“macula-off”), reduce the likelihood of full visual recovery.
8. Will I need additional surgeries after the initial vitrectomy?
Yes, in some cases additional intervention may be necessary:
-
If silicone oil was used, it often needs removal later via a second surgery, once retina stability is certain.
-
If the retina re-detaches or a new tear forms, additional surgeries may be needed.
-
In some cases, vitrectomy may be combined with scleral buckling or other techniques to improve retinal support, either at the primary surgery or later.
-
Cataract surgery may eventually be needed, especially if a cataract accelerates after vitrectomy.
9. What factors influence the outcome and how good is the success rate?
Factors affecting outcomes:
-
How long the retina has been detached (longer durations worsen prognosis)
-
Whether the macula (central retina) was detached or still attached at the time of surgery
-
Extent, location, and complexity of retinal tears or detachments
-
Presence of proliferative vitreoretinopathy (PVR) or scar tissue formation
-
Patient's age, overall eye health, and coexisting ocular conditions (e.g. glaucoma, diabetic retinopathy)
Success rates:
Many sources report a high anatomical reattachment success rate for vitrectomy in
retinal detachment, often around ~90% in favorable cases.
However, visual improvement may not always reach pre-detachment levels, especially if
there was long-standing detachment or macular involvement.
10. What precautions should patients take before and after vitrectomy?
Before surgery:
-
The surgeon will advise on medications, fasting, and any systemic health checks (e.g. blood pressure, diabetes control).
-
Avoid medications or supplements (anticoagulants, etc.) as instructed by surgeon.
-
Arrange for someone to accompany and drive the patient home after surgery.
After surgery:
-
Strict adherence to postoperative eye drop regimen (antibiotic, anti-inflammatory)
-
Observe head positioning requirements (especially if gas bubble used)
-
Avoid activities that increase eye pressure (heavy lifting, bending, strenuous exercise)
-
Avoid air travel or high altitudes while gas remains in the eye
-
Attend all scheduled follow-up visits to monitor healing, intraocular pressure, and retinal status
-
Report any sudden increase in pain, worsening vision, new flashes or floaters immediately (could indicate complication)


