Introduction to Wireless Capsule Endoscopy
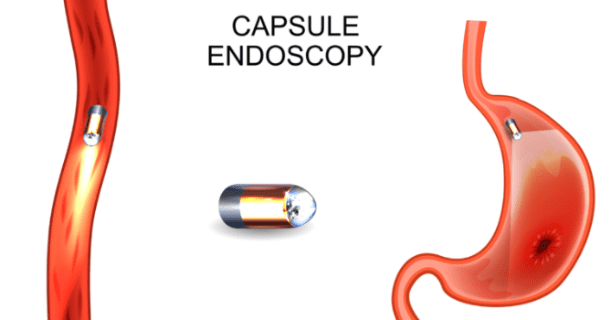
Wireless Capsule Endoscopy (WCE) is an innovative medical technology used to examine the gastrointestinal (GI) tract, particularly the small intestine, which is often difficult to visualize using traditional endoscopic methods like colonoscopies or upper GI endoscopy. This non-invasive procedure involves swallowing a small, pill-sized capsule equipped with a tiny camera. As the capsule moves through the digestive tract, it wirelessly transmits high-resolution images to an external data recorder worn by the patient.
The beauty of capsule endoscopy lies in its ability to provide real-time, high-quality images of the small intestine, helping to diagnose a range of gastrointestinal issues, including inflammatory bowel diseases (IBD), small intestine tumors, bleeding disorders, and celiac disease. Unlike traditional endoscopy, there are no incisions or anesthesia required, making it a less invasive alternative for patients.
The procedure represents a major breakthrough in gastroenterology, offering insights into parts of the digestive system that were previously hard to reach. This guide explores the uses, benefits, risks, and applications of Wireless Capsule Endoscopy, as well as what patients can expect during the procedure.
Causes and Risk Factors Relevant to Wireless Capsule Endoscopy
Because WCE is a diagnostic procedure, strictly speaking it does not have “causes” in the way a disease does. Rather, what one would discuss here is indications, risk factors for failing the test (e.g. retention), and patient populations for which it is useful or contraindicated. Below is how you might structure this:
Indications / Why a physician orders WCE
Some of the main settings in which WCE is used include:
-
Obscure (occult) gastrointestinal bleeding (i.e. persistent iron deficiency anemia or positive fecal occult blood without source found on upper endoscopy / colonoscopy)
-
Suspected small-bowel Crohn's disease or monitoring known Crohn's disease when other studies are inconclusive
-
Evaluation of small-bowel tumors, polyps, or masses
-
NSAID-induced enteropathy (small-bowel ulcers, erosions)
-
Celiac disease complications or refractory celiac disease when conventional biopsy is nonconclusive
-
Incomplete colonoscopy (in some cases) or other GI tract evaluation in patients unfit for conventional scopes
Some guidelines (or medical policy statements) limit its use to certain indications (for example, some insurers consider its use for Crohn's or colonic evaluation “investigational”).
Risk Factors / Contraindications / Limitations
While generally safe, there are risks and limitations. It is important to mention:
-
Capsule retention (i.e. the capsule failing to pass through the GI tract) is the most feared complication. Defined typically as the capsule remaining in the GI tract for ≥ 2 weeks or requiring intervention.
-
Risk is higher in patients with known Crohn's disease, strictures, prior abdominal surgeries, radiation enteritis, or adhesive disease.
-
In a review of >22,000 procedures, retention occurred in ~1.4% of cases overall, but higher in Crohn's patients (~5-13%) and lower in bleeding evaluation cases.
-
Some retained capsules may fragment, cause obstruction, or very rarely perforation.
-
Retrieval may require endoscopic or surgical intervention.
-
-
Incomplete examination: because of limited battery life or rapid transit in parts of the GI tract, parts of the small bowel may not be visualized. Some studies report ~10-20% of exams as incomplete.
-
Poor image quality due to residual food, debris, bubbles, or rapid movement.
-
Inability to control capsule: no steering, no insufflation, no suction, no biopsy — limiting ability to sample an abnormal lesion or revisit a suspicious site.
-
Technical limitations: battery duration, frame rate, signal loss, misalignment of sensors, interference.
-
Relative contraindications: known GI obstruction, swallowing disorders, patients with pacemakers or other electronic implants (though many newer systems are safe), pregnancy (usually avoided), GI fistulas or strictures, or inability to cooperate with preparation.
It is helpful in your content to distinguish the “risks of using capsule endoscopy” (i.e. retention, incomplete study) from disease risks — readers sometimes confuse “treatment risks” as disease causes.
Symptoms and Signs (What WCE Detects / Clinical Presentation)
Because WCE is a diagnostic tool, “symptoms and signs” refers to the underlying GI conditions it helps detect. In your content, you can frame this as:
Clinical contexts / patient presentations in which WCE is useful. Below are common scenarios and findings.
Clinical Presentations Leading to WCE
-
Occult or obscure GI bleeding / iron deficiency anemia — Patient may present with fatigue, pallor, low hemoglobin, positive fecal occult blood test or melena/hematochezia when upper/lower scopes fail to locate source. WCE is often used when both upper GI endoscopy and colonoscopy are negative.
-
Abdominal pain, chronic diarrhea, weight loss — These are nonspecific symptoms raising suspicion of small bowel disease (e.g. Crohn's, small bowel tumors, celiac disease). WCE may help identify mucosal inflammation, ulcers, strictures.
-
Suspected Crohn's disease — In patients with negative ileocolonoscopy or imaging, WCE can detect early mucosal lesions (aphthous ulcers, linear ulcers) especially in jejunum or mid small bowel.
-
Tumors / polyps of small bowel — Patients may present with bleeding, obstruction, malabsorption or nonspecific symptoms, and WCE may detect protruding lesions, mass effect, mucosal irregularities.
-
NSAID enteropathy — Chronic painkillers can cause ulceration or erosions in the small bowel, which may lead to obscure bleeding or abdominal symptoms. WCE can image these mucosal defects.
-
Refractory celiac disease — In patients with ongoing symptoms or suspected complications (ulcerative jejunoileitis, lymphoma), WCE can detect mucosal atrophy, ulceration, or neoplastic changes beyond the reach of standard duodenal biopsy.
Typical Findings / Signs on WCE Imaging
When reviewing the capsule images, a gastroenterologist might see:
-
Mucosal erosions, ulcers, or ulcerated plaques
-
Mucosal erythema/inflammation
-
Vascular lesions / angiodysplasias / telangiectasia
-
Protruding lesions, masses, polyps, submucosal bulges
-
Nodular mucosa, stricturing segments or narrowing
-
Bleeding stigmata such as fresh blood, clots
-
Villous atrophy, mosaic patterns (e.g. in celiac)
You can include sample images or anonymized cases of typical lesions seen via capsule endoscopy (with captions) to enrich the content.
Diagnosis via Wireless Capsule Endoscopy (Procedure, Workflow)
This section should walk the reader through how WCE is done, how images are analyzed, and limitations.
Preparation and Patient Requirements
-
Patients are instructed to fast (usually 8-12 hours) before swallowing the capsule to reduce residue and improve visibility.
-
Bowel preparation (a clear liquid diet, laxatives, possibly a purgative bowel cleansing) may be required (often the night before) to clear debris.
-
Adhesive surface sensors or electrodes may be placed on the abdomen; the receiver is strapped to the waist or worn in a belt.
-
The patient swallows the capsule with water (sometimes with a small shimmy or maneuvers to ease swallowing).
-
During the study, patients are usually allowed to move freely, eat light meals after a few hours (as per protocol), and carry on normal daily activities.
Image Capture, Transmission, and Recording
-
The capsule captures images (often at 2-6 frames per second) and transmits them wirelessly to the external recording device for the duration of battery life (commonly 8-12 hours).
-
The external recorder stores the images and associated timing / localization data. After the capsule exits (typically passed in stool), the recording device is returned to the facility, and data are downloaded.
Interpretation & Reporting
-
A trained gastroenterologist (or GI specialist) reviews the thousands of images, often using software tools that highlight potential abnormalities, bleeding, or suspicious lesions.
-
The report describes location (time index, estimated small bowel segment), lesion findings (ulcers, vascular lesions, strictures, masses) and any suspected bleeding sources.
-
Some scoring systems exist in Crohn's disease for capsule activity (e.g. Lewis score, CE Crohn's Disease Activity Index) to quantify inflammation.
Limitations & Pitfalls (revisited)
-
As noted earlier, incomplete studies due to battery life or rapid transit may leave gaps.
-
False negatives can occur (lesions may be missed because of poor visualization).
-
Uncertain localization — the capsule is passive, so exact anatomical correlates may be imprecise.
-
Artefacts, bubbles, fluid, debris, or overlapping folds may hinder accurate reading.
-
Misalignment or signal loss due to electronics or interference.
Complementary / Follow-up Diagnostics
If WCE findings suggest a lesion needing biopsy or therapy, additional procedures may follow:
-
Conventional endoscopy or push enteroscopy to sample or treat the lesion
-
Deep enteroscopy (double-balloon, single-balloon, spiral) for access to small-bowel lesions
-
Radiologic imaging (CT enterography, MR enterography) to assess extraluminal involvement or mass extension
-
If capsule retention is suspected, plain abdominal X-ray, CT or small bowel follow-through may localize the capsule
Treatment Options of Conditions Diagnosed via Capsule Endoscopy
This section is about the therapeutic follow-up — once WCE reveals a pathology, what treatments are available.
Because WCE is diagnostic only, “treatment options” refer to the underlying conditions discovered. You may organize by condition:
Bleeding / Vascular Lesions (e.g. Angiodysplasia)
-
Endoscopic treatments: argon plasma coagulation, laser, electrocautery via enteroscopy
-
Medical therapy: iron supplementation, blood transfusion if needed, somatostatin analogues
-
Interventional radiology: embolization when endoscopic control fails
-
Surgery in refractory bleeding
Crohn's Disease / Inflammatory Bowel Disease
-
Medical therapy: corticosteroids (for induction), immunomodulators (azathioprine, methotrexate), biologics (anti-TNF, anti-integrin, anti-IL)
-
Nutritional therapy, dietary modulation, symptom control
-
If strictures or obstruction: endoscopic dilation or surgical resection
-
Monitoring and surveillance for complications
Small-Bowel Tumors / Polyps
-
Surgical resection (open or laparoscopic) depending on location, size, and malignancy risk
-
Endoscopic resection if accessible
-
Oncologic management (chemotherapy, radiotherapy, targeted therapy) in malignant tumors
-
Surveillance in polyposis syndromes
NSAID Enteropathy / Ulcerative Lesions
-
Stop or reduce offending NSAID / medication
-
Proton pump inhibitors or localized anti-inflammatory therapy
-
Monitor bleeding and anemia, iron supplementation
-
Follow-up imaging/endoscopy to assess healing
Handling Capsule Retention (if it occurs)
-
Conservative management: if asymptomatic, some physicians observe (especially if spontaneous passage anticipated)
-
Endoscopic retrieval: using double-balloon or deep enteroscopy if reachable
-
Surgical retrieval: via laparoscopy or open surgery in obstructed or complicated cases
You may also include a small “decision tree” or algorithm: e.g. WCE → abnormal lesion → plan: endoscopy, imaging, surgery, medical therapy.
Prevention and Management Strategies (Before, During, After)
Since WCE is a test, this section is more about ensuring a successful, safe procedure and managing patient expectations and risk mitigation.
Pre-procedure Strategies
-
Careful patient selection: screening for known strictures, history of bowel surgery, Crohn's disease, radiation, adhesions
-
Use of patency capsule (a dissolvable capsule) in high-risk patients to assess intestinal patency (i.e. whether capsule can pass) — though its utility is still debated.
-
Adequate bowel preparation (diet, laxatives, purgative) to minimize debris and improve visualization
-
Instruction to patients about preparation, hydration, and what to expect
During the Procedure
-
Advise minimal strenuous activity, although moderate movement is typically allowed
-
Monitoring adherence to protocol (e.g. when to resume food, when to return recorder)
-
Use of sensor placement optimization to minimize signal loss
Post-procedure and Follow-up
-
Confirm passage of the capsule (ask patient to check stool; if not found, may use imaging)
-
Monitor for symptoms of retention (abdominal pain, nausea, vomiting, obstruction signs)
-
Review images, deliver results, plan further steps
-
If retention is suspected or confirmed, follow algorithm for intervention
-
In patients with chronic GI disease (e.g. Crohn's), schedule periodic surveillance or follow-up imaging as per guidelines
Patient Education & Lifestyle
-
Inform patient about signs to watch (abdominal pain, no capsule passage)
-
Diet, hydration, and compliance with follow-up
-
In disease-specific settings (e.g. Crohn's), standard disease-modifying strategies
Complications of Wireless Capsule Endoscopy
Although WCE is considered safe, complications (albeit uncommon) must be addressed. You should present both incidence, risk factors, signs to watch for, and management.
Typical / Known Complications
-
Capsule retention / obstruction
-
Incidence overall ~1-2%, higher in patients with known Crohn's or strictures.
-
May cause partial or complete bowel obstruction, intervention may be needed.
-
Rarely, capsule fragmentation, perforation have been reported in long-term retention.
-
-
Incomplete examination / missed lesions
-
Some segments of the small bowel may not be visualized due to rapid transit or battery exhaustion.
-
-
Technical failures / image artifacts
-
Signal loss, misalignment of sensors, data corruption, electromagnetic interference
-
Blurred images from debris, bubbles, luminal content, or motion
-
-
Aspiration / swallowing difficulty (rare)
-
In patients who have trouble swallowing, the capsule might be mis-swallowed or lodged in the esophagus (rare).
-
-
Other rare risks
-
Allergic reaction to adhesives or sensors
-
Discomfort or local skin irritation from recorder belts or sensors
-
In theory, interference with some implanted electrical devices, though most modern systems are safe
-
Signs / Warning Symptoms
Patients should seek medical care if they experience:
-
Persistent abdominal pain or cramping
-
Nausea, vomiting
-
Bloating, inability to pass gas or stools
-
Fever
-
No passage of capsule in expected time (e.g. beyond several days)
Management Approaches
-
Conservative observation (if asymptomatic and retention is minimal)
-
Imaging (X-ray, CT) to locate capsule
-
Endoscopic retrieval (enteroscopy) if possible
-
Surgical retrieval (laparoscopic or open) if obstruction or complications exist.
-
In rare perforation cases, emergency surgery
You can include statistics from literature reviews or case series to underscore the low risk but serious potential.
Living with the Condition / After the Procedure / Patient Perspective
This section helps patients or readers understand what to expect, how to live around the procedure, recovery, monitoring, and longer-term aspects.
What Patients Should Expect
-
The procedure is painless — the patient should not feel the capsule as it moves through intestines.
-
Typically, after 8-12 hours, the sensors are removed and the patient can resume normal activities (depending on local protocol).
-
The capsule is excreted naturally (usually within 24-48 hours) in stool.
-
Patients may be asked to inspect stools or collect specimen to confirm capsule passage
Follow-up & Monitoring
-
Review of capsule images and clinician consultation to discuss results and next steps
-
If pathology is detected — follow-up investigations or treatment as discussed above
-
In chronic diseases (e.g. Crohn's), additional surveillance and therapeutic monitoring
-
Monitoring for delayed complications (e.g. signs of retention)
Quality of Life & Precautions
-
Because the test is minimally invasive, minimal downtime is expected
-
Patients should stay hydrated, eat lightly as per instructions, and comply with bowel prep for optimal results
-
If the underlying diagnosis is a chronic GI condition (e.g. Crohn's, small bowel disease), patients may need lifelong monitoring, dietary adjustments, medications, and lifestyle modifications
-
In case of capsule retention, patients may require further interventions, which can affect recovery and patient anxiety
Tips for Patients (To Include as a Sidebox or Sidebar)
-
Report any symptoms such as abdominal pain, nausea, inability to pass stool or gas after the procedure
-
Keep the recording device safe and intact, follow instructions about not tampering with sensors
-
Note the timing of any meals (if allowed) as it may help in localization of lesions
-
Keep a diary (time, symptoms) during the study day to correlate with findings
-
Ensure the follow-up appointment is kept to review results
-
Ask your doctor whether you are a candidate for newer “smart capsule” or advanced imaging options
Top 10 Frequently Asked Questions about Wireless Capsule Endoscopy
1. What is wireless capsule endoscopy?
Wireless capsule endoscopy (WCE) is a non-invasive diagnostic procedure used to examine the inside of the gastrointestinal (GI) tract. It involves swallowing a small, pill-sized capsule equipped with a camera. As the capsule moves through the digestive system, it takes thousands of pictures that are transmitted to an external receiver worn by the patient. The images are then analyzed by a doctor to diagnose conditions like Crohn's disease, ulcers, and gastrointestinal bleeding.
2. How does wireless capsule endoscopy work?
The procedure works as follows:
-
Swallowing the capsule: The patient swallows a small, pill-sized capsule that contains a tiny camera and a light source.
-
Capturing images: As the capsule travels through the digestive system, it captures high-quality images of the esophagus, stomach, small intestine, and part of the colon.
-
Transmitting data: The camera transmits the images wirelessly to a small external recorder worn by the patient, typically attached to a belt or around the waist.
-
Data analysis: Once the capsule passes through the digestive system (usually in 8-12 hours), the data is transferred to a computer, where a doctor analyzes the images to look for any abnormalities.
The procedure is painless and does not require sedation.
3. Why is wireless capsule endoscopy used?
Wireless capsule endoscopy is used primarily for diagnosing conditions that affect the small intestine, which is difficult to reach with traditional endoscopy. Common uses include:
-
Diagnosing unexplained gastrointestinal bleeding (e.g., from ulcers, Crohn's disease, or tumors)
-
Identifying causes of chronic diarrhea or abdominal pain
-
Evaluating inflammatory bowel diseases (like Crohn's disease and celiac disease)
-
Detecting small intestine tumors, polyps, or vascular malformations
-
Screening for sources of bleeding that are not visible via other diagnostic methods (e.g., traditional colonoscopy or endoscopy)
It's particularly helpful when other diagnostic tests have been inconclusive.
4. What are the benefits of wireless capsule endoscopy?
The main benefits of wireless capsule endoscopy include:
-
Non-invasive: Unlike traditional endoscopies, this method doesn't require insertion of a tube through the mouth or rectum.
-
Minimal discomfort: The procedure is painless, and no sedation is required.
-
Detailed imaging: It provides high-resolution images of the entire GI tract, especially the small intestine, which is hard to examine with conventional endoscopy.
-
Convenient: The patient can swallow the capsule and go about their daily activities while the capsule transmits images. There is no need for hospitalization or long recovery times.
-
Detection of small or hard-to-reach lesions: Wireless capsule endoscopy can detect subtle abnormalities that may be missed by other methods.
5. Is wireless capsule endoscopy safe?
Yes, wireless capsule endoscopy is generally considered safe. Since it is a non-invasive procedure, the risk of complications is minimal. Some possible risks include:
-
Capsule retention: In rare cases, the capsule may become lodged in the GI tract, typically in patients with a narrowed part of the intestine due to conditions like Crohn's disease. If this happens, additional procedures like a CT scan or endoscopic retrieval may be necessary.
-
Discomfort: Although the procedure is painless, some patients may feel slight discomfort when swallowing the capsule.
-
Failure to pass through the intestines: Very rarely, the capsule may not pass through the entire digestive tract, particularly if there are blockages or strictures.
Before the procedure, a doctor will assess whether wireless capsule endoscopy is appropriate for you, especially if you have any pre-existing gastrointestinal conditions.
6. How long does the wireless capsule endoscopy procedure take?
The entire process of wireless capsule endoscopy usually takes 8 to 12 hours for the capsule to travel through the GI tract and pass out of the body naturally. Most patients can go about their normal daily activities, although they are advised to avoid eating or drinking for a few hours before the test and to wear the recording device throughout the procedure.
Afterward, the capsule is naturally excreted in the stool, and the images are analyzed by the doctor.
7. Do I need to prepare for wireless capsule endoscopy?
Yes, some preparation is required before the procedure:
-
Fasting: You may need to fast for 12 hours before the procedure to ensure that the stomach and intestines are empty.
-
Bowel cleansing: Similar to preparation for a colonoscopy, you may be asked to follow a specific regimen to clear the bowel, especially if the procedure is to assess the small intestine.
-
Medications: Inform your doctor about any medications you are taking, as certain medications may need to be paused or adjusted before the procedure.
-
Clothing: You will be asked to wear loose, comfortable clothing for the procedure, as the external receiver will be attached to your waist.
Follow your doctor's instructions closely for optimal results.
8. Are there any side effects or risks associated with wireless capsule endoscopy?
The procedure is generally safe and well-tolerated, with few side effects. However, there are a few potential risks to consider:
-
Capsule retention: As mentioned, the capsule can sometimes become lodged in the digestive tract, particularly if there are strictures or other abnormalities. This is rare, and doctors will assess the risk beforehand.
-
Discomfort: Some patients may experience mild discomfort or a feeling of fullness while the capsule moves through the GI tract.
-
Incomplete results: In some cases, the capsule may not capture enough images due to a problem in the intestines or the movement of the capsule. This may require further testing.
It is important to discuss any concerns or pre-existing conditions with your doctor before the procedure.
9. What happens after wireless capsule endoscopy?
After the procedure, you can resume your normal activities. You will need to:
-
Return the recording device: Once the capsule has passed through the digestive system, the data from the external receiver will be downloaded, and your doctor will review the images.
-
Pass the capsule: The capsule will be naturally excreted in your stool within 24-48 hours.
-
Follow-up appointment: Your doctor will discuss the findings with you after reviewing the images and recommend any further action if necessary.
The results can usually be available within a few days after the procedure.
10. How much does wireless capsule endoscopy cost?
The cost of wireless capsule endoscopy can vary depending on the country, healthcare facility, and whether it's covered by insurance. On average, the procedure can cost anywhere from $1,000 to $3,000 or more.
Insurance coverage may be available, especially if the procedure is medically necessary (e.g., for diagnosing gastrointestinal bleeding or evaluating Crohn's disease). Be sure to check with your healthcare provider or insurance company for specific details regarding coverage.


