Introduction to Antrostomy
Antrostomyis a surgical procedure performed to create an artificial opening into the maxillary sinus, one of the paranasal sinuses located within the maxillary bone of the face. The main purpose of this operation is to improve drainage, ventilation, and access to the sinus cavity, especially in cases where the natural opening is blocked due to chronic sinusitis, infection, polyps, or other pathological conditions. By establishing a new or enlarged passage between the sinus and the nasal cavity, antrostomy helps in clearing accumulated secretions, reducing infection, and restoring normal sinus function.
The procedure can be performed through two main approaches: the traditional Caldwell-Luc operation, which involves making an incision in the upper gum to access the sinus directly, and the modern endoscopic middle meatal antrostomy, which is minimally invasive and done through the nasal cavity using an endoscope. The endoscopic method has largely replaced the older technique because it causes less tissue damage, ensures faster recovery, and provides better visualization of the sinus structures.
Antrostomy is commonly indicated for patients suffering from chronic maxillary sinusitis resistant to medical treatment, removal of foreign bodies, cysts, or tumors, and for managing dental complications involving the sinus. Overall, it is an important and effective surgical procedure in otolaryngology that significantly improves sinus drainage, relieves symptoms, and enhances the patient's quality of life.
Causes and Risk (Why an Antrostomy Becomes Necessary)
An antrostomy (usually referring to maxillary antrostomy) becomes necessary when there is chronic or recurrent blockage, infection, or inflammation in the maxillary sinus that fails to respond to medical therapy. The procedure creates a surgical opening between the maxillary sinus and nasal cavity to facilitate drainage, ventilation, and healing.
Common indications
-
Chronic rhinosinusitis with persistent maxillary disease despite adequate medical therapy (topical steroids, antibiotics, saline irrigations). FESS with maxillary antrostomy is indicated for refractory disease.
-
Antrochoanal polyps (ACPs) - solitary polyps originating in the maxillary antrum that extend into the choana; endoscopic antrostomy with complete antral removal reduces recurrence.
-
Fungal ball of the maxillary sinus - requires endoscopic antrostomy and removal. MMA is commonly used for fungal balls and fungal sinusitis.
-
Odontogenic maxillary sinusitis - dental infections, root canal material, or implants that breach the sinus often need antrostomy for drainage and removal of offending materials. Sometimes combined dental/sinus approach is required.
-
Recurrent acute sinusitis with anatomic obstruction (e.g., concha bullosa, deviated septum causing ostial obstruction) - when anatomy blocks the ostium repeatedly.
Risk factors that lead to needing surgery
-
Failed maximal medical therapy (topical steroid + antibiotics when indicated).
-
Anatomic variants: narrow infundibulum, a hypertrophied uncinate process, concha bullosa, or lateralized middle turbinate.
-
Prior dental work with complications (tooth infection, implant migration).
-
Large antral polyps or fungal disease.
-
Conditions that impair mucociliary clearance (cystic fibrosis, immune deficiency).
Note for clinicians: patient selection should follow guideline-based indications for FESS / sinus surgery; isolated maxillary antrostomy is useful when disease is primarily maxillary and anatomy permits endoscopic access. Insufficient attention to mucosal disease or incomplete procedures (residual antral disease) are common causes of revision.
Symptoms and Signs (When Patients Present)
Patients who eventually require anterior resection (often for rectal or low sigmoid colon cancer) commonly present with both rectal and general symptoms, depending on tumor size, location, and stage. When evaluating for surgery, attention is given to persistent or alarming bowel changes and signs of local or advanced disease.
Typical symptoms suggesting maxillary sinus disease
-
Facial pressure/pain localized to cheek or upper teeth (often worse bending forward)
-
Nasal obstruction or congestion
-
Purulent (thick/yellow/green) nasal discharge, post-nasal drip
-
Reduced or lost sense of smell (hyposmia/anosmia)
-
Recurrent or persistent sinus infections despite treatment
-
Fever and malaise in acute exacerbations; chronic disease often has more subtle systemic signs
-
Dental pain or sense of sinus pressure after dental treatment (odontogenic cases)
Signs on examination
-
Purulent secretion in the middle meatus on nasal endoscopy
-
Mucosal edema, polypoid change, or visible antrochoanal polyp
-
Nasal septal deviation, turbinate hypertrophy, mucous crusting (especially post op or in chronic disease)
-
Tenderness over maxillary sinus to palpation in acute disease (limited sensitivity)
-
Dental exam may reveal a dental source (caries, abscess, implant displacement).
Important red flags: proptosis, visual disturbance, severe unilateral facial swelling, neurologic signs, or high fever - these suggest complicated acute sinusitis (orbital or intracranial extension) and need urgent ENT evaluation and imaging.
Diagnosis of Maxillary Sinus Disease (Preoperative Workup)
Diagnosis and preoperative workup for maxillary sinus disease (especially in cases where surgery like antrostomy may be needed) rely on a thorough combination of clinical evaluation and advanced imaging to assess the underlying pathology, its extent, and anatomical variations-ensuring safe and effective surgical planning.
4.1 Clinical assessment
-
Detailed history: duration, prior treatments, dental history, prior sinus surgery, asthma/allergies, immunodeficiency.
-
Nasal endoscopy: essential outpatient exam to visualize middle meatus, ostium, polyps, or purulence. Endoscopy detects findings not visible on anterior rhinoscopy.
4.2 Imaging
-
CT scan of the paranasal sinuses (non-contrast, axial/coronal) is the gold standard for surgical planning - shows opacification, ostiomeatal complex anatomy, antral anatomy, bony details, mucoceles, polyps, dental roots, and prior hardware. CT also helps plan whether a middle meatal antrostomy will access the diseased antral recess.
-
MRI is used selectively (suspected fungal invasion, soft-tissue neoplasm, or intraorbital/intracranial complications).
4.3 Microbiology / Labs
-
Cultures from middle meatal or sinus aspirate can guide therapy in refractory or complicated infections, and when unusual organisms (fungus, resistant bacteria) or odontogenic organisms are suspected.
-
Blood tests are used when systemic disease or complications are suspected.
4.4 Dental assessment
-
When odontogenic sinusitis is suspected (unilateral maxillary disease, history of dental procedure, periapical lucency on imaging), coordinate with dental/oral surgery for source control; removal of offending dental material may be required.
When to operate
Surgery (antrostomy ± additional procedures) is considered when:
-
Disease persists despite appropriate medical therapy (saline irrigations, topical steroids ± antibiotics) or
-
Clear anatomic obstruction exists (e.g., obstructed ostium, large polyps) or
-
Complications (mucocele, fungal ball), or
-
There is an odontogenic source requiring sinus access and drainage.
Treatment Options (How Antrostomy Is Performed & Alternatives)
Antrostomy-most often referring to maxillary antrostomy-is a surgical procedure to enlarge the natural opening of the maxillary sinus, restoring drainage and relieving chronic or recurrent sinus disease. It can be performed using different surgical techniques, and is usually chosen when medical management of chronic sinusitis fails.
5.1 Overview of surgical options
-
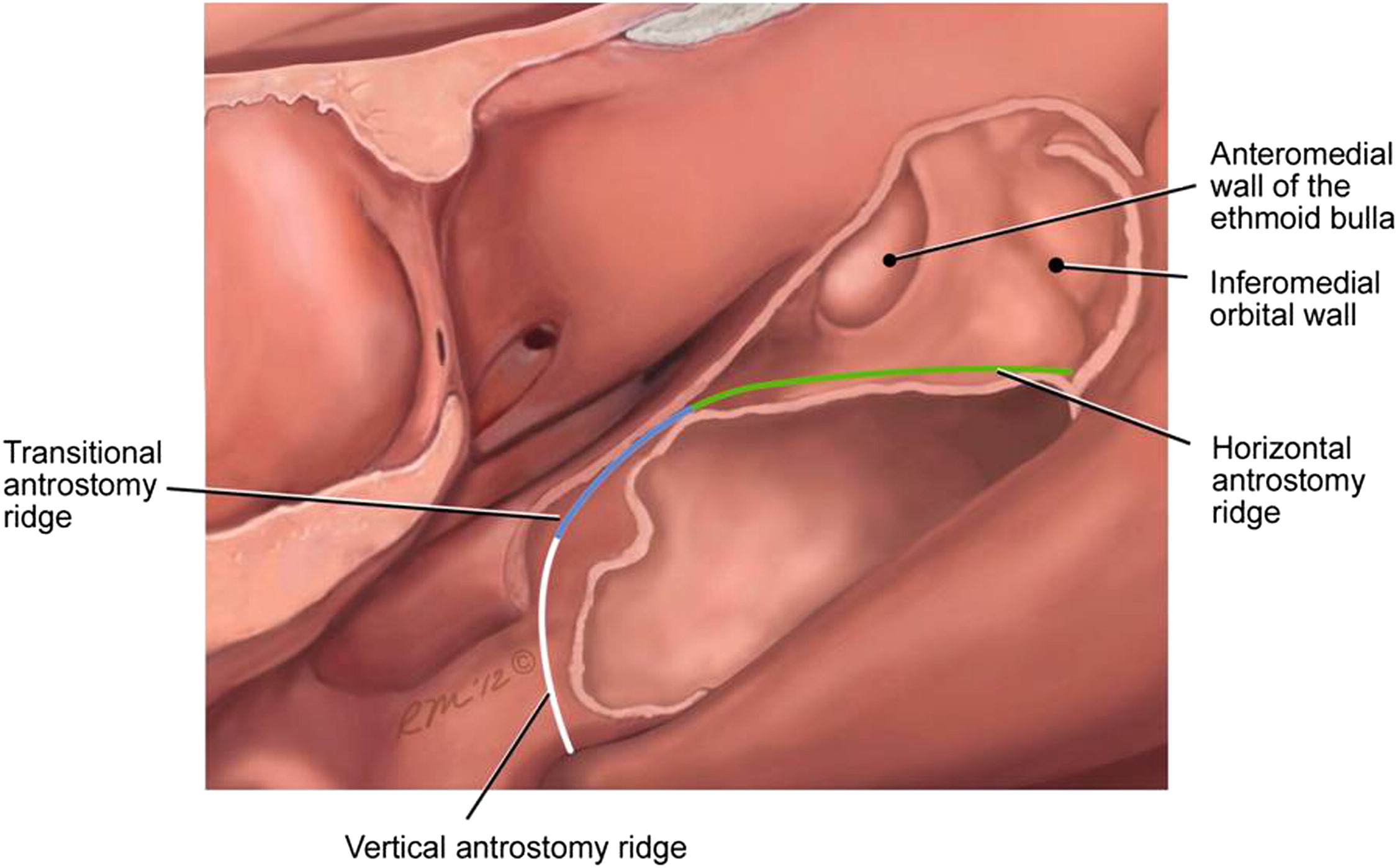
Endoscopic Middle Meatal Antrostomy (MMA) - currently the most common procedure: uncinectomy (removal of uncinate process) followed by enlargement of the natural maxillary ostium via the middle meatus to create a larger drainage pathway. Typically performed under general anesthesia using nasal endoscopes.
-
Extended or Inferior Antrostomy / Inferior Meatal Antrostomy (IMA) - sometimes used for disease in anterior or inferior recesses not reachable via MMA, or in revision cases. IMA creates an opening in the inferior meatus (nasal floor) into the antrum; used more selectively today.
-
Caldwell-Luc (external) approach - external sublabial entrance into the antrum; historically used for chronic maxillary disease and removal of foreign bodies but largely replaced by endoscopic techniques. May still be used for certain odontogenic cases or when endoscopic access is insufficient. Modified Caldwell-Luc approaches exist but are less favored due to morbidities (infraorbital nerve injury, facial numbness, cheek swelling).
5.2 Typical operative steps (endoscopic MMA)
-
Nasal decongestion and local anaesthesia ± general anesthesia.
-
Endoscopic uncinectomy to expose the natural ostium of the maxillary sinus.
-
Creation and enlargement of the antrostomy (middle meatal antrostomy) - remove bone at the ostium to create a patent window large enough for drainage and scope access.
-
Suctioning of purulence, removal of polyps/ fungal debris, or targeted antral instrumentation (microdebrider, curved instruments) to clear disease.
-
Inspection for additional pathology (ethmoid disease, frontal recess disease) and address concurrently when indicated.
-
Haemostasis; placement of dissolvable packing or small non-dissolving packs as needed. Postoperative saline rinses and topical nasal steroids are typically resumed as directed.
5.3 Adjunct techniques
-
Balloon sinuplasty enlarges the natural ostium using an intraluminal balloon under endoscopic and/or fluoroscopic guidance - used mainly in selected chronic sinusitis without polyps and with limited disease; less useful for fungal disease, polyps or complex anatomy.
-
Image guidance (neuronavigation) is recommended for complex anatomy or revision surgery to reduce risk of orbital or skull base injury.
-
Use of topical antifungals, antibiotics tailored to culture results for fungal ball or chronic bacterial disease.
5.4 Special cases
-
Antrochoanal polyps (ACPs): wide middle meatal antrostomy or extended MMA that allows complete antral removal reduces recurrence; simple polypectomy is associated with high recurrence if antral component remains.
-
Odontogenic sinusitis: may require combined dental and endoscopic approaches; remove infected tooth or foreign body plus maxillary antrostomy for drainage. Outcomes are improved when both dental and sinus sources are treated.
Prevention and Management (Before & After Antrostomy)
Prevention and management before and after maxillary antrostomy (endoscopic sinus surgery) revolve around optimizing sinus health preoperatively, minimizing surgical risks, and supporting ideal healing and function after the procedure. Coordinated medical care, patient adherence, and early intervention for complications ensure the best long-term outcomes.
6.1 Preoperative optimization
-
Medical therapy first: ensure an adequate trial of medical therapy (intranasal corticosteroids, nasal saline irrigations, targeted antibiotics if bacterial infection suspected). Surgery is for refractory disease or structural causes.
-
Treat dental sources pre-op: coordinate with dental/oral teams to address odontogenic triggers.
-
Smoking cessation improves postoperative mucosal healing and reduces infection risk.
-
Pre-op counseling: explain nasal packing expectations, postoperative saline rinses, temporary smell changes, and timeline of recovery.
6.2 Postoperative care (standard modern ERAS-type approach for sinus surgery)
-
Nasal saline irrigations begin soon after surgery to remove crusts and keep the antrostomy patent; frequency varies by surgeon but often multiple times daily early on.
-
Topical steroid sprays / irrigations usually restarted within 1-2 weeks to control mucosal inflammation (surgeon-dependent).
-
Antibiotics are used when bacterial infection or odontogenic source indicated; routine prolonged antibiotics are not universally recommended.
-
Avoid nose blowing, heavy lifting, air travel, and swimming for the first 1-2 weeks or per surgeon guidance (to reduce risk of bleeding or pressure changes).
-
Follow-up nasal endoscopy 1-4 weeks post op to debride crusts, assess mucosa, and confirm antral drainage; additional care visits as needed. Early endoscopic debridement reduces adhesions and improves outcomes.
6.3 Long-term management and prevention of recurrence
-
Continued nasal hygiene (saline irrigations) and topical steroid therapy when indicated (chronic rhinosinusitis with polyps).
-
Address comorbidities (allergic rhinitis, asthma) with appropriate medical therapy to reduce recurrence.
-
Smoking cessation and dental care to reduce risk of recurrent or odontogenic disease.
-
Timely revision endoscopic surgery may be indicated for recurrent disease, scarring/stenosis of the antrostomy, or persistent antral disease; careful revision planning uses image guidance and addresses the cause (residual disease, narrow antrostomy, uncinate remnant).
Complications of Antrostomy
Endoscopic antrostomy is generally safe, but complications-especially in revision or complex cases-may occur. Overall significant complication rates for FESS (including antrostomy) are low, but minor complications are more common.
7.1 Early (intraoperative/perioperative) complications
-
Bleeding - usually minor; severe bleeding rare but may require packing or re-exploration. Vascular anatomy variability can increase risk.
-
Orbital injury - from lateral or superior dissection; may cause orbital hematoma, diplopia, or vision changes (rare but serious) - image guidance reduces this risk.
-
CSF leak / skull base injury - rare, more likely in revision surgery or when disease extends superiorly. Prompt recognition and repair are essential.
-
Tooth or dental root injury in inferior antral access or Caldwell-Luc approaches (less common with endoscopic MMA).
7.2 Early postoperative complications
-
Infection / persistent or recurrent sinusitis - may require further medical therapy or revision surgery.
-
Crusting / synechiae (adhesions) - can obstruct drainage if not addressed by early debridement.
-
Pain, nasal obstruction, minor epistaxis - common and usually self-limited.
7.3 Late complications
-
Antrostomy stenosis or closure - can cause recurrence of symptoms; may need endoscopic revision and enlargement (extended MMA or inferior antrostomy) if persistent disease is present.
-
Persistent antral disease - missed fungal debris or odontogenic source causing recalcitrant infection; combined dental/sinus management often needed.
-
Facial numbness or infraorbital nerve dysfunction (especially with Caldwell-Luc approach).
7.4 Rates & risk mitigation
-
Major complications (vision loss, CSF leak) are rare (<1-2% in experienced hands); minor complications and need for revision are more common - the literature reports variable revision rates depending on indication and surgeon experience. Use of image guidance, meticulous technique, early follow-up debridement and addressing all diseased areas in the same sitting reduces revision rates.
Living with the Condition / After Antrostomy - Recovery & Expectations
Recovery after a maxillary antrostomy (endoscopic sinus surgery) is typically smooth, with most patients experiencing noticeable symptom relief and improved sinus drainage within a few weeks. The recovery period focuses on restoring sinus function, controlling swelling, and preventing infection while allowing the mucosa to heal.
1. Early recovery timeline
-
Immediate post-op: mild-moderate facial pressure, nasal congestion, crusting - analgesia and saline irrigation help. Most patients go home same day or next day depending on extent.
-
First 1-2 weeks: packing (if used) dissolves or is removed; begin gentle saline irrigations; avoid nose blowing or heavy exertion per surgeon's advice.
-
Weeks 2-6: repeated clinic endoscopies for crust removal and mucosal healing as recommended; topical steroids often started or resumed.
8.2 Functional outcomes and symptom improvement
-
Majority of appropriately selected patients experience significant improvement in facial pressure, nasal discharge, and overall sinus-related quality of life after antrostomy ± FESS. Improvements may continue over months as mucosa heals and chronic inflammation resolves.
8.3 When symptoms persist or recur
-
Persistent unilateral symptoms should prompt repeat endoscopic evaluation and CT imaging to look for residual antral disease, odontogenic sources, antrostomy stenosis, or foreign bodies. Revision endoscopic antrostomy or combined dental interventions may be necessary.
8.4 Practical patient advice
-
Adhere to saline irrigation regimen and follow-up appointments - these significantly reduce crusting and adhesions.
-
Restart topical steroids as advised to suppress inflammation.
-
Maintain dental hygiene and follow dental advice if odontogenic disease was involved.
-
Report any visual changes, severe pain, high fever, or neurological signs urgently.
Top 10 Frequently Asked Questions about Antrostomy
1. What is Antrostomy and why is it performed?
Antrostomy is a surgical procedure that creates an opening in the maxillary sinus, one of the air-filled cavities located behind the cheekbones. The main goal of antrostomy is to improve sinus drainage and ventilation, particularly when the natural sinus openings are blocked.
Blocked sinuses can lead to chronic infections, facial pain, headaches, nasal congestion, and pressure, often resistant to medications. By surgically enlarging the sinus opening, antrostomy allows mucus to drain naturally, reduces infection risk, and restores normal airflow and sinus function.
It is frequently performed for conditions such as:
-
Chronic or recurrent sinusitis that does not respond to medications
-
Nasal polyps or cysts causing blockage
-
Structural abnormalities of the sinus or nasal passages
-
Obstructions after previous sinus surgery
Modern techniques, particularly endoscopic antrostomy, allow for minimally invasive surgery with faster recovery, fewer complications, and minimal disruption to surrounding tissues.
2. Who is an ideal candidate for Antrostomy?
Not every patient with sinus problems requires antrostomy. Candidates are typically those who:
-
Have persistent sinus infections lasting 12 weeks or more
-
Experience frequent flare-ups despite antibiotics, nasal sprays, or decongestants
-
Suffer from obstruction-related symptoms such as facial pressure, postnasal drip, headaches, and difficulty breathing
-
Have nasal polyps, cysts, or anatomical obstructions blocking the sinus
-
Are in overall good health to tolerate surgery
Before recommending surgery, an ENT specialist performs a detailed evaluation, including nasal endoscopy, CT scans, and medical history review, to confirm the need for antrostomy.
3. How is Antrostomy performed?
Antrostomy can be performed as endoscopic (minimally invasive) or, in rare cases, open surgery. The endoscopic approach is preferred for most patients because it reduces recovery time and risk of complications.
The procedure generally involves:
-
Administration of anesthesia - either local with sedation or general anesthesia depending on patient preference and complexity.
-
Endoscopic access through the nasal cavity - a small, flexible camera (endoscope) allows the surgeon to visualize the sinus.
-
Creation or enlargement of the sinus opening - using specialized instruments, the maxillary sinus opening is widened to allow proper drainage.
-
Removal of obstructive tissue - nasal polyps, cysts, or scar tissue may be carefully excised.
-
Placement of temporary stents or packing, if needed, to maintain patency during healing.
Endoscopic antrostomy is usually an outpatient procedure, allowing most patients to go home the same day.
4. What are the benefits of Antrostomy?
Antrostomy provides numerous benefits for patients suffering from chronic or obstructive sinus issues:
-
Improved sinus drainage and reduced infection risk
-
Alleviation of facial pressure, headaches, and congestion
-
Minimally invasive approach preserves normal nasal structures
-
Short recovery time and reduced hospital stay compared to open surgery
-
Enhanced effectiveness of topical medications post-surgery, such as nasal sprays
-
Long-term relief for patients with nasal polyps, cysts, or anatomical obstructions
This procedure significantly improves quality of life for patients with chronic sinus disease.
5. What is the recovery process after Antrostomy?
Recovery depends on the extent of the surgery, but typical timelines are:
-
Day 0-2: Mild discomfort, nasal congestion, and slight bleeding are common. Pain is managed with over-the-counter or prescribed medications.
-
Week 1: Patients can usually return to light daily activities. Nasal saline irrigation may be recommended to aid healing.
-
Week 2-4: Swelling decreases, sinus drainage improves, and any packing or stents may be removed.
-
1-2 months: Most patients experience full symptom relief, though complete healing may take longer in cases of severe chronic sinusitis or polyp removal.
Regular follow-up appointments with the ENT surgeon are critical to monitor healing and prevent recurrence.
6. Are there any risks or complications associated with Antrostomy?
Antrostomy is generally safe, especially when performed by an experienced ENT surgeon. However, as with any surgery, there are potential risks:
-
Minor bleeding from the nasal passages
-
Infection, which is uncommon but can occur postoperatively
-
Scarring or narrowing of the sinus opening if healing is abnormal
-
Damage to surrounding structures, such as the eyes, teeth, or nasal cartilage (rare)
-
Persistent or recurrent sinusitis, particularly if underlying causes such as allergies or anatomical variations are not addressed
Careful surgical planning, precise technique, and diligent post-operative care minimize these risks.
7. How soon will I notice relief after Antrostomy?
Many patients experience immediate improvement in nasal breathing and sinus drainage within a few days after surgery.
-
Some mild congestion or discomfort may persist for 1-2 weeks.
-
Full resolution of chronic sinus symptoms, including pressure, headaches, and postnasal drip, typically occurs within 4-6 weeks.
-
Long-term improvement is enhanced when nasal irrigation and follow-up care are consistently practiced.
8. Can Antrostomy be combined with other procedures?
Yes, antrostomy is often performed alongside other sinus or nasal procedures to address multiple issues at once:
-
Endoscopic sinus surgery (ESS) for multi-sinus blockages
-
Polypectomy to remove nasal polyps
-
Septoplasty to correct deviated septum
-
Turbinate reduction to improve airflow
Combining procedures improves overall sinus function and reduces the likelihood of needing additional surgeries in the future.
9. How should I prepare for Antrostomy surgery?
Preparation is important for a safe and effective procedure:
-
Preoperative evaluation including medical history, nasal endoscopy, and CT scans
-
Medication review, especially anticoagulants or anti-inflammatory drugs
-
Smoking cessation to promote healing
-
Arranging post-surgery support for transportation and daily care
-
Nasal hygiene may be advised to reduce bacterial load before surgery
Your ENT surgeon will provide a personalized preparation plan for optimal outcomes.
10. Is Antrostomy a permanent solution for sinus problems?
Antrostomy can provide long-lasting relief for patients with chronic sinus blockages, especially when combined with proper post-operative care. However, the following factors may influence long-term outcomes:
-
Allergic rhinitis or chronic inflammation may cause recurrence of symptoms
-
Structural issues, if not fully addressed, can lead to partial recurrence
-
Patient adherence to nasal irrigation and follow-up care is critical
With proper care and follow-up, most patients experience significant and enduring improvement in sinus drainage, breathing, and overall quality of life.


