Introduction to Atherectomy
Atherectomy is an advanced endovascular procedure used to remove or debulk atherosclerotic plaque from the interior of an artery, thereby restoring or improving blood flow. Unlike balloon angioplasty (which widens an artery by compressing the plaque) or stenting (which props the artery open), atherectomy physically removes or modifies material obstructing the lumen—particularly useful in heavily calcified or fibrotic lesions that are resistant to dilation.
Plaque inside arteries typically comprises lipid cores, fibrous tissue, calcium deposits, and inflammatory elements. Over time, plaques can harden and encroach upon the lumen, limiting perfusion to downstream tissues (such as muscle, skin, or organs). In selected cases, when symptoms are significant and less invasive therapies are insufficient or at high risk of failure, atherectomy is considered.
There are multiple atherectomy modalities, including:
-
Rotational atherectomy (a diamond-tipped burr spins at high rpm to sand plaque)
-
Orbital atherectomy (an eccentrically mounted crown orbits within the vessel lumen to erode plaque)
-
Laser atherectomy (ultraviolet laser pulses vaporize plaque)
-
Directional atherectomy, aspiration atherectomy, and other hybrid variants
These techniques are used in both coronary (heart vessel) and peripheral arterial disease (PAD) (limbs, especially legs) settings. The aim is plaque modification, vessel compliance improvement, and facilitation of adjunctive therapies like balloon angioplasty or stent deployment.
While earlier atherectomy was used mainly for debulking, modern usage generally focuses on preparing the vessel (i.e., modifying plaque so that further interventions are safer and more effective). Recent studies and expert consensus continue to refine indications, technique, and patient selection.
Despite its promise, the evidence base is evolving—some trials have not demonstrated superiority in all settings, and complication risk remains a key consideration.
Causes & Risk Factors (Underlying Disease Leading to Atherectomy Use)
Because atherectomy is a treatment rather than a disease itself, this section basically describes the mechanisms and risk factors behind the underlying atherosclerotic disease that might prompt consideration for atherectomy.
Pathophysiology: How Plaque Forms & Advances
-
Endothelial injury / dysfunction
Chronic injury to the inner endothelial lining (due to hypertension, elevated LDL cholesterol, smoking, diabetes) causes increased permeability, inflammation, and adhesion of monocytes. -
Lipid infiltration & inflammation
Low-density lipoprotein (LDL) particles enter the arterial intima, become oxidized, and trigger inflammatory pathways. Macrophages and foam cells accumulate, and a necrotic lipid core may develop. -
Smooth muscle cell migration and extracellular matrix deposition
Smooth muscle cells migrate from the media into the intima, laying down collagen and elastin, contributing to the fibrous cap of the plaque. -
Calcification
Over time, microcalcification can grow into dense calcium deposits. These stiff, rigid portions are particularly resistant to expansion during angioplasty. It is often these calcified plaques that are targeted by atherectomy. -
Progression & remodeling
Plaques can expand inward (narrowing the lumen) or outward (arterial remodeling). When they impinge significantly on the lumen, ischemic symptoms may appear. Plaque rupture or erosion may precipitate acute events (e.g., myocardial infarction or acute limb ischemia).
Lesions that are long, tortuous, heavily calcified, or reinforced after prior interventions are especially challenging for plain angioplasty or stenting alone, making them candidates for atherectomy.
Risk Factors for Atherosclerosis / Plaque Burden
These are the classic modifiable and non-modifiable risk factors that drive plaque formation and progression:
-
High LDL cholesterol / low HDL cholesterol
-
Hypertension (high blood pressure)
-
Diabetes mellitus (especially poorly controlled)
-
Smoking / tobacco use
-
Obesity / metabolic syndrome
-
Sedentary lifestyle
-
Chronic kidney disease
-
Older age
-
Male gender (in many settings)
-
Family history of premature cardiovascular disease
-
Chronic inflammation / autoimmune disease
These factors accelerate endothelial injury, lipid infiltration, inflammatory activity, and calcification.
Lesion-Specific & Procedure-Specific Risks
Certain lesion or procedural features increase both the challenge of the intervention and the risk of complications:
-
Heavy calcification (superficial or deep)
-
Long lesions or diffuse disease
-
Vessel tortuosity / angulation
-
Small vessel diameter
-
Lesions crossing bifurcations
-
Prior stents or restenosis
-
Collateral circulation limited (so distal embolization is more dangerous)
-
Comorbid conditions (e.g., poor renal function, bleeding risk, frailty)
Given these risks, careful patient and lesion selection is critical, and atherectomy is usually reserved for complex cases where its mechanical advantages outweigh additional procedural risk.
Symptoms & Clinical Presentation
Again, to clarify: atherectomy is a treatment. The symptoms and signs relate to the underlying arterial disease (coronary or peripheral) that led to the need for intervention.
Coronary (Heart Vessels) - When Atherectomy Is Applied
If the atherosclerotic lesion is in a coronary artery, symptoms typically reflect myocardial ischemia:
-
Angina pectoris (chest pain or discomfort) — often exertional, sometimes at rest
-
Shortness of breath (dyspnea)
-
Reduced exercise tolerance / fatigue
-
Unstable angina or acute coronary syndrome
-
Myocardial infarction (heart attack) — if plaque ruptures or vessel is fully occluded
In heavily calcified, rigid lesions, attempts to dilate or stent may fail, or stent expansion may be suboptimal, prompting use of atherectomy as a vessel preparation tool.
Peripheral Arterial Disease (PAD) - Most Common Indication for Atherectomy Use
When the arterial disease affects the limbs (especially lower extremities), symptoms may include:
-
Intermittent claudication: cramping, pain, fatigue in muscles (calf, thigh, buttocks) during walking, relieved by rest
-
Rest pain / ischemic pain: particularly in feet or toes when lying down, often more when elevated or at night
-
Nonhealing ulcers / wounds / gangrene: due to insufficient perfusion
-
Coldness, numbness, tingling, or changes in skin color / temperature
-
Weak or absent pulses in the foot or leg
-
Delayed capillary refill, hair loss on legs, shiny skin
The severity of symptoms and impact on daily life often dictates urgency of intervention. Atherectomy may be used when conservative measures and simpler endovascular approaches are insufficient.
It is critical for clinicians to distinguish vascular vs. neurogenic or musculoskeletal causes of leg pain (e.g., spinal stenosis, neuropathy). Noninvasive testing is often the first step.
Diagnosis of Acupressure Therapy
Before proceeding with atherectomy, comprehensive assessment is essential to confirm the lesion anatomy, physiological significance, and risks. Here's how:
Clinical Assessment & History
-
Detailed symptom history: onset, frequency, triggers, location
-
Assessment of risk factors: lipids, hypertension, diabetes, smoking
-
Physical exam: palpation of pulses, auscultation for bruits, skin changes, ulceration
-
Assessment of comorbidities (renal function, bleeding risk, cardiac status)
Noninvasive Vascular Testing
-
Ankle-brachial index (ABI) / toe-brachial index (TBI)
-
Segmental limb pressures / plethysmography
-
Duplex ultrasound / Doppler: assesses blood flow, velocity, degree of stenosis
-
CT angiography (CTA) or MR angiography (MRA): visualize vessel course, calcification, lesion length
-
Stress testing / functional imaging (for coronary disease)
These tests help localize disease, grade severity, and plan the intervention.
Invasive Imaging & Hemodynamic Assessment
-
Angiography (digital subtraction angiography) is the gold standard for mapping lesion location, length, and collateral circulation
-
Intravascular imaging (IVUS, OCT) can assess plaque morphology, depth of calcification, lumen dimensions, and guide device selection.
-
Fractional flow reserve (FFR) or other physiological metrics may help determine the need for revascularization in coronary settings
-
Intravascular lithotripsy (in some centers) or other adjunct imaging may be used for particularly calcified lesions
Lesion Classification & Risk Stratification
When planning atherectomy, operators evaluate:
-
Depth and circumferential extent of calcification (i.e., superficial vs. deep calcium, number of quadrants)
-
Lesion length
-
Vessel diameter and tortuosity
-
Presence of side branches or bifurcations
-
Access route feasibility
-
Risk of distal embolization
-
Patient co-morbidities
Expert consensus documents have provided guidance on burr/artery size ratios, rhythm of passes, and imaging integration.
Indications for Atherectomy Use
While not all lesions require atherectomy, some indications include:
-
Heavily calcified lesions that do not respond to balloon dilation
-
Lesions that may prevent optimal stent expansion
-
Ostial lesions, bifurcations, in-stent restenosis with rigid plaque
-
Lesion preparation before drug-coated balloon or stent deployment
-
Situations where standard ballooning would risk dissection or embolization
Contraindications or unsuitable settings include:
-
Lesions with heavy thrombus burden (risk of distal embolization)
-
Soft, noncalcified lesions where ballooning suffices
-
Vessels too small to safely deliver devices
-
Cases where surgical bypass is more appropriate
Treatment Options & Role of Atherectomy
This section explores how atherectomy fits into the full spectrum of interventions, the various techniques, procedural steps, and pros/cons.
Broad Treatment Landscape for Atherosclerotic Lesions
Before discussing atherectomy in depth, it helps to see the full range of therapies:
-
Lifestyle and medical therapy: statins, antihypertensives, antiplatelets, glucose control, exercise, diet, smoking cessation
-
Balloon angioplasty (PTA) — inflating a balloon to widen the vessel
-
Stenting (bare-metal, drug-eluting) — to scaffold the vessel open
-
Drug-coated balloons (DCB) — for certain peripheral lesions, avoids permanent implant
-
Endarterectomy (surgical removal of plaque, e.g. carotid endarterectomy)
-
Bypass surgery — for extensive disease when endovascular options are limited
-
Hybrid therapy — combinations of surgery and endovascular
-
Atherectomy — as a complement or preparatory tool
In practice, many revascularization strategies blend therapies (e.g., atherectomy + balloon + stent) to achieve optimal results.
Atherectomy Modalities: Mechanisms & Uses
Rotational Atherectomy
-
Uses a diamond-coated burr spinning at very high speeds (e.g., 160,000-200,000 rpm)
-
The burr abrades superficial calcification and creates micro-fractures, improving vessel compliance
-
Usually used in coronary settings for heavily calcified lesions before stenting.
-
Modern consensus suggests limiting total run time, using low burr:artery ratio, and integrating intravascular imaging.
Orbital Atherectomy
-
Uses an eccentrically mounted crown that orbits within the vessel lumen
-
The orbiting motion allows plaque sanding longitudinally and circumferentially
-
Can reach slightly larger vessel diameters than similarly sized rotational burrs
-
Some flexibility in rotational speed adjustments
-
The recent ECLIPSE trial (2025) compared orbital atherectomy + DES vs. conventional PCI + DES in severely calcified coronary lesions and found no significant superiority of the atherectomy arm in target vessel failure at 1 year, though numerically the burr group had a slightly higher 30-day mortality, raising safety scrutiny.
Laser Atherectomy
-
Uses short-pulse ultraviolet laser energy (e.g., 355 nm) to vaporize plaque and create shock waves that fracture calcium
-
It is particularly advantageous in calcified peripheral arteries, below-knee vessels, restenotic lesions, or in lesions where mechanical burrs may not navigate
-
Recent data from the Auryon laser system show promising safety and efficacy: in 102 patients with complex lesions, a 12-month target lesion revascularization (TLR) of ~6.7% and amputation rate of 2.2%.
-
Helps reduce bailout stenting, dissections, and may better treat in-stent restenosis or below-knee disease.
Directional & Aspiration Atherectomy
-
Directional atherectomy: uses a side-cutting blade to shave plaque in a targeted direction; often paired with aspiration
-
Aspiration atherectomy: uses suction to remove the plaque debris
-
These are used in peripheral settings, and some cases in coronary intervention, often when lesions are focal or in softer plaque regions
Hybrid / Adjunct Approaches
-
Many operators use atherectomy + balloon angioplasty + drug-coated balloon / stent placement
-
Vessel preparation: Atherectomy is commonly used as a preparatory step to facilitate subsequent dilation and stent expansion
-
Embolic protection devices / distal filters may be deployed in conjunction to catch debris and reduce distal embolization
-
Sequential therapy: start with atherectomy, then assess whether further intervention (ballooning or stenting) is needed
Procedural Technique & Best Practices
While each device has nuances, general principles apply across atherectomy procedures:
-
Vascular Access & Guide Catheter Selection
-
Femoral or radial access can be used (radial increasingly favored for patient comfort)
-
Guide catheter size depends on device (commonly 6-7 Fr, sometimes up to 7-8 Fr)
-
Ensure support and coaxial alignment
-
-
Guidewire Crossing & Imaging
-
Cross the lesion with an appropriate wire (rotawire for rotational systems)
-
Use intravascular imaging (IVUS, OCT) if available, to guide burr sizing, length, and strategy
-
Imaging helps assess calcium depth, vessel size, and guide dosing
-
-
Device Preparation & Flushing
-
Many systems require continuous lubrication, cooling, and flush solutions to reduce burr heating and prevent entrapment
-
For rotational systems, maintaining brake release and safe retrieval practices is essential
-
-
“Pecking” or “Pulsed” Technique
-
Rather than continuously rotational ablation, devices are advanced in controlled, short runs (e.g., 10-15 s) with intermittent withdrawal
-
This “pecking” technique reduces heat, vessel trauma, and risk of complications
-
Some protocols limit total ablation time (e.g. ≤ 5 minutes total for certain systems) .
-
-
Adjunctive Balloon or Stent
-
After plaque modification, balloon angioplasty is usually performed to further open the lumen
-
In coronary interventions, stenting (typically drug-eluting) is often deployed
-
In peripheral disease, drug-coated balloons or stents may follow depending on the lesion and operator preference
-
-
Monitoring & Safety Measures
-
Continuous monitoring of ECG, hemodynamics, and distal flow
-
Keep ablation runs short, pause between runs to reassess
-
Use distal protection or aspiration when feasible
-
Be ready to manage complications (e.g., vessel dissection, perforation, slow flow)
-
-
Post-Procedure Hemostasis & Recovery
-
After catheter removal, the puncture site requires care (manual compression, closure devices)
-
Patients often lie flat for several hours to reduce bleeding risk
-
Monitor vital signs, access site, limb perfusion
-
European and Japanese expert consensus statements detail refined protocols, such as burr sizing strategies, vessel preparation, and intravascular imaging integration.
Advantages, Limitations & Evidence Summary
Advantages:
-
Better lumen gain in heavily calcified lesions
-
Improved vessel compliance before ballooning
-
May reduce stent under-expansion or malapposition
-
Reduced need for oversized stents or excessive balloon inflation
-
Useful in complex anatomies (bifurcations, ostial lesions, in-stent restenosis)
Limitations / Risks:
-
Possibility of distal embolization (plaque fragments lodging in smaller vessels)
-
Vessel dissection, perforation, or burr entrapment
-
Increased procedural time and complexity
-
Cost of devices and reimbursement issues
-
Evidence remains inconclusive in many peripheral settings—some randomized trials did not demonstrate clear benefit over standard endovascular therapy
For example, the ECLIPSE trial (2025) failed to show superiority of orbital atherectomy + DES versus conventional PCI + DES in calcified coronary lesions in terms of target vessel failure at 1 year.
A 2024 review reported that atherectomy use in peripheral interventions in the U.S. has increased (up to 18% of peripheral vascular interventions) but that “high-quality, prospective data” remain sparse.
A systematic review from 2020 (Cochrane) concluded that evidence for atherectomy in PAD is “very uncertain” regarding patency, mortality, and cardiovascular events.
Nonetheless, many operators favor atherectomy in selected high-risk lesions, and ongoing research continues to refine optimal usage.
Prevention & Management (Before and After Atherectomy)
Because atherectomy is a procedural tool, its success and durability depend heavily on robust prevention and post-intervention management.
Primary Prevention (To Avoid Progression to Severe Disease)
-
Lifestyle modifications: heart-healthy diet (e.g. Mediterranean, low in saturated fat), weight management
-
Regular physical activity, walking programs for PAD patients
-
Smoking cessation (one of the strongest modifiable risk factors)
-
Aggressive control of hypertension, diabetes, lipid levels
-
Statin therapy, antiplatelets as indicated by current cardiovascular guidelines
-
Screening & monitoring in high-risk populations
These measures slow plaque progression, stabilize vulnerable plaques, and reduce the overall burden of disease that might require intervention.
Pre-Procedure Optimization
Before undergoing atherectomy, patients should be optimized:
-
Detailed pre-procedural evaluation (renal function, bleeding risk, coagulation profile)
-
Adjust or discontinue antithrombotic medications as appropriate
-
Control of comorbidities (e.g. optimize glycemic control, correct anemia)
-
Imaging review and planning (angiography, CT/MR, intravascular imaging)
-
Pre-procedural patient counseling: expected benefits, risks, post-procedure care, follow-ups
Post-Procedure / Secondary Prevention
To maximize durability and reduce recurrence:
-
Dual or single antiplatelet therapy as indicated (often aspirin ± P2Y12 inhibitor) to reduce thrombosis risk
-
Statin therapy / lipid-lowering therapy to stabilize remaining plaques
-
Strict risk factor control: blood pressure, blood sugar, smoking cessation, diet, exercise
-
Surveillance imaging or functional assessment (e.g. duplex ultrasound, ABI) at periodic intervals
-
Supervised exercise / rehabilitation (especially post-PAD intervention)
-
Close clinical follow-up to detect recurrence, new symptoms, or access site problems
-
Lifestyle counselling & adherence support — long-term behavior changes are pivotal
By combining the mechanical intervention with medical optimization, the chances of restenosis, disease progression, and repeat interventions can be minimized.
Complications & Risks of Atherectomy
As with all invasive vascular procedures, atherectomy carries potential complications. Awareness and mitigation strategies are key to safe practice.
Acute / Procedural Complications
-
Distal embolization or microembolism: dislodged plaque fragments may travel downstream and obstruct smaller vessels
-
Vessel dissection: tearing of arterial wall layers
-
Vessel perforation or rupture (especially in fragile or tortuous vessels)
-
Burr entrapment or device lodging — a rare but serious issue
-
Slow-flow or no-reflow phenomenon (especially in coronary settings, when microcirculation is compromised)
-
Thrombosis / acute closure of the treated vessel
-
Access site complications: hematoma, bleeding, pseudoaneurysm, arteriovenous fistula
-
Contrast-induced nephropathy (from imaging dye)
-
Arrhythmias, hemodynamic instability (especially in coronary procedures)
-
Thermal injury (heat build-up during ablation)
Complication risk is higher in complex, long, calcified, or tortuous lesions. Close procedural vigilance, limiting run time, and use of adjunctive protection (e.g., distal filters) help reduce risk.
Intermediate & Long-Term Complications
-
Restenosis / Re-narrowing due to neointimal hyperplasia or residual plaque
-
Need for repeat revascularization
-
Stent failure / in-stent restenosis (if stents were placed after atherectomy)
-
Progression of disease elsewhere in the vascular tree
-
Loss of vessel compliance / vessel injury leading to scarring
-
Compromised future interventions: excessive vessel damage may limit options
A 2025 retrospective study of aspiration atherectomy in PAD patients (34 cases) showed acceptable short- and medium-term outcomes, but emphasized that more data are needed.
Risk Mitigation Strategies
-
Careful patient and lesion selection
-
Use of intravascular imaging to guide intervention
-
Limit total ablation time and burr size / device aggressiveness
-
Employ distal protection / filters when applicable
-
Use of appropriate anticoagulation / antiplatelet therapy
-
Experienced operators and high-volume centres tend to have lower complication rates
-
Close monitoring during and after the procedure
-
Prompt detection and management of complications (e.g. balloon tamponade for perforation, stent salvage, embolectomy)
Expert consensus statements and guidelines recommend adhering to proven protocols (e.g. gradual burr up-sizing, limiting runs, monitoring) to minimize risk.
Living with the Condition After Atherectomy
Once an atherectomy has been performed, long-term success depends on effective follow-up, risk management, and patient engagement. This section addresses post-procedure care, quality-of-life considerations, surveillance, and expectations.
Immediate Recovery & Post-Procedure Care
-
After the procedure, patients are monitored in a recovery unit or hospital bed
-
Vital signs, puncture site, limb perfusion (or cardiac function) are closely observed
-
Patients often must lie flat for several hours (commonly 4-6 h) to reduce risk of bleeding from the puncture site (especially femoral access)
-
Access site care includes compression, hemostasis, and inspection for hematoma
-
Gradual return to mobility as allowed by the interventionalist
Most patients can return to basic daily activities in a few days, although the pace depends on the complexity, vascular bed treated, and presence of comorbidities.
Follow-Up & Surveillance
-
Schedule follow-up visits to monitor symptoms, access site, pulses, wound healing (if relevant)
-
Periodic noninvasive vascular imaging (duplex ultrasound, ABI / TBI) to detect recurrence or restenosis
-
In coronary settings, functional testing or stress imaging may be repeated if symptoms recur
-
Evaluate and manage any new or worsening symptoms (e.g. claudication, leg pain, chest pain) early
-
In PAD, supervised exercise or walking programs help improve functional capacity and vascular health
Ongoing Risk Factor & Lifestyle Management
-
Continue or initiate antiplatelet therapy (usually aspirin ± P2Y12 inhibitor) per protocol
-
Maintain statin / lipid-lowering therapy
-
Control blood pressure, diabetes, weight
-
Strict smoking cessation
-
Healthy diet and regular exercise
-
Regular monitoring of renal function, lipid profile, glucose etc.
-
Encourage patient adherence and education, since the intervention is only part of treatment
Quality of Life, Expectations & Limitations
-
Patients should understand that atherectomy addresses a specific segment of disease—it does not cure systemic atherosclerosis
-
Long-term outcomes depend heavily on medical therapy and lifestyle adherence
-
Symptom relief and improved mobility are commonly achieved, though sometimes gradual
-
Some patients might need repeat interventions over time
-
For PAD patients, walking capacity and functional status often improve, but may not return to normal baseline if disease is extensive
-
Psychological support might be beneficial—fear of recurrence, anxiety about further interventions are common
Redo Interventions & Future Options
-
If restenosis or new lesion develops, options include repeat atherectomy, balloon angioplasty, drug-coated balloon, stent placement, or even surgical bypass
-
Preservation of downstream vessels and avoidance of excessive vessel trauma are essential to retain future treatment options
-
In many centers, operators now consider combining atherectomy with intravascular lithotripsy, drug-coated balloons, or scoring balloons to optimize results while minimizing trauma
As one recent roundtable discussion noted, in the field of PAD management, atherectomy remains an important tool to reduce plaque burden and preserve options rather than being the endpoint itself.
Top 10 Frequently Asked Questions about Atherectomy
1. What is an Atherectomy?
An atherectomy is a minimally invasive endovascular
procedure used to remove fatty deposits (plaque) that have built up inside
arteries, restricting blood flow.
It involves using a catheter with a cutting or grinding device to
shave, vaporize, or remove plaque from artery walls.
The goal is to restore normal blood circulation, relieve symptoms such
as leg pain or chest pain, and prevent serious complications like heart attack, stroke,
or limb amputation.
Atherectomy is often performed as an alternative or complement to angioplasty
and stenting.
2. Why is Atherectomy performed?
Atherectomy is performed to treat narrowed or blocked arteries caused by atherosclerosis — a condition where plaque builds up inside the arteries.
Common reasons for performing an atherectomy include:
-
Peripheral Artery Disease (PAD) - reduced blood flow to the legs.
-
Coronary Artery Disease (CAD) - plaque in the arteries supplying the heart.
-
Carotid Artery Disease - narrowing of neck arteries that supply the brain.
-
Recurrent blockages after angioplasty or stent placement.
It’s particularly beneficial when calcified or hard plaque makes angioplasty less effective.
3. What are the different types of Atherectomy procedures?
There are several types of atherectomy devices, each designed for specific kinds of blockages:
-
Directional Atherectomy: Uses a rotating blade to shave plaque from the artery wall.
-
Rotational Atherectomy: A diamond-tipped burr grinds plaque into microscopic particles.
-
Orbital Atherectomy: A spinning crown sands away plaque and widens the vessel gradually.
-
Laser Atherectomy: A laser vaporizes plaque into gas and small particles.
Your doctor will choose the most suitable method depending on artery location, plaque type, and severity of blockage.
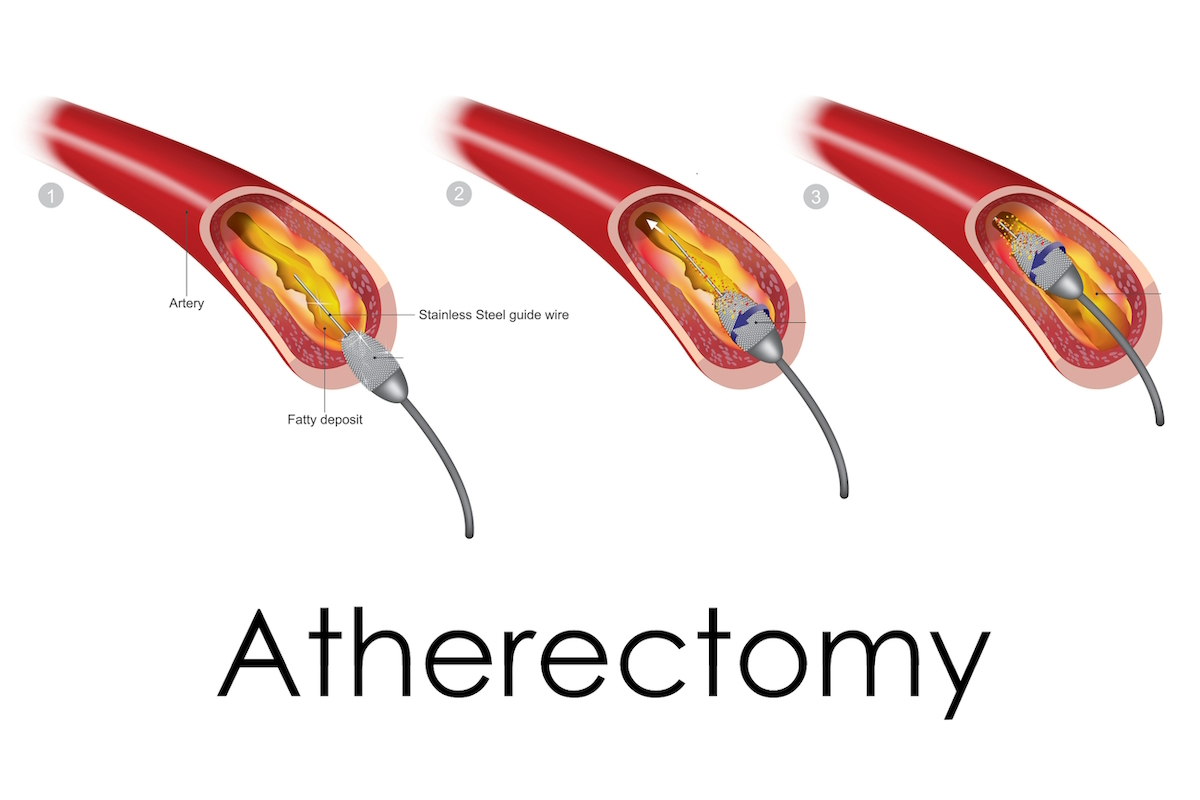
4. How is an Atherectomy performed?
Atherectomy is performed in a catheterization lab under local anesthesia and mild sedation.
Procedure steps:
-
A small incision is made, usually in the groin or wrist.
-
A catheter is guided through the blood vessels to the site of the blockage using X-ray imaging.
-
The atherectomy device is activated to remove the plaque.
-
In some cases, angioplasty or stenting follows to keep the artery open.
-
The catheter is removed, and the incision is closed.
The entire procedure usually takes 1-2 hours, and most patients go home the same day or after one night of observation.
5. Who is a good candidate for Atherectomy?
You may be a candidate for atherectomy if you:
-
Have peripheral or coronary artery disease causing reduced blood flow.
-
Experience leg pain, numbness, or ulcers due to PAD.
-
Have hard or calcified plaque that’s difficult to treat with angioplasty.
-
Previously had stent or angioplasty failure.
A vascular specialist will determine suitability through diagnostic tests like angiography, ultrasound, or CT scan.
6. What are the advantages of Atherectomy compared to other procedures?
Atherectomy offers several distinct benefits:
-
Removes plaque directly instead of merely compressing it.
-
Improves blood flow and reduces symptoms such as pain and fatigue.
-
Preserves arterial flexibility, minimizing trauma to the vessel wall.
-
Reduces the need for stents in some cases.
-
Faster recovery and minimal scarring due to its minimally invasive nature.
It’s particularly effective for calcified or eccentric blockages that are hard to treat using angioplasty alone.
7. What are the risks or complications of Atherectomy?
Although generally safe, atherectomy carries some potential risks, such as:
-
Bleeding or infection at the catheter site.
-
Artery damage or perforation.
-
Embolization (plaque particles traveling downstream and blocking smaller vessels).
-
Re-narrowing of the artery (restenosis) over time.
-
Allergic reaction to contrast dye.
Choosing an experienced vascular surgeon and following postoperative care instructions helps reduce these risks significantly.
8. What happens after the procedure?
After atherectomy, you’ll be monitored for a few hours or overnight in the hospital.
Postoperative care includes:
-
Lying flat for several hours to prevent bleeding from the puncture site.
-
Monitoring vital signs and blood circulation.
-
Drinking plenty of fluids to flush out the contrast dye.
-
Taking prescribed blood-thinning medications to prevent clot formation.
Most patients can resume normal activities within 2-3 days, depending on their condition and overall health.
9. How successful is Atherectomy in restoring blood flow?
Atherectomy has a success rate of 85-95% in improving blood flow and
relieving symptoms.
It’s especially effective in treating calcified and complex arterial
blockages that may not respond well to angioplasty.
However, maintaining long-term results requires lifestyle modifications such as:
-
Quitting smoking
-
Controlling cholesterol and blood sugar
-
Maintaining a healthy weight
-
Regular exercise
These steps reduce the chance of plaque buildup recurring.
10. Is Atherectomy covered by insurance?
Yes, most health insurance providers and government health schemes cover
atherectomy when it’s medically necessary for treating arterial
blockages.
Coverage typically includes:
-
Hospital and procedural costs
-
Surgeon’s fees
-
Device or catheter expenses
It’s advisable to confirm your coverage, co-payment, and any preauthorization requirements with your insurance company and hospital before scheduling the procedure.


