Introduction to AV Canal Repair
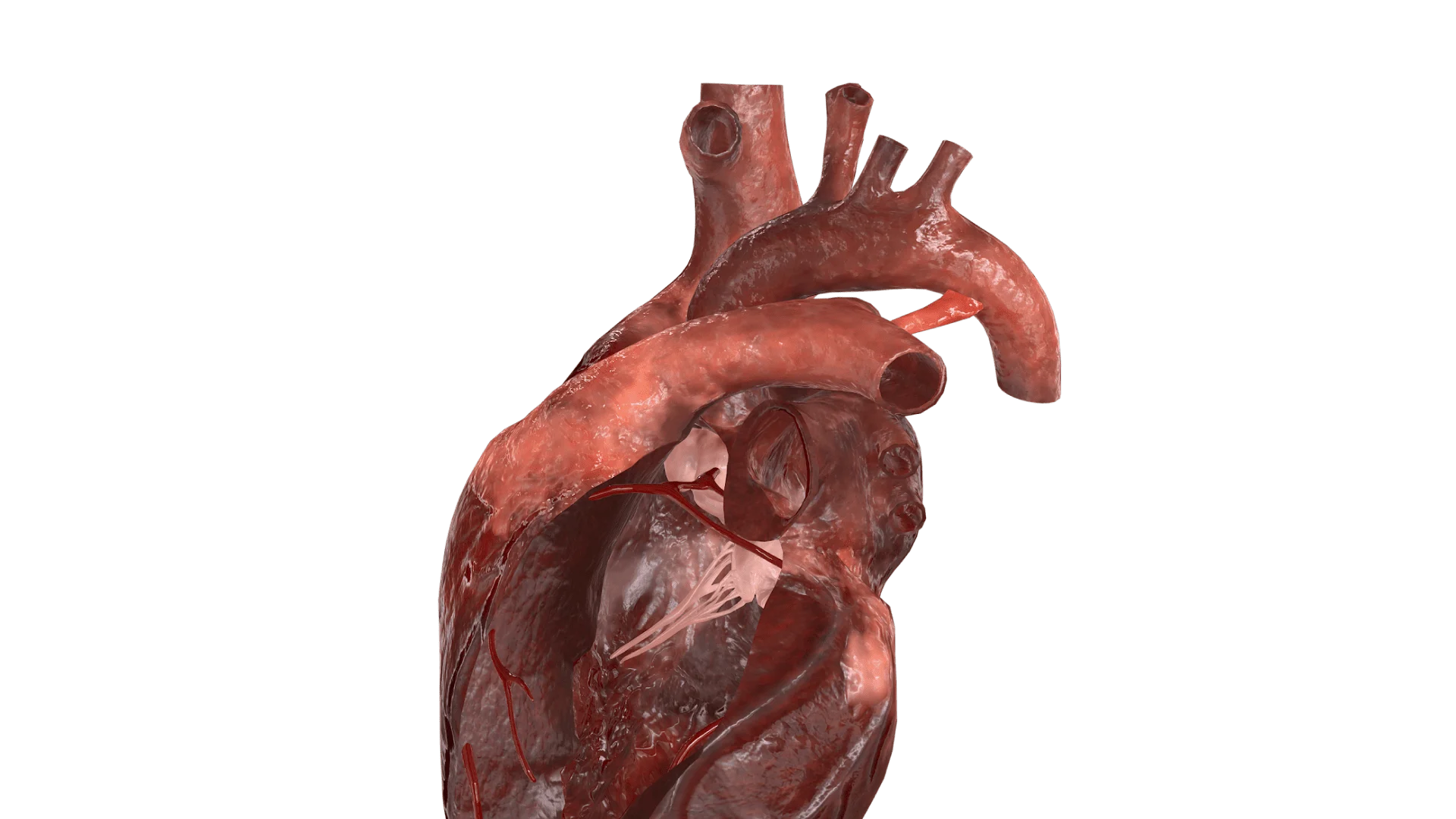
The term atrioventricular (AV) canal defect (also known as an atrioventricular septal defect, AVSD) describes a congenital (present at birth) heart abnormality in which there is a combination of defects affecting the walls (septa) that separate the heart chambers and the atrioventricular valves (the valves between the atria and ventricles).
In simple terms: the centre of the heart-where the upper (atria) and lower
(ventricles) chambers meet and where the mitral and tricuspid valves should
be-is malformed. This leads to abnormal blood flow, mixing of oxygen-rich and
oxygen-poor blood, increased workload on the heart and lungs, and if untreated,
can lead to serious complications.
"AV canal repair" refers to the surgical correction of this defect: closing the
septal holes, reconstructing the valves (or replacing them), and restoring the
normal four-chamber, two-valve anatomy so that the heart can function
effectively with minimal abnormal shunting of blood.
The outlook for patients has improved dramatically over the past decades: modern
surgical techniques provide excellent survival and functional outcomes when done
timely, although lifelong follow-up is still required.
In this blog post we will explore the causes and risks, symptoms, diagnosis,
treatment options (including the repair surgery), prevention/management,
complications, and what life is like living with this condition after repair.
Causes and Risk of AV Canal Defect (leading to Repair)
How and when it develops
During fetal development, the heart transitions from a simple tube into a
four-chamber organ with distinct atria, ventricles, and valves. Part of this
process is formation and fusion of the endocardial cushions around weeks 4-5 of
gestation, which contribute to the atrial septum, the ventricular septum and the
atrioventricular (AV) valves.
In AV canal defects, the cushions fail to fuse or the septa fail to grow
properly, leading to a spectrum of anomalies: an atrial septal defect (ASD) in
the lowest part of the atrial septum ("ostium primum" type), often a ventricular
septal defect (VSD), and abnormal AV valves (either one common valve instead of
mitral + tricuspid, or two but with cleft leaflets or leaks).
Risk factors
While the exact cause remains unknown in many cases, several risk factors have been shown or suspected:
-
Genetic/chromosomal associations: especially Down syndrome (Trisomy 21) - infants with Down syndrome have a much higher incidence of AV canal defects.
-
Maternal conditions: poorly controlled diabetes (pre-gestational) and maternal obesity have been associated with increased risk of non-syndromic AV canal defects.
-
Maternal infections/exposures: for instance maternal rubella (German measles) infection during early pregnancy has been implicated in congenital heart defects including AV canal.
-
Maternal alcohol use, smoking or certain medications during pregnancy may slightly increase risk of congenital heart defects (including but not exclusively AV canal).
Magnitude / incidence
AV canal defects account for about 3-5% of all congenital heart disease (CHD). In the U.S., about 1 in 1,700 babies are born with AVSD each year.
Why repair is needed
Because the defect disrupts normal blood flow-oxygen-rich and poor blood mix, the heart works harder, extra blood travels to lungs causing pulmonary over-circulation and ultimately may lead to heart failure or irreversible pulmonary vascular disease. Early repair prevents these long-term consequences.
Symptoms and Signs of AV Canal Defect
The spectrum of presentation
Because the anatomical defect can vary in severity (complete vs partial vs transitional), the symptoms likewise vary.
-
Complete AV canal defect: There is a large hole between both atria and ventricles, and one common AV valve. These babies often show symptoms early - within first few weeks of life.
-
Partial / incomplete AV canal defect: The ventricular septum may be intact or small defect, and the AV valve abnormality may be milder. Symptoms may be delayed into infancy or childhood, sometimes even adulthood.
Typical signs/symptoms
In infants with more severe defects:
-
Rapid or laboured breathing (tachypnea, using accessory muscles)
-
Difficulty feeding (tiring during feeds), poor weight gain ("failure to thrive")
-
Sweating (especially with feeding)
-
Bluish or greyish skin colour (cyanosis) or pale skin tone - depending on how much mixing of oxygen-poor blood.
-
Swelling (edema) of legs, ankles or feet, or fluid in the belly (ascites) in more advanced heart failure.
-
A heart murmur or irregular rapid heartbeat may be noted by a clinician.
In milder/partial defects (sometimes later onset): -
Fatigue, reduced exercise tolerance
-
Shortness of breath on exertion
-
Persistent cough or wheezing (especially from lung congestion)
-
Palpitations or arrhythmia (irregular heartbeat)
-
Some may remain asymptomatic for years until valve leakage or pulmonary hypertension develops.
What to look for (for your blog readers)
Highlight for parents/readers: If a baby tires easily, seems to feed poorly,
breathes fast, sweats more than expected, or remains small/underweight despite
feeding, it is wise to ask the paediatrician about a possible cardiac
evaluation.
In older children/adults, unexplained shortness of breath, arrhythmia, or heart
murmurs should lead to cardiology review.
Diagnosis of AV Canal Defect
Initial clinical suspicion
Diagnosis often begins with clinical suspicion: newborn with heart murmur, signs of heart failure, or abnormal findings on prenatal ultrasound. Some centres screen fetuses with echocardiography if risk factors (e.g., Down syndrome) are present.
Key investigations
-
Echocardiogram (echo): The gold standard for diagnosis. It shows the anatomy of the septal defects (ASD, VSD), the AV valves (how many leaflets, whether there is a 'common' valve), chamber sizes, blood flow direction (shunts) and valve leaks.
-
Electrocardiogram (ECG/EKG): To check for arrhythmias or signs of chamber enlargement.
-
Chest X-ray: May show enlarged heart, increased lung blood flow (pulmonary congestion).
-
Cardiac catheterisation / MRI: In some cases to delineate anatomy, measure pressures (especially if pulmonary hypertension suspected) or assess suitability for surgery.
Prenatal diagnosis
With high-resolution obstetric ultrasound (fetal echo), some AV canal defects are detected before birth. When detected, delivery planning at a tertiary centre with paediatric cardiology/cardiac surgery is advisable.
Timing of diagnosis & its importance
Early diagnosis is critical because the longer the abnormal flow persists (especially large left-to-right shunt), the greater risk of irreversible damage (to lungs, to the heart). Once diagnosed, planning for repair (surgery) should not be unduly delayed.
Treatment Options for AV Canal Defect (AV Canal Repair)
Medical management (pre-operative support)
In many infants who are symptomatic (high shunt, heart failure), initial medical therapy is required to stabilize before surgery:
-
Diuretics (reduce fluid overload)
-
Digoxin or other heart-failure medications as applicable
-
Nutritional support (calorie-rich feeds, possibly tube feeding) to enable growth and strength before surgery.
Surgical repair - the mainstay
For most patients with AV canal defect (especially the complete form), surgical
correction is the treatment of choice.
Key elements:
-
Closure of septal defects (patching the ASD and VSD, or single patch depending on the technique)
-
Reconstruction or repair of the AV valves (mitral and tricuspid), or creation of two separate valves if there is a single common valve.
-
The surgery is open-heart, under cardiopulmonary bypass (pump), usually via sternotomy.
Timing of surgery
-
For very large defects (complete AV canal) with early heart failure: surgery is often done in the first 3-6 months of life.
-
For partial defects or milder cases: surgery may be scheduled at a slightly older age, but before long-term damage to lungs or valves sets in.
Surgical techniques
-
There are different surgical techniques: single-patch, double-patch, modified single-patch. Studies show good outcomes with modern approaches.
-
Surgeons also pay attention to reconstruction of valve leaflets to minimise post-operative valve leak (regurgitation) and avoid left ventricular outflow tract (LVOT) obstruction.
Post-operative care & follow up
-
After surgery, patients require ICU care, monitoring for rhythm disturbances, valve function, residual leaks, infection, fluid balance, etc.
-
Long-term follow up by a congenital heart disease specialist is needed: lifelong monitoring of valve function, ventricular function, rhythm, and pulmonary pressures.
Outcome / prognosis
-
Modern surgical repair results are excellent: for instance, a 2023 study of a single-patch technique found no in-hospital mortality and very good short to mid-term results.
-
A large long-term study found that early repair of complete AVSD can lead to excellent survival into adulthood.
However, this does not mean "cure" in the sense of no further care - rather "excellent repair" and "much better life expectancy/function".
Special considerations in India / resource-limited settings (you may tailor)
-
Early referral to a paediatric cardiologist/cardiac surgeon is key.
-
Pre-operative optimisation (nutrition, controlling heart failure) may be more challenging.
-
Post-op lifelong follow-up is essential yet may get overlooked; emphasise importance of periodic check-ups, even years after successful surgery.
Prevention and Management of AV Canal Defect
Prevention (primary)
While many congenital heart defects cannot be fully prevented, certain steps can reduce risk or ensure early detection:
-
Pre-conception and antenatal care: optimizing maternal health (control diabetes, manage weight/obesity, avoid alcohol/smoking during pregnancy) reduces risk of many congenital anomalies including AV canal defect.
-
Prenatal screening: High-risk pregnancies (e.g., known chromosomal anomalies, maternal illness) may benefit from detailed fetal echocardiography. Early detection allows planning of delivery, early intervention and improves outcomes.
Management (secondary)
For children/adults who have undergone repair or have unrepaired/mild defect:
-
Lifelong cardiology follow-up: periodic echocardiogram, ECG, assessment of valve/leak, rhythm issues, pulmonary pressure.
-
Exercise and activity: after repair, most children can lead near-normal lives with encouragement to stay active; customised advice from cardiologist is needed.
-
Infection prophylaxis: In some cases, patients may need prophylaxis for infective endocarditis (depending on residual valve lesions) - to be guided by cardiologist.
-
Healthy lifestyle: Maintaining normal blood pressure, avoiding obesity, smoking, staying physically active, eating heart-healthy diet will support long-term heart health.
-
Monitoring for late complications: Even after successful repair, there is risk of valve regurgitation, arrhythmia, need for re-intervention; timely recognition improves outcomes.
Patient / Parent education
-
Explain clearly what repair does and what it does not do (e.g., anatomy may be improved but lifelong monitoring is needed).
-
Encourage adherence to follow-up schedules, medication compliance, prompt reporting of symptoms (e.g., palpitations, breathlessness, swelling).
-
Support growth and development (in infants: ensure good nutrition; monitor for developmental delays which may accompany syndromic forms like Down syndrome).
Planning for adulthood
As more children with congenital heart disease survive into adulthood, ensure transition from paediatric to adult congenital heart clinics. Issues such as pregnancy, fitness, employment, insurance need guidance.
Complications of AV Canal Defect / Repair
If untreated
-
Progressive heart failure (due to volume overload)
-
Pulmonary hypertension (high pressure in lung vessels) which can become irreversible (Eisenmenger-type physiology) if the shunt persists.
-
Arrhythmias (abnormal heart rhythms)
-
Increased risk of infections (especially respiratory infections).
After surgical repair
Even after successful repair, there are potential long-term complications to be aware of:
-
Residual or recurrent AV valve (especially left AV valve / mitral) regurgitation (leak). Many studies note that left AV valve regurgitation is one of the common causes of re-intervention.
-
Stenosis (narrowing) of the repaired AV valve or left ventricular outflow tract (LVOT obstruction) may develop later.
-
Rhythm disturbances: conduction blocks, arrhythmias requiring pacemaker in some cases.
-
Residual septal defects or shunts, residual leaks, or patch-related complications.
-
Late heart failure, even in repaired patients, especially if valve regurgitation or pulmonary hypertension persists.
-
In adulthood: problems with pregnancy (in females), exercise limitation (in some), endocarditis risk in some cases.
Key takeaway for your blog
It's important to emphasise that while repair dramatically improves outlook, it is not a one-time cure requiring no further attention. Patients and families must stay vigilant, attend follow-ups, and manage heart health proactively.
Living with the Condition After AV Canal Repair
Quality of life and outlook
Thanks to advances in surgical technique, most children who undergo timely AV canal repair go on to lead active, healthy lives. Studies show very high survival into adolescence and adulthood with good functional status.
Follow-up care
-
Regular check-ups at a congenital heart disease centre (or paediatric/adult cardiologist) - periodic echo, ECG, possibly exercise testing.
-
Medication if needed (for heart rhythm, valve leak, heart failure).
-
Monitoring valve function, any residual or new leak, rhythm issues, and lung pressures.
-
Lifestyle: Encouraging near-normal physical activity is generally allowed; however, any restrictions or guidance must come from the specialist.
-
Growth, nutrition and development: Especially in infants with syndromic associations (e.g., Down syndrome) vigilance for associated health/developmental issues is important.
Education & psychosocial support
-
Helping families understand the condition, surgery, what to watch for, how to support children's growth and activity.
-
In adulthood: transition to adult congenital heart disease services, fertility/pregnancy counselling (especially for women), employment/insurance plan\
When to seek medical attention
Advise patients/parents to contact their cardiologist if they notice:
-
New or worsening shortness of breath, fatigue
-
Palpitations or irregular heartbeats
-
Swelling of legs/ankles or abdomen
-
Change in exercise tolerance
-
Fever, signs of infection (especially if valve prosthesis or residual lesions)
Pregnancy considerations
Women who had AV canal repair and are in good condition can often have successful pregnancies, but planning is essential: consultation with an adult congenital cardiologist is advised. If there were significant valve issues or residual lesions, pregnancy may carry increased risk.
Top 10 Frequently Asked Questions about Acupressure
1. What is an Atrioventricular (AV) Canal Defect?
An AV Canal defect, also known as an Atrioventricular Septal Defect (AVSD) or Endocardial Cushion Defect, is a congenital heart condition where there is a hole in the center of the heart affecting all four chambers. This defect leads to a large hole between the atria and ventricles and a common valve instead of the normal mitral and tricuspid valves. It results in abnormal blood flow between the heart chambers and increased blood flow to the lungs.
2. What are the types of AV Canal Defects?
There are three main types:
-
Complete AV Canal Defect: Involves a large hole between all four chambers and a single valve.
-
Partial AV Canal Defect: Involves a hole between the atria or ventricles and an abnormal valve.
-
Transitional AV Canal Defect: A combination of partial and complete defects.
3. What are the symptoms of an AV Canal Defect?
Symptoms can vary based on the size of the defect and the amount of blood flowing to the lungs. Common symptoms include:
-
Rapid breathing
-
Difficulty feeding
-
Poor weight gain
-
Sweating
-
Cyanosis (bluish skin color)
-
Heart murmur
4. How is an AV Canal Defect diagnosed?
Diagnosis typically involves:
-
Echocardiogram: Ultrasound imaging to visualize heart structure and blood flow.
-
Electrocardiogram (ECG/EKG): Measures electrical activity of the heart.
-
Chest X-ray: Assesses heart size and lung condition.
-
Cardiac MRI or CT scan: Provides detailed images of heart anatomy.
-
Cardiac catheterization: Measures pressures within the heart chambers.
5. What is the treatment for an AV Canal Defect?
Surgical repair is the primary treatment. The procedure involves:
-
Closing the hole between the heart chambers using patches.
-
Separating the common valve into two distinct valves (mitral and tricuspid).
-
Repairing any associated valve abnormalities.
Surgery is typically performed within the first few months of life, especially for complete AV Canal defects.
6. What is the prognosis after surgery?
With successful surgery, many children lead healthy lives. The long-term outlook is generally good, but regular follow-up with a pediatric cardiologist is essential to monitor heart function and detect any complications early.
7. Are there any risks or complications associated with AV Canal Repair?
Potential risks include:
-
Valve leakage (regurgitation)
-
Arrhythmias (abnormal heart rhythms)
-
Pulmonary hypertension
-
Need for additional surgeries in the future
However, advancements in surgical techniques have significantly reduced these risks.
8. What is the recovery process like after surgery?
Post-surgery recovery involves:
-
Hospital stay of 5-7 days, depending on the child's condition.
-
Gradual reintroduction to feeding and physical activities.
-
Regular follow-up visits to monitor heart health.
Most children recover well and resume normal activities with time.
9. Can AV Canal Defects be prevented?
Most AV Canal defects occur due to genetic factors and cannot be prevented. However, maintaining a healthy pregnancy by avoiding alcohol, tobacco, and certain medications, and managing chronic conditions like diabetes, can reduce the risk of congenital heart defects.
10. What follow-up care is needed after AV Canal Repair?
Lifelong follow-up care is crucial and may include:
-
Regular echocardiograms to assess heart function.
-
Monitoring for any signs of valve issues or arrhythmias.
-
Consultation with an adult congenital heart disease specialist as the child grows.
Early detection of any problems can lead to more effective management and improved outcomes.


