Introduction to Balloon Atrial Septostomy
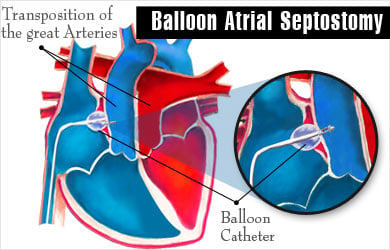
Balloon Atrial Septostomy (BAS) is a specialized cardiac catheterization procedure used to create or enlarge a hole (called an atrial septal defect) between the upper chambers of the heart — the right atrium and left atrium. This is done to improve oxygenated blood flow in newborns and infants who are born with certain types of congenital heart defects (CHDs), particularly those that restrict normal circulation of oxygen-rich blood.
The procedure was first introduced by Dr. William Rashkind and Dr. William Miller in 1966, marking a breakthrough in neonatal cardiac care. It remains one of the essential palliative interventions for conditions such as Transposition of the Great Arteries (TGA), where the pulmonary and systemic circulations are improperly connected.
The goal of Balloon Atrial Septostomy is not to cure the underlying defect but to temporarily stabilize the infant by improving oxygen saturation until a definitive corrective surgery can be performed. Advances in imaging, catheter design, and interventional cardiology techniques have significantly improved the safety and success rate of this life-saving procedure.
Causes and Risk Factors Related to Balloon Atrial Septostomy
Causes or Indications for the Procedure
Balloon Atrial Septostomy is primarily indicated in cyanotic congenital heart diseases where there is a need to mix oxygen-rich and oxygen-poor blood to maintain adequate oxygen levels in the body. The most common conditions requiring BAS include:
-
Transposition of the Great Arteries (TGA): The most frequent indication for BAS. In TGA, the two main arteries leaving the heart are switched, causing blood to circulate improperly between the lungs and the body.
-
Tricuspid Atresia: Absence of the tricuspid valve prevents blood flow from the right atrium to the right ventricle.
-
Pulmonary Atresia: Blockage of blood flow from the right ventricle to the lungs.
-
Total Anomalous Pulmonary Venous Return (TAPVR): Pulmonary veins connect abnormally to the right atrium instead of the left.
-
Hypoplastic Left Heart Syndrome (HLHS): Underdevelopment of the left side of the heart.
In all these conditions, a septostomy helps ensure better oxygen mixing between the two atria until surgical correction.
Risk Factors for Performing BAS
While the procedure itself is generally safe, certain factors increase the risk of complications or failure:
-
Very small or thickened atrial septum.
-
Premature infants with low body weight.
-
Presence of associated cardiac anomalies.
-
Pre-existing infections or sepsis.
-
Inadequate imaging guidance.
-
Poor systemic oxygenation before the procedure.
Modern advancements, such as echocardiographic guidance and improved catheter materials, have significantly reduced these procedural risks.
Symptoms and Signs Necessitating Balloon Atrial Septostomy
Infants who require a Balloon Atrial Septostomy often present with severe cyanosis (bluish discoloration of the skin, lips, and nails) within hours or days after birth due to insufficient oxygen in the bloodstream.
Common Symptoms Include:
-
Bluish coloration of lips, tongue, and fingertips (central cyanosis).
-
Rapid or labored breathing (respiratory distress).
-
Poor feeding and lethargy.
-
Low oxygen saturation despite oxygen therapy.
-
Cold extremities and weak pulse.
-
Episodes of fainting or collapse in severe cases.
Clinical Findings:
-
Heart murmur or abnormal heart sounds.
-
Low oxygen levels on pulse oximetry.
-
Poor growth and development if left untreated.
-
Evidence of heart enlargement or abnormal circulation patterns on imaging.
When such symptoms are identified, urgent evaluation and intervention such as BAS may be required to stabilize the infant.
Diagnosis of Conditions Requiring Balloon Atrial Septostomy
Diagnosis begins with a detailed clinical examination followed by imaging studies to confirm the type and severity of the congenital heart defect.
Diagnostic Procedures Include:
-
Echocardiography (ECHO):
-
The primary diagnostic tool used to visualize the structure and function of the heart.
-
It identifies the presence of septal defects, direction of blood flow, and oxygen mixing efficiency.
-
Real-time echocardiographic guidance is also used during the BAS procedure.
-
-
Pulse Oximetry:
-
Measures oxygen saturation levels in the blood.
-
Persistent low oxygen saturation despite oxygen therapy raises suspicion for TGA or similar defects.
-
-
Chest X-ray:
-
Helps identify the size and shape of the heart and any pulmonary vascular congestion.
-
-
Cardiac Catheterization:
-
A more detailed invasive study that confirms diagnosis and allows for immediate treatment, including BAS.
-
-
MRI or CT Angiography (in older infants or children):
-
Provides 3D visualization of cardiac anatomy when complex defects are suspected.
-
Early and accurate diagnosis is crucial, as timely septostomy can prevent hypoxic brain injury, organ damage, and death.
Treatment Options – Balloon Atrial Septostomy Procedure
Overview of the Procedure
Balloon Atrial Septostomy is a minimally invasive cardiac catheterization technique typically performed in a neonatal intensive care or cardiac catheterization lab.
Step-by-Step Procedure:
-
The baby is sedated or given general anesthesia to prevent movement and pain.
-
A thin catheter with a small balloon at its tip is inserted, usually through the umbilical vein or femoral vein, and advanced into the right atrium.
-
Under echocardiographic and fluoroscopic guidance, the catheter crosses the atrial septum into the left atrium.
-
The balloon is inflated and pulled back abruptly into the right atrium, tearing the septum and creating a larger opening.
-
The balloon is then deflated and withdrawn.
-
The baby’s oxygen levels are closely monitored; the improvement in oxygen saturation confirms the success of the procedure.
Alternative or Supportive Treatments:
-
Prostaglandin E1 Infusion: Keeps the ductus arteriosus open to improve oxygenation temporarily.
-
Surgical Atrial Septostomy: May be performed if BAS is unsuccessful or the septum is too thick.
-
Definitive Cardiac Surgery: Once the infant is stabilized, corrective surgery (like an arterial switch operation for TGA) is planned.
Post-Procedure Care:
-
Continuous cardiac and oxygen monitoring.
-
Echocardiography to assess septal opening.
-
Intravenous fluids, antibiotics, and supportive care.
-
Gradual transition to definitive surgical repair.
Prevention and Management Related to Balloon Atrial Septostomy
Since Balloon Atrial Septostomy is primarily a treatment for congenital heart defects rather than a preventable condition, prevention efforts focus on reducing the risk of congenital heart diseases and ensuring early detection.
Preventive Measures:
-
Prenatal screening: Fetal echocardiography can detect congenital heart defects during pregnancy.
-
Maternal health management: Control of diabetes, infections, and avoidance of teratogenic drugs during pregnancy.
-
Genetic counseling: For families with a history of congenital heart disease.
-
Newborn screening: Routine oxygen saturation checks immediately after birth can detect cyanotic defects early.
Management Strategies:
-
Early stabilization and immediate transfer to a cardiac care center.
-
Ongoing cardiology follow-up to plan further surgeries.
-
Use of oxygen therapy, medications, and nutrition support for recovery.
-
Long-term developmental monitoring to ensure normal growth milestones.
Complications of Balloon Atrial Septostomy
Though BAS is generally safe, complications can occasionally occur, especially in very small or critically ill infants.
Possible Complications Include:
-
Cardiac perforation or tamponade (fluid around the heart).
-
Arrhythmias (irregular heartbeats).
-
Bleeding or vascular injury at the catheter site.
-
Embolism (clot dislodgment).
-
Residual septal defect that is too large or too small.
-
Infection or sepsis.
-
Stroke or neurologic complications (rare).
Most of these complications can be minimized with expert hands, advanced imaging guidance, and appropriate postoperative care.
Living with the Condition after Balloon Atrial Septostomy
Children who undergo BAS usually require lifelong follow-up with a pediatric cardiologist, especially if they have complex congenital heart disease.
Long-Term Outlook:
-
BAS itself is a temporary or palliative procedure. The child will likely need corrective surgery (e.g., arterial switch or Glenn procedure) later.
-
With modern surgical advances, the long-term survival and quality of life of these children have improved dramatically.
-
Growth, development, and physical activity can be nearly normal after complete repair.
Lifestyle and Follow-Up:
-
Regular cardiac checkups and echocardiograms.
-
Monitoring for any signs of recurrent cyanosis, fatigue, or growth delays.
-
Proper nutrition and vaccination.
-
Avoidance of infections, especially respiratory infections, which can strain the heart.
-
Support from family and counseling services to help cope with the condition emotionally.
Top 10 Frequently Asked Questions about Balloon Atrial Septostomy
1. What is Balloon Atrial Septostomy?
Balloon Atrial Septostomy (BAS) is a minimally invasive cardiac procedure that creates or enlarges an opening (called a septal defect) between the right and left atria — the upper chambers of the heart.
This hole allows oxygen-rich and oxygen-poor blood to mix, which improves the amount of oxygen delivered to the body.
The procedure is most often performed in newborns with congenital heart defects, such as Transposition of the Great Arteries (TGA), where normal blood flow is disrupted.
2. Why is Balloon Atrial Septostomy performed?
BAS is performed to improve oxygen levels in the blood and relieve pressure in the right side of the heart.
It is typically done in babies born with certain cyanotic (blue baby) congenital heart defects, such as:
-
Transposition of the Great Arteries (TGA)
-
Tricuspid Atresia
-
Total Anomalous Pulmonary Venous Return (TAPVR)
-
Pulmonary Atresia or Stenosis
By creating or enlarging the atrial opening, BAS allows for better blood mixing, which helps stabilize the child until corrective heart surgery can be performed.
3. How is Balloon Atrial Septostomy performed?
BAS is performed in a cardiac catheterization laboratory under general anesthesia (for infants) or sedation and local anesthesia (for older children or adults).
Procedure steps:
-
A thin, flexible catheter with a deflated balloon at its tip is inserted through a vein (usually in the groin) and guided into the right atrium of the heart.
-
The catheter is advanced through the foramen ovale (a natural opening between the atria) into the left atrium.
-
The balloon is inflated and pulled back into the right atrium, stretching or tearing the septum to create a larger opening.
-
The catheter and balloon are then removed.
The entire procedure typically takes 30–60 minutes, and results are often seen immediately through improved oxygen levels.
4. Who needs a Balloon Atrial Septostomy?
Balloon Atrial Septostomy is usually performed on:
-
Newborns with cyanotic heart defects who appear blue due to low oxygen levels.
-
Infants with restricted blood flow between atria, detected through echocardiography.
-
Patients awaiting open-heart surgery, as a temporary measure to stabilize oxygenation.
It may also be performed in adults with pulmonary hypertension or other heart conditions where controlled shunting is beneficial.
5. What are the benefits of Balloon Atrial Septostomy?
The main benefits of BAS include:
-
Improved oxygenation throughout the body.
-
Relief of right heart pressure, allowing more efficient heart function.
-
Immediate improvement in cyanosis (blue discoloration).
-
Bridge to definitive surgical repair for congenital heart defects.
-
Life-saving intervention in newborns with critical cardiac malformations.
For many babies, this procedure is the first and most essential step toward survival and future corrective surgery.
6. What are the risks or complications of the procedure?
Balloon Atrial Septostomy is generally considered safe, especially when performed by experienced pediatric cardiologists. However, potential risks include:
-
Bleeding or bruising at the catheter insertion site.
-
Arrhythmias (irregular heartbeats) during or after the procedure.
-
Perforation of the heart wall (very rare).
-
Blood clots or stroke (extremely rare).
-
Infection at the catheter site.
-
Low blood pressure or oxygen fluctuations during the procedure.
Most complications are rare and manageable with proper monitoring and care.
7. How long is the recovery period after Balloon Atrial Septostomy?
Recovery time after BAS is usually short:
-
Babies are typically monitored in the neonatal intensive care unit (NICU) for 24–48 hours.
-
Continuous oxygen and heart rate monitoring are performed.
-
Feeding and activity return to normal within a few days if oxygen levels stabilize.
Most patients are discharged once oxygen saturation remains stable and no complications are observed. BAS often provides temporary relief until definitive surgical correction is performed within weeks or months.
8. How successful is Balloon Atrial Septostomy?
The success rate of BAS is over 95%, especially in newborns with Transposition of the Great Arteries (TGA).
Immediate benefits include:
-
Improved blood oxygen levels.
-
Stabilized heart function.
-
Reduced cyanosis and better feeding and growth in infants.
BAS often buys critical time before more complex surgeries, such as the Arterial Switch Operation or Rashkind procedure, are performed.
9. How long does the created opening last?
The opening created by Balloon Atrial Septostomy may remain open for several weeks or months. However, over time, the hole can narrow or close naturally as tissue heals.
In some cases, a stent may be inserted during the procedure to maintain patency (keep the hole open) until definitive corrective surgery.
Regular follow-up with echocardiography ensures that the atrial opening remains functional until no longer needed.
10. Is Balloon Atrial Septostomy covered by insurance?
Yes. Most health insurance companies and government health schemes cover Balloon Atrial Septostomy when performed for congenital or life-threatening heart defects.
Coverage generally includes:
-
Hospital and cardiac catheterization lab charges.
-
Pediatric cardiologist and anesthetist fees.
-
Equipment and catheter costs.
-
Postoperative monitoring and care.
Families are encouraged to check specific coverage details and preauthorization requirements with their insurance provider and hospital before admission.


