Introduction to Bartholin's Gland Marsupialisation
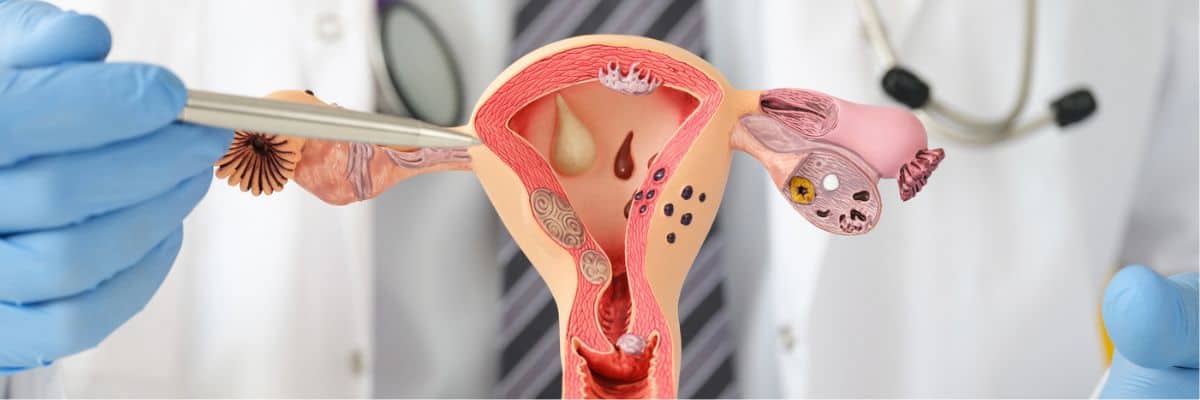
The Bartholin's glands are paired small glands located at the 4 and 8 o'clock positions of the vaginal vestibule. Their role is to secrete mucus for vaginal lubrication, particularly during sexual arousal. When the duct of one of the Bartholin glands becomes obstructed - for example due to infection, trauma or blockage of drainage - a fluid-filled cyst may develop. If that cyst becomes infected, an abscess can form.
Marsupialisation is a surgical procedure designed to treat symptomatic Bartholin's gland cysts or abscesses by creating a permanent drainage tract. In this procedure, the surgeon makes an incision in the cyst/abscess, drains its contents, and then sutures the remaining cyst wall to the surrounding mucosa, thereby forming a pouch (or "marsupialised" opening) that allows continuous drainage and reduces the chance of re-accumulation.
This treatment is typically recommended for recurrent cysts/abscesses, for those causing significant discomfort, or when simpler office-based treatments (for example catheter drainage) are not appropriate or have failed.
In this blog we will explore the causes and risks, symptoms, diagnosis, full range of treatment options including marsupialisation, how to prevent/manage the condition, possible complications, and what living with the condition looks like.
Causes and Risk of Bartholin's Gland Marsupialisation
Strictly speaking, we don't treat "Bartholin's gland marsupialisation" as a disease - the condition is a Bartholin gland cyst or abscess, and the marsupialisation is the treatment. So here we interpret this heading to mean "causes and risk factors of Bartholin's gland cyst/abscess (which may lead to marsupialisation)".
Causes / Pathophysiology
-
Obstruction of the Bartholin duct leads to accumulation of glandular secretions and formation of a cyst. This obstruction may be due to trauma, local irritation, infection, or (less commonly) a mucus plug.
-
If the fluid becomes infected (by typical skin flora, or in some cases sexually transmitted organisms), the cyst can turn into an abscess (a pus-filled cavity) causing pain, swelling, redness.
Risk Factors
-
Age: most common in women of reproductive age (typically 20s-40s).
-
Sexual activity: multiple sexual partners or history of sexually transmitted infection may increase risk of duct obstruction/infection.
-
Prior vulvar trauma or surgery (for example episiotomy, vulvar surgery) may predispose to duct damage or obstruction.
-
History of previous Bartholin gland cyst/abscess: recurrence risk is elevated.
-
Possibly immunosuppression or poor local hygiene may play a role (though direct strong data is limited).
-
Women over 40: while cysts are still possible, any new vulvar mass in older women should raise concern for malignancy (i.e., risk of overlooked vulvar cancer) and should therefore be evaluated carefully.
Why the Procedure May Be Needed
Because the cyst/abscess may keep recurring if simply drained, and because the obstruction persists, marsupialisation is performed to create a more permanent drainage pathway and reduce recurrence. As an overview: frequent recurrence, symptomatic discomfort (pain sitting, walking, sexual intercourse) and patient preference may prompt the procedure.
Symptoms and Signs of Bartholin's Gland Cyst/Abscess (and Indication for Marsupialisation)
A Bartholin's gland cyst or abscess develops when the duct of a Bartholin gland near the vaginal opening becomes blocked, leading to fluid accumulation or infection. The symptoms and clinical signs depend on whether the swelling is a simple cyst or an abscess.
Symptoms
-
A swelling or lump at one side of the vaginal opening (labia majora/vestibule) - often pea- to walnut-sized for a cyst, but may enlarge considerably when infected.
-
Pain or discomfort: particularly during walking, sitting, or sexual intercourse (dyspareunia).
-
If abscess develops: increased pain, redness, warmth, sometimes fever or systemic signs of infection.
-
Discharge: if the cyst/abscess drains spontaneously, a foul or purulent discharge may be present.
Signs on Physical Examination
-
Visible or palpable swelling at 4 or 8 o'clock of the introitus (vaginal opening).
-
Tenderness on palpation (especially if abscess).
-
Overlying skin may be erythematous and warm (if infected).
-
Occasionally fluctuance may be felt (if abscess).
-
In recurring cases or in older women: examination may include rule-out of vulvar carcinoma (especially if unusual features: fixed mass, hard areas, ulceration).
When to Consider Marsupialisation
Indications for marsupialisation include:
-
Recurrent cysts/abscesses despite conservative/office treatment.
-
Large symptomatic cysts causing pain, discomfort, interfering with sitting/walking/sexual activity.
-
Abscess that may benefit from surgical management to ensure good drainage and healing.
-
Patient preference for longer-term solution.
Diagnosis of Bartholin's Gland Cyst/Abscess (and Pre-operative Workup)
Diagnosis of a Bartholin's gland cyst or abscess primarily relies on careful clinical evaluation, supported by laboratory testing and selective imaging when indicated. Pre-operative workup is essential before marsupialization or excision to confirm diagnosis, rule out malignancy, and assess surgical readiness.
Clinical Diagnosis
-
Most cases are diagnosed clinically based on history and examination. The characteristic presentation of a unilateral vulvar swelling at the site of the Bartholin gland is strongly suggestive.
-
For simple cysts (asymptomatic) often no further work-up is needed.
Additional Investigations
-
If abscess: may obtain culture of drainage fluid (if indicated) to guide antibiotic therapy (especially if unusual organisms).
-
In recurrent cases or cases in older women (e.g., > 40-45 years), imaging (ultrasound) or biopsy may be considered to exclude underlying malignancy (e.g., Bartholin gland carcinoma) or other vulvar pathology.
-
Pre-operative assessment: Ensure patient is appropriate for surgery (fitness for anaesthesia, local conditions, any bleeding risk, possibility of pregnancy, etc.).
-
In the context of marsupialisation: ensure informed consent - discuss benefits, risks, possibility of recurrence, alternatives (e.g., Word catheter, excision).
Pre-operative Preparation
-
Good vulvar hygiene; treatment of any co-existing infection prior to elective surgery.
-
Patient counselling about post-operative care (pain, sitting difficulty, sexual abstinence for a time).
-
Ensure any antibiotics, analgesics, instructions for sitz baths etc are given.
Treatment Options of Bartholin's Gland Cyst/Abscess (with focus on Marsupialisation)
Treatment of Bartholin's gland cysts and abscesses depends on the size, symptoms, infection status, and recurrence history. The main goal is to relieve pain, drain the cyst or abscess, eradicate infection, and prevent recurrence.
Here we outline the spectrum of treatments, then zoom in on the marsupialisation procedure.
Conservative / Office Treatments
-
Asymptomatic cysts may be observed (no intervention).
-
Sitz baths (warm water soaks) multiple times daily to promote spontaneous drainage and relief of discomfort.
-
Simple incision and drainage (I&D) for abscess formation - often provides rapid relief but has higher recurrence.
-
Placement of a Word catheter (silicone balloon catheter) in the drained cyst/abscess: the balloon keeps duct open and allows epithelialisation of a tract. Good for outpatient management.
-
Other methods reported: silver nitrate application, CO₂ laser-ablation, electrosurgery of capsule, but these are less commonly first-line.
Marsupialisation
-
As described earlier, marsupialisation involves making an incision in the cyst/abscess, evacuating contents, then suturing the cyst wall to the mucosal edge to establish a wide permanent drainage opening.
-
Indications: recurrent cases, large symptomatic cyst or abscess, patient preference, failed previous drainage or catheter treatment.
-
Procedure details: Typically performed under local, regional, or general anaesthesia depending on size/complexity. The incision may be 1.5-3 cm. After drainage, the edges of the cyst/duct are sutured to the outside mucosa to create a permanent opening (neo-ostium).
-
Post-operative care: After the procedure, warm sitz baths, analgesics, sometimes antibiotics (especially if infection present) are used. Activity modification (avoid prolonged sitting, sexual activity until healing) is advised. Recovery generally takes 2-4 weeks.
Comparison of Treatments / Evidence
-
A recent meta-analysis (2023) comparing Word catheter vs marsupialisation found no statistically significant difference in recurrence rate (Word catheter ~7.6% vs marsupialisation ~9.4%).
-
Some other studies suggest marsupialisation may have a lower recurrence or better satisfaction in certain settings. For example, one retrospective review concluded higher recurrence/dissatisfaction in the Word catheter group and suggested marsupialisation as first-line.
-
Sexual function outcomes: One study compared female sexual function index (FSFI) scores after marsupialisation vs gland excision; both improved significantly, and gland excision had slightly better sub-scores but no statistical difference in total score.
Other Surgical Options
-
Gland excision (removal of the Bartholin gland) may be considered in recurrent, complex, or high-risk cases (e.g., suspected malignancy) but carries risks (scarring, dyspareunia) though some data show improved sexual function.
-
Laser treatment, electrosurgery: some emerging evidence suggests electrosurgery of the capsule may yield lower recurrence compared with traditional marsupialisation in small studies.
Choosing the Right Treatment
The choice depends on the patient's symptoms, recurrence history, size of cyst/abscess, presence of infection, patient preference, operator experience and local resources. Marsupialisation remains a reliable approach for recurrent symptomatic cases, though less invasive options like Word catheter may suffice in first-time uncomplicated cases.
Prevention and Management of Bartholin's Gland Cyst/Abscess
Prevention and management of Bartholin's gland cyst or abscess focus on maintaining genital hygiene, reducing infection risks, providing early conservative treatment for mild cases, and using surgical options like marsupialisation for recurrent or complicated cases.
Prevention
While not all cysts/abscesses can be prevented (since duct obstruction may occur idiopathically), some measures may reduce risk:
-
Good vulvovaginal hygiene and prompt treatment of any vulvar infections.
-
Avoiding trauma to the vulvar area (e.g., during sexual activity or vigorous exercise) where possible.
-
Safe sexual practices to reduce risk of sexually transmitted infections, which may predispose to ductal obstruction/infection.
-
Regular pelvic/vulvar examinations for women with a history of Bartholin gland issues to detect early swelling.
-
Prompt treatment of a first cyst/abscess (so it does not recur repeatedly and cause scarring/obstruction).
Management (Post-treatment & Long-term)
-
After marsupialisation or any procedure, follow scheduled post-operative visits to ensure good healing.
-
Encourage sitz baths and analgesics to relieve discomfort.
-
Advise avoidance of prolonged sitting, strenuous exercise or sexual intercourse until the area has sufficiently healed (often 2-4 weeks).
-
Maintain good vulvar hygiene and monitor for signs of recurrence: swelling, pain, discharge.
-
For women who have recurrent problems: consider more definitive surgical options (e.g., excision) or referral to specialist gynecologic surgeon.
-
Psychological support: recurrent vulvar issues can impact sexual function, body image, and quality of life; counselling may help.
Complications of Bartholin's Gland Marsupialisation
Complications of Bartholin's gland marsupialisation are generally rare, with most patients recovering fully within 2-4 weeks. However, both minor and major complications can occur during or after the procedure and should be understood for appropriate management and patient counseling.
Immediate / Short-term Complications
-
Post-operative pain, swelling, bruising.
-
Hematoma formation at surgical site.
-
Infection or delayed healing, especially if pre-existing abscess/infection.
-
Wound dehiscence (opening of the surgical site).
-
Difficulty sitting, walking or urinating initially due to discomfort.
Longer-term Complications
-
Recurrence of cyst/abscess: despite marsupialisation, some patients may experience repeat episodes (though recurrence rate is relatively low). For example, one review quoted 2-13%.
-
Scarring and altered anatomy of the vulvar vestibule, which could lead to discomfort or dyspareunia (pain with intercourse).
-
Possible impact on sexual function: although many studies show improvement, there remains risk of altered sensation or pain.
-
Rarely fistula formation, persistent drainage or need for further surgery.
-
In older women, if underlying vulvar carcinoma was missed, there is potential risk of delayed diagnosis (not a complication of the procedure per se but a diagnostic consideration) - hence the importance of thorough evaluation.
How to Mitigate Risks
-
Pre-operative optimisation: treat any infection, ensure good hygiene.
-
Skilled surgical technique: ensure adequate and appropriately sized marsupialisation opening to avoid early closure.
-
Post-operative follow-up and instructions: adherence to sitz bath regimen, avoid early sexual activity, monitor healing.
-
Educate patient about signs of recurrence or complication (persistent pain, discharge, swelling) and when to seek care.
Living with the Condition of Bartholin's Gland Cyst/Abscess (and After Marsupialisation)
Living with a Bartholin's gland cyst or abscess, and adjusting after marsupialisation, involves careful self-care, hygiene, and attention to long-term comfort and recurrence prevention. Most women recover fully and return to normal routines within a few weeks, with minimal risk of recurrence.
Day-to-Day Life
-
Many women with a one-time uncomplicated cyst may manage well with conservative measures and have minimal disruption.
-
For those requiring marsupialisation, the recovery phase should be expected to last 2-4 weeks for full healing; many patients feel better earlier but discomfort (especially sitting, walking, sexual activity) may persist for some days.
-
Early post-op adjustments: avoid prolonged sitting, apply ice packs or sitz baths, wear loose-fitting underwear/clothing, maintain hygiene to reduce friction.
Sexual Activity and Intimacy
-
Because the Bartholin gland contributes to lubrication, patients may worry about sexual function after surgery. Reassuringly, studies show that both marsupialisation and gland excision improve sexual function scores significantly.
-
Most clinicians advise waiting until the area has healed (often 2-4 weeks, or when pain/discharge has resolved) before resuming sexual activity.
-
Open communication with partner, appropriate lubrication, gradual resumption of intimacy, and counselling if dyspareunia persists are advisable.
Psychological/Quality of Life Considerations
-
Recurrent vulvar swellings or surgical procedures may provoke anxiety about body image, recurrence, sexual performance, or malignancy risk; addressing these concerns openly is important.
-
Offering patient education about the condition, expected outcomes, recurrence risk, and self-care strategies helps empower patients.
-
If recurrent problems are causing distress, referral to a gynaecologist with vulvar expertise and possibly a pelvic floor physiotherapist or sexual health specialist may be beneficial.
Follow-Up and Long-Term Outlook
-
After successful marsupialisation, recurrence is uncommon but still possible. Some studies report very low recurrence (~2%) in certain series.
-
Women should continue to monitor for any new lump/swelling, pain, or discharge and seek prompt evaluation if symptoms recur.
-
Encouraging healthy lifestyle, sexual health awareness, and routine gynaecologic care remain important.
Top 10 Frequently Asked Questions about Bartholin's Gland Marsupialisation
1. What is Bartholin's Gland Marsupialisation?
Bartholin's Gland Marsupialisation is a surgical procedure performed to treat a Bartholin's cyst or abscess, which occurs when the duct of the Bartholin's gland becomes blocked.
During the procedure, the cyst or abscess is opened and drained, and the
edges of the skin are stitched to create a permanent small opening.
This allows the gland to drain naturally, preventing fluid buildup and
recurrence of the cyst or abscess.
It is typically performed under local or general anesthesia as a day-care (outpatient) surgery.
2. What is the Bartholin's gland and what does it do?
The Bartholin's glands are two small, pea-sized glands located on each
side of the vaginal opening.
Their main function is to secrete a lubricating fluid that helps keep
the vaginal area moist during sexual activity.
When the duct of one of these glands becomes blocked due to infection or
inflammation, fluid can accumulate, forming a Bartholin's
cyst.
If bacteria infect the cyst, it can become a painful abscess that may
require surgical drainage or marsupialisation.
3. When is Marsupialisation recommended?
Marsupialisation is recommended when:
-
You have recurrent Bartholin's cysts or abscesses.
-
The cyst is large, painful, or infected.
-
Previous simple drainage or antibiotics have failed to prevent recurrence.
-
The cyst significantly interferes with walking, sitting, or sexual activity.
It is often considered the most effective and long-lasting treatment for chronic or recurring Bartholin's cysts.
4. How is the Bartholin's Gland Marsupialisation procedure performed?
The procedure is usually performed under local anesthesia with sedation or general anesthesia, depending on the size and infection level.
Step-by-step overview:
-
The doctor makes a small incision in the cyst or abscess to drain the fluid or pus.
-
Once emptied, the inner walls are cleaned thoroughly to remove any infected tissue.
-
The edges of the cyst are stitched to the vaginal mucosa to create a small, permanent drainage opening.
-
A small gauze dressing may be placed for a few hours to absorb any remaining fluid.
The procedure takes 20-40 minutes, and most patients can go home the same day.
5. What should I expect after the procedure?
After marsupialisation, you may experience:
-
Mild pain or soreness in the vulvar area for a few days.
-
Light vaginal bleeding or discharge.
-
Swelling around the incision site.
These symptoms typically improve within a week.
Your doctor may recommend:
-
Sitz baths (warm water baths) to soothe discomfort and promote healing.
-
Pain relievers or antibiotics, if necessary.
-
Avoiding sexual intercourse or tampon use for at least 2-3 weeks.
Most women return to normal activities within 2-5 days after surgery.
6. Is Bartholin's Gland Marsupialisation painful?
The procedure itself is not painful because it's performed under
anesthesia.
However, mild discomfort or soreness is common for a few days afterward.
Over-the-counter pain relievers like ibuprofen or paracetamol are
usually sufficient to manage post-procedure pain.
Regular sitz baths also help relieve discomfort and speed up healing.
7. What are the risks or complications of Marsupialisation?
While Bartholin's Gland Marsupialisation is generally safe, there are some potential risks:
-
Infection at the surgical site.
-
Bleeding or hematoma formation.
-
Pain or swelling during recovery.
-
Recurrence of the cyst (in a small percentage of cases).
-
Scarring or changes in the appearance of the vulva (rare).
These complications are uncommon when the procedure is performed by an experienced gynecologist and proper post-operative care is followed.
8. How effective is Bartholin's Gland Marsupialisation?
Marsupialisation is considered highly effective, with a success rate of 85-95% in preventing recurrence of Bartholin's cysts or abscesses.
Compared to simple drainage, marsupialisation provides:
-
Better long-term relief.
-
Lower recurrence rate.
-
Faster healing and restoration of normal function.
In rare cases where the cyst returns, the doctor may recommend gland excision (complete removal).
9. How should I care for myself after the surgery?
Proper self-care after marsupialisation promotes faster recovery and reduces infection risk. Follow these steps:
-
Keep the area clean and dry.
-
Take warm sitz baths (2-3 times daily) after the first 24 hours.
-
Avoid sexual intercourse and tampon use until fully healed.
-
Wear loose cotton underwear and avoid tight clothing.
-
Take prescribed antibiotics as directed by your doctor.
-
Attend follow-up appointments to monitor healing.
If you notice severe pain, heavy bleeding, or fever, contact your doctor immediately.
10. Is Bartholin's Gland Marsupialisation covered by insurance?
Yes. Most health insurance providers cover Bartholin's Gland Marsupialisation as it is a medically necessary surgical procedure to treat a cyst or abscess.
Coverage typically includes:
-
Surgeon's fees
-
Hospital or clinic charges
-
Anesthesia costs
-
Postoperative care
It's best to check with your insurance provider and the hospital's billing department in advance to confirm coverage and preauthorization requirements.


