Introduction to Belt Buckling Vitrectomy Endolaser
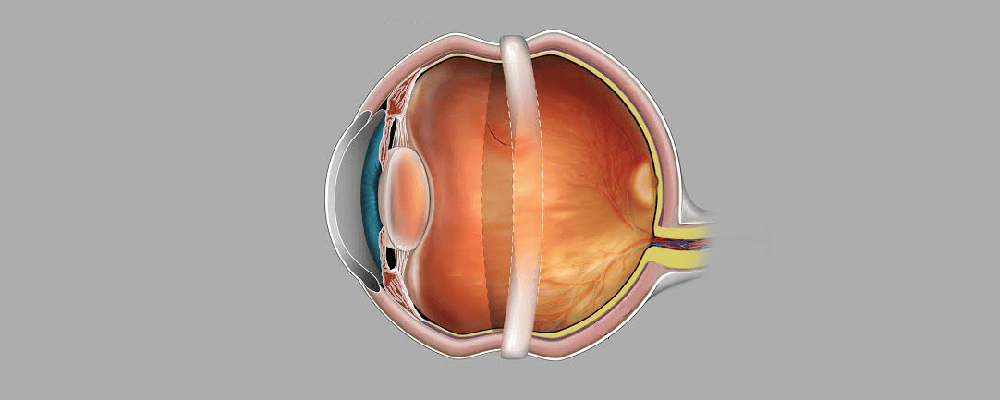
Belt Buckling Vitrectomy Endolaser (BBVE) is an advanced, combined surgical technique employed in the management of complex or high-risk retinal detachments, particularly those associated with proliferative vitreoretinopathy (PVR), giant retinal tears, multiple retinal breaks, or recurrent detachments following previous surgery. This integrated approach leverages the strengths of three complementary procedures to optimize anatomical and functional outcomes. The scleral buckle component, often in the form of a circumferential silicone band, provides external indentation of the sclera, relieving vitreoretinal traction and supporting retinal breaks, especially in the peripheral retina. This external support helps stabilize the globe and reduces the likelihood of recurrent detachment.
The pars plana vitrectomy (PPV) aspect involves meticulous removal of the vitreous gel, including tractional membranes or residual vitreous scaffolds, allowing for controlled manipulation of the retina and facilitating access for internal tamponade agents such as gas or silicone oil. This step addresses internal tractional forces that a scleral buckle alone cannot relieve. Endolaser photocoagulation is then applied internally around retinal breaks or areas at risk, creating strong chorioretinal adhesions to secure the retina and prevent further extension of detachment. BBVE is particularly advantageous in eyes with complex detachment patterns, where single-modality interventions may fail, as it combines external mechanical support with internal traction relief and retinal reinforcement.
Preoperative planning is critical, including careful assessment of the number, size, and location of retinal breaks, the degree of PVR, lens status, and selection of appropriate vitreoretinal instruments and tamponade agents. While BBVE has high success rates in achieving anatomical reattachment, potential complications include cataract formation, elevated intraocular pressure, infection, hypotony, or buckle-related issues such as extrusion or erosion. Overall, BBVE represents a synergistic surgical strategy that maximizes the likelihood of retinal reattachment and visual recovery in eyes with complex retinal pathology.
Causes and Risk of Belt Buckling Vitrectomy Endolaser
Belt Buckling Vitrectomy Endolaser is indicated for several retinal and vitreoretinal conditions where conventional repair methods are insufficient or ineffective. Understanding the causes and risk factors leading to these diseases is essential to appreciate the need for this combined surgical approach.
1. Retinal Detachment
This is the most common reason for Belt Buckling Vitrectomy Endolaser. Retinal detachment occurs when the neurosensory retina separates from the underlying retinal pigment epithelium, disrupting visual function.
Types of Retinal Detachment:
-
Rhegmatogenous Detachment: Caused by a retinal tear or break allowing fluid to pass underneath.
-
Tractional Detachment: Occurs when fibrovascular tissue pulls on the retina, often due to diabetes.
-
Exudative Detachment: Caused by fluid accumulation without a tear, as seen in inflammatory or vascular diseases.
2. Proliferative Diabetic Retinopathy
In advanced diabetes, abnormal new blood vessels grow on the retina and may bleed into the vitreous cavity. Fibrous tissue forms and contracts, leading to tractional retinal detachment. Belt Buckling Vitrectomy Endolaser helps remove the vitreous hemorrhage, release traction, and stabilize the retina.
3. Vitreous Hemorrhage
Blood in the vitreous cavity blocks vision and may result from diabetic retinopathy, retinal tears, or trauma. Persistent or dense hemorrhage often requires vitrectomy to clear the visual axis.
4. Giant Retinal Tears
Extensive circumferential retinal breaks (covering more than 90 degrees) demand combined surgical techniques to reattach the retina securely.
5. Retinal Detachment with PVR (Proliferative Vitreoretinopathy)
PVR involves scarring and membrane formation that cause recurrent detachment even after primary surgery. Combined buckle, vitrectomy, and laser help to flatten and stabilize the retina.
6. Ocular Trauma
Penetrating or blunt trauma can lead to vitreoretinal traction, hemorrhage, or tears requiring reconstructive retinal surgery.
7. Complicated Post-Cataract Surgery
Intraoperative or postoperative complications, such as posterior capsular rupture or dropped nucleus, can cause retinal detachment or vitreous problems that demand surgical correction.
Risk Factors
-
High myopia (elongated eyeball structure)
-
Prior retinal surgery
-
Advanced diabetic retinopathy
-
Family history of retinal detachment
-
Systemic hypertension and vascular disease
-
Aging (liquefaction of vitreous gel)
-
Trauma or head injury
-
Eye inflammation or infection
-
Previous ocular laser procedures
Understanding these underlying causes helps determine the necessity and timing of Belt Buckling Vitrectomy Endolaser.
Symptoms and Signs of Conditions Requiring Belt Buckling Vitrectomy Endolaser
Patients requiring this combined surgery often exhibit symptoms related to retinal detachment, vitreous hemorrhage, or retinal traction. Recognizing these early symptoms is critical for timely diagnosis and intervention.
Common Symptoms:
-
Floaters: Sudden appearance of dark specks, lines, or cobwebs in vision caused by vitreous debris or bleeding.
-
Flashes of Light (Photopsia): Resulting from retinal traction or tears.
-
Blurred or Distorted Vision: Often due to fluid accumulation beneath the retina.
-
Shadow or Curtain Effect: A progressive dark area in the field of vision, indicating retinal detachment.
-
Loss of Peripheral Vision: One of the earliest signs of detachment.
-
Sudden Central Vision Loss: If the macula becomes detached or affected.
-
Visual Field Defects: Gaps or blind spots in the vision field.
-
In Diabetic Retinopathy: Gradual blurring, poor night vision, and visual distortion due to recurrent hemorrhages.
Clinical Signs Observed by the Ophthalmologist:
-
Visible retinal tears or breaks on ophthalmoscopy.
-
Vitreous hemorrhage obscuring the retina.
-
Retinal detachment folds or fluid.
-
Abnormal vitreoretinal adhesions.
-
Neovascularization on the retina or optic disc.
-
Reduced visual acuity on testing.
Timely recognition of these symptoms allows for early surgical intervention, improving prognosis and visual outcomes.
Diagnosis of Belt Buckling Vitrectomy Endolaser
A comprehensive ophthalmic evaluation is essential before determining the need for Belt Buckling Vitrectomy Endolaser. The diagnostic process involves clinical assessment, advanced imaging, and functional tests to assess the retina’s structural and functional status.
1. Detailed Ophthalmic History and Examination
-
Assessment of visual acuity and field.
-
Intraocular pressure measurement.
-
Slit-lamp biomicroscopy to evaluate anterior and posterior segments.
2. Fundus Examination
-
Indirect Ophthalmoscopy: Allows wide-angle view of the retina to identify breaks, tears, or detachment.
-
Scleral Indentation: Helps detect peripheral retinal pathology.
3. Optical Coherence Tomography (OCT)
-
Provides cross-sectional, high-resolution images of the retina.
-
Helps detect subretinal fluid, macular detachment, and epiretinal membranes.
4. B-Scan Ultrasonography
-
Used when the retina is not visible due to hemorrhage or opacity.
-
Confirms retinal detachment and evaluates vitreous abnormalities.
5. Fundus Fluorescein Angiography
-
Highlights areas of retinal ischemia, neovascularization, or leakage.
-
Useful in diabetic retinopathy cases.
6. Fundus Photography
-
Baseline documentation and monitoring of disease progression.
7. Electrophysiological Tests (Optional)
-
Electroretinogram (ERG) and visual evoked potential (VEP) assess retinal and optic nerve function, particularly before surgery in chronic cases.
Through this multi-step diagnostic approach, surgeons plan the extent of vitrectomy, buckle placement, and laser application to achieve maximum retinal reattachment and visual recovery.
Treatment Options of Belt Buckling Vitrectomy Endolaser
Belt Buckling Vitrectomy Endolaser is a combination surgical intervention performed in specialized ophthalmic operating theaters under strict aseptic conditions.
1. Preoperative Preparation
-
Full ophthalmic assessment and systemic evaluation.
-
Blood sugar, blood pressure, and coagulation control.
-
Informed consent explaining potential risks, outcomes, and recovery.
-
Pupil dilation and administration of local or general anesthesia.
2. Surgical Procedure Steps
A. Scleral Buckling (Belt Application)
-
A silicone band or sponge is sutured to the sclera around the equator of the eyeball.
-
The buckle exerts inward pressure, closing retinal breaks and reducing vitreoretinal traction.
-
The buckle may be temporary or permanent depending on the case.
B. Pars Plana Vitrectomy
-
Tiny incisions (0.5 mm) are made to insert microsurgical tools (vitrector, light probe, infusion cannula).
-
The vitreous gel, membranes, and hemorrhage are removed.
-
The retina is flattened by fluid-air exchange.
-
Perfluorocarbon liquids may be used to stabilize the retina during manipulation.
C. Endolaser Photocoagulation
-
An endolaser probe delivers precise laser burns around retinal tears.
-
These burns create strong chorioretinal adhesions, sealing off breaks and preventing fluid entry.
D. Internal Tamponade
-
A gas bubble (SF6, C3F8) or silicone oil is introduced to hold the retina in place.
-
The type of tamponade depends on the complexity and location of the detachment.
E. Closure
-
Instruments are withdrawn, incisions closed, and antibiotic-steroid drops applied.
3. Postoperative Management
-
Strict head positioning to keep the tamponade bubble in optimal position.
-
Topical antibiotic, steroid, and cycloplegic medications.
-
Avoid air travel until the gas bubble resolves.
-
Regular follow-up to monitor retinal status and intraocular pressure.
The combination of these steps ensures comprehensive retinal reattachment and stabilization.
Prevention and Management of Belt Buckling Vitrectomy Endolaser
Preventive Strategies
While not all causes of retinal detachment are preventable, certain lifestyle and medical measures can reduce risks:
-
Routine Eye Examinations: Especially for myopic and diabetic patients.
-
Strict Diabetes Control: Prevents proliferative retinopathy and subsequent detachment.
-
Prompt Management of Retinal Tears: Early laser photocoagulation for small tears.
-
Eye Protection: Use protective eyewear during sports or hazardous activities.
-
Avoid Eye Rubbing: Especially in predisposed individuals.
-
Monitor Visual Symptoms: Early reporting of flashes, floaters, or vision loss.
Postoperative Management
-
Head Positioning: Crucial when gas tamponade is used.
-
Medication Adherence: Follow all topical and systemic prescriptions.
-
Lifestyle Adjustments: Avoid heavy exercise and rapid eye movements.
-
Periodic Eye Check-ups: To detect recurrence or new retinal issues.
-
Blood Sugar and Blood Pressure Control: Essential in diabetic and hypertensive patients.
With effective preventive and postoperative management, long-term visual stability can be achieved.
Complications of Belt Buckling Vitrectomy Endolaser
Though modern techniques have reduced risks, complications may occur and require timely management.
Early Complications
-
Intraocular bleeding (vitreous or choroidal hemorrhage)
-
Raised intraocular pressure (glaucoma)
-
Infection (endophthalmitis)
-
Corneal edema or epithelial defects
-
Pain, inflammation, or redness
Late Complications
-
Cataract formation (common after vitrectomy)
-
Recurrent retinal detachment
-
Proliferative vitreoretinopathy (PVR)
-
Diplopia due to buckle-induced muscle imbalance
-
Silicone oil–related complications (emulsification, migration)
-
Epiretinal membrane formation
-
Reduced night vision or visual field defects
Early diagnosis and prompt treatment of complications help preserve visual function.
Living with the Condition After Belt Buckling Vitrectomy Endolaser
Recovery after Belt Buckling Vitrectomy Endolaser varies depending on disease severity, surgical complexity, and individual healing. Vision improvement may be gradual over weeks to months.
Post-Surgical Lifestyle Tips
-
Maintain regular follow-ups with your ophthalmologist.
-
Protect your eyes from injury and sunlight (wear sunglasses).
-
Avoid strenuous activities or rapid head movements during healing.
-
Use prescribed eye drops as directed.
-
If silicone oil is used, a second procedure may be required for removal.
-
Manage systemic diseases like diabetes, hypertension, and cholesterol.
Visual Rehabilitation
Patients with partial vision loss may benefit from:
-
Low-vision aids (magnifiers, adaptive lighting).
-
Vision therapy and rehabilitation programs.
-
Psychological counseling to cope with visual challenges.
Emotional and Social Well-being
Vision problems can affect daily functioning, independence, and emotional health. Support groups and counseling services can help patients adapt and regain confidence.
With commitment to treatment and lifestyle adjustments, most patients experience improved or stabilized vision and maintain a satisfactory quality of life.
Top 10 Frequently Asked Questions about Belt Buckling Vitrectomy with Endolaser
This procedure is a hybrid technique that combines three key components:
-
Vitrectomy: Removal of the vitreous gel to access the retina.
-
Scleral Buckling: Placement of a silicone band around the eye to indent the sclera and relieve traction on the retina.
-
Endolaser Photocoagulation: Application of laser to the retina to seal retinal tears and prevent fluid accumulation beneath the retina.
Together, these steps aim to reattach the retina and stabilize the eye's internal structures.
2. Why is this procedure performed?
The combined approach is typically indicated for:
-
Rhegmatogenous retinal detachment, where a retinal tear allows fluid to accumulate beneath the retina.
-
Diabetic retinopathy with complications.
-
Traumatic retinal injuries.
-
Macular holes or epiretinal membranes.
It is particularly beneficial when other treatments have not been successful or when the detachment is extensive.
3. How is the procedure performed?
The surgery is conducted under general anesthesia and involves:
-
Vitrectomy: Removing the vitreous gel to access the retina.
-
Scleral Buckling: Placing a silicone band around the eye to relieve retinal traction.
-
Endolaser Photocoagulation: Applying laser to retinal tears to seal them.
The entire procedure typically lasts 1.5 to 2 hours.
4. What are the benefits of this combined approach?
This hybrid technique offers several advantages:
-
Enhanced Retinal Reattachment: Combines internal and external support for the retina.
-
Reduced Risk of Recurrence: Addresses multiple causes of detachment simultaneously.
-
Improved Visual Outcomes: Higher success rates compared to single-modality treatments.
-
Shorter Recovery Time: Efficient treatment of complex cases.
5. What are the risks and complications?
As with any surgery, potential risks include:
-
Infection: Postoperative infections can occur.
-
Bleeding: Hemorrhage within the eye.
-
Increased Intraocular Pressure: May lead to glaucoma.
-
Cataract Formation: Especially in older patients.
-
Recurrence of Retinal Detachment: In some cases.
However, the combined approach has shown to reduce the incidence of these complications.
6. What is the recovery process like?
Postoperative recovery typically involves:
-
Hospital Stay: Usually 1 to 2 days.
-
Medication: Use of eye drops to prevent infection and reduce inflammation.
-
Positioning: Maintaining specific head positions to aid retinal reattachment.
-
Follow-up Visits: Regular check-ups to monitor healing.
Most patients can resume normal activities within 4 to 6 weeks.
7. How effective is the procedure?
Studies indicate that the combined approach has a high success rate:
-
Single-Surgery Success Rate: Approximately 93.3%.
-
Visual Acuity Improvement: Significant improvement in visual outcomes post-surgery.
The success largely depends on the extent of retinal damage and the timeliness of the intervention.
8. Will I need to stay in the hospital?
Typically, patients stay in the hospital for 1 to 2 days for monitoring. The procedure is usually performed on an outpatient basis, allowing for discharge the same day or the following day.
9. Are there any long-term considerations?
After surgery, patients should:
-
Avoid Strenuous Activities: Refrain from heavy lifting and vigorous exercise for several weeks.
-
Monitor Vision: Report any sudden changes in vision to the doctor immediately.
-
Regular Check-ups: Attend all scheduled follow-up appointments to ensure proper healing.
Most patients experience stable vision post-recovery.
10. Is this procedure covered by insurance?
Yes, most health insurance plans cover the cost of the Belt Buckling Vitrectomy with Endolaser procedure, as it is considered a medically necessary treatment for retinal detachment and related conditions. It's advisable to check with your insurance provider for specific coverage details and any pre-authorization requirements.


