Introduction to Birmingham Hip Resurfacing
Birmingham Hip Resurfacing (BHR) is an advanced surgical procedure designed as an alternative to total hip replacement, primarily for younger and more active patients suffering from hip joint damage due to arthritis or injury. Developed in Birmingham, England, in the late 1990s by Mr. Derek McMinn, this innovative technique aims to preserve more of the patient's natural bone while providing pain relief and restoring mobility.
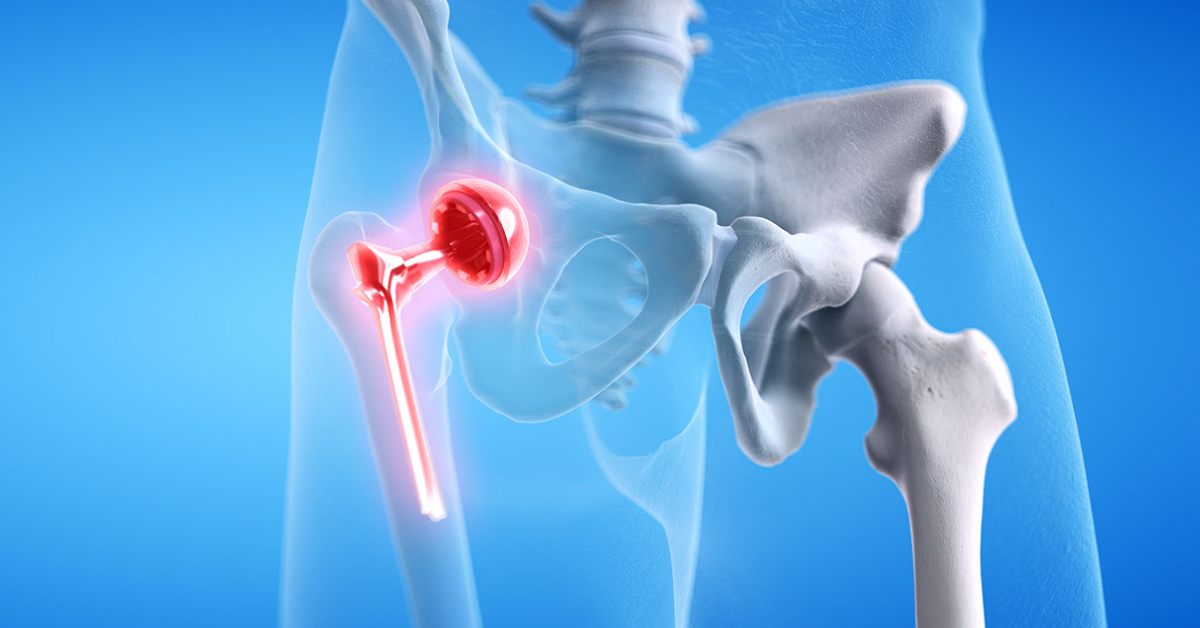
Unlike traditional total hip replacement, which involves removing the entire femoral head and replacing it with a prosthesis, BHR involves reshaping and capping the femoral head with a smooth metal covering and inserting a corresponding metal socket into the hip bone (acetabulum). This bone-conserving approach makes future revisions easier, improves joint stability, and offers excellent functional outcomes for patients with active lifestyles.
Over the years, BHR has gained global recognition as one of the most durable and natural-feeling solutions for suitable candidates, particularly men under 60 with strong bone quality. The procedure has demonstrated long-term success rates exceeding 90% in experienced surgical centers.
Causes and Risk Factors for Birmingham Hip Resurfacing (Candidates for the Procedure)
Birmingham Hip Resurfacing is typically indicated for patients suffering from degenerative conditions of the hip joint where conservative management has failed. The “cause” in this context refers to the underlying diseases or conditions that damage the hip joint enough to require surgical intervention.
Common Causes
-
Osteoarthritis (Degenerative Joint Disease): The most frequent cause, where the cartilage cushioning the hip joint wears down, leading to pain, stiffness, and reduced mobility.
-
Avascular Necrosis (AVN): Loss of blood supply to the femoral head causes bone tissue death and collapse, resulting in severe pain and deformity.
-
Rheumatoid Arthritis: Chronic inflammation damages cartilage and joint structures, leading to joint destruction.
-
Post-Traumatic Arthritis: Arthritis following previous hip injuries or fractures that disrupt joint alignment.
-
Hip Dysplasia: Developmental abnormalities of the hip socket causing premature arthritis.
Risk Factors
-
Age: Typically performed in patients between 40-60 years.
-
Sex: Men have better outcomes due to larger bone structure and denser bone quality.
-
Activity Level: Best suited for physically active individuals who need strong, stable hip function.
-
Bone Density: Healthy bone tissue is essential for supporting the metal cap and implant stability.
-
Pre-existing Conditions: Conditions such as osteoporosis, metal allergies, or kidney disease may limit eligibility.
Symptoms and Signs Leading to Birmingham Hip Resurfacing
Patients who are potential candidates for BHR often exhibit advanced symptoms of hip joint deterioration. These symptoms significantly affect daily life, mobility, and independence.
Typical Symptoms
-
Chronic Hip Pain: Persistent pain in the groin, thigh, or buttock that worsens with movement or activity.
-
Reduced Range of Motion: Stiffness and difficulty performing simple movements such as bending, sitting, or climbing stairs.
-
Limping or Altered Gait: Uneven walking due to pain or weakness in the affected leg.
-
Joint Grinding or Clicking: Sensation of friction or locking in the hip joint due to cartilage loss.
-
Night Pain: Discomfort while lying on the affected side, leading to disturbed sleep.
-
Functional Limitation: Difficulty participating in sports, walking long distances, or even standing for prolonged periods.
If these symptoms persist despite medication, physical therapy, or lifestyle modification, surgical evaluation for hip resurfacing or replacement becomes necessary.
Diagnosis of Hip Conditions Requiring Birmingham Hip Resurfacing
Before recommending Birmingham Hip Resurfacing, orthopedic surgeons perform a comprehensive diagnostic evaluation to determine if the patient is an ideal candidate.
Diagnostic Process
-
Medical History and Physical Examination:
The surgeon reviews symptoms, activity level, past injuries, and overall health. A physical exam assesses hip motion, strength, and pain location. -
Imaging Studies:
-
X-rays: To evaluate bone quality, joint space narrowing, and deformity.
-
MRI (Magnetic Resonance Imaging): To detect early avascular necrosis or soft tissue damage.
-
CT Scans: For precise preoperative mapping of the hip anatomy.
-
Bone Density Tests: To confirm adequate bone strength for resurfacing implants.
-
-
Laboratory Tests:
-
Blood tests may be done to rule out infection or inflammatory arthritis.
-
Metal allergy testing may be recommended in sensitive individuals.
-
The diagnostic process helps determine the extent of damage, bone strength, and suitability for the BHR system. Patients with poor bone density or certain metal sensitivities may be directed toward alternative treatments.
Treatment Options: The Birmingham Hip Resurfacing Procedure
Birmingham Hip Resurfacing is a technically demanding surgery that requires specialized training and equipment. The goal is to replace the damaged joint surfaces while conserving bone and maintaining the patient's anatomy.
Preoperative Preparation
-
Full medical evaluation and anesthesia assessment.
-
Pre-surgical imaging for implant sizing and placement.
-
Patient education regarding postoperative rehabilitation.
Surgical Procedure
-
Anesthesia: Usually performed under general or spinal anesthesia.
-
Incision and Exposure: The surgeon makes an incision over the hip joint to expose the femoral head and acetabulum.
-
Femoral Head Preparation: The damaged cartilage is removed, and the femoral head is reshaped to fit the metal cap precisely.
-
Implant Placement:
-
A metal cap (cobalt-chrome alloy) is fitted over the femoral head.
-
A matching metal cup is placed into the hip socket.
-
-
Alignment and Fixation: The components are aligned to ensure smooth joint motion and stability.
-
Closure and Recovery: The incision is closed, and the patient is moved to recovery for observation.
Postoperative Rehabilitation
-
Early mobilization, often within 24 hours.
-
Gradual physiotherapy focusing on strength, balance, and mobility.
-
Most patients resume light activities within 6 weeks and full activity in 3-6 months.
Prevention and Management After Birmingham Hip Resurfacing
Although BHR is primarily a corrective procedure rather than preventive, certain measures help maximize its success and longevity.
Prevention Before Surgery
-
Early Management of Hip Disorders: Timely diagnosis and treatment of arthritis or trauma can delay progression.
-
Healthy Lifestyle: Maintaining ideal body weight reduces hip stress.
-
Avoiding High-Risk Activities: Limiting repetitive hip strain from heavy sports or trauma can protect joint health.
Postoperative Management
-
Physiotherapy: Essential for restoring strength, flexibility, and balance.
-
Weight Management: Prevents undue stress on the new joint.
-
Regular Follow-Up: X-rays and physical assessments ensure proper implant positioning.
-
Activity Modification: High-impact sports like long-distance running should be limited, while swimming, cycling, and walking are encouraged.
Complications of Birmingham Hip Resurfacing
While BHR has an excellent safety record, like all major surgeries, it carries certain risks and potential complications.
Early Complications
-
Infection: Occurs in rare cases; prevented through antibiotics and sterile surgical techniques.
-
Blood Clots (Deep Vein Thrombosis): Prevented with blood thinners and mobility exercises.
-
Nerve or Vessel Injury: Very rare, minimized by skilled surgical technique.
Late Complications
-
Femoral Neck Fracture: A known risk due to bone stress, particularly in patients with weak bone quality.
-
Metal Ion Release: Metal-on-metal bearings may release ions into the bloodstream; regular monitoring is recommended.
-
Implant Loosening or Wear: Over time, wear or poor fixation may require revision surgery.
-
Leg Length Discrepancy: Rare and usually minor.
Proper surgical selection and expert technique significantly reduce complication risks.
Living with Birmingham Hip Resurfacing
After successful recovery, most patients enjoy a pain-free, active lifestyle for many years.
Long-Term Outcomes
-
High Success Rates: Clinical studies report implant survival rates above 90% after 15-20 years.
-
Natural Movement: Patients report more natural joint motion compared to total hip replacement.
-
Active Lifestyle: Enables return to recreational sports, cycling, swimming, and hiking.
-
Improved Quality of Life: Marked improvement in pain, independence, and confidence.
Tips for Long-Term Care
-
Regular follow-up every 1-2 years.
-
Maintain muscle strength and joint flexibility.
-
Avoid high-impact trauma or extreme sports.
-
Report any new pain or swelling promptly to the surgeon.
Birmingham Hip Resurfacing offers an ideal balance between durability, mobility, and bone preservation — a leading choice for younger, active patients seeking to restore hip function and quality of life.
Top 10 Frequently Asked Questions about Birmingham Hip Resurfacing (BHR)
1. What is Birmingham Hip Resurfacing (BHR)?
BHR is a surgical procedure that involves capping the femoral head (the ball of the hip joint) with a metal prosthesis and replacing the acetabulum (hip socket) with a metal cup. Unlike total hip replacement, which involves removing the femoral head and inserting a long stem into the femur, BHR preserves more of the patient's natural bone.
2. Who is an ideal candidate for BHR?
Ideal candidates are typically active individuals under 60 years of age with good bone quality. Conditions such as osteoarthritis, hip dysplasia, or avascular necrosis may be treated with BHR, provided the femoral head is healthy. Patients with poor bone quality or certain systemic conditions may not be suitable candidates.
3. How does BHR differ from total hip replacement (THR)?
The primary difference lies in the femoral component. In THR, the femoral head is removed and replaced with a stemmed prosthesis, whereas in BHR, the femoral head is preserved and capped with a metal prosthesis. BHR is considered more bone-conserving and may offer advantages in younger, more active patients.
4. What materials are used in BHR implants?
BHR implants are typically made from a cobalt-chromium-molybdenum alloy, known for its durability and wear resistance. The metal-on-metal design aims to reduce wear and tear compared to traditional polyethylene components.
5. How long do BHR implants last?
While individual results may vary, studies suggest that BHR implants have a high survival rate. For instance, a clinical study showed a 98.4% survivorship at the five-year mark. Long-term data indicates that BHR implants can last 20 to 30 years, making them a viable option for younger patients.
6. What is the recovery process like after BHR surgery?
Recovery times can vary, but many patients are able to walk with assistance within a day or two post-surgery. Physical therapy typically begins shortly after surgery to strengthen the hip and improve mobility. Most patients can resume normal activities, including light sports, within a few months, with more strenuous activities introduced gradually.
7. What are the potential risks and complications of BHR?
As with any surgical procedure, BHR carries risks such as infection, blood clots, nerve or blood vessel damage, and implant-related issues. Specific to BHR, there is a risk of metal ion release due to the metal-on-metal design, which can lead to adverse reactions in some patients. Regular follow-up and monitoring are essential to detect and address any complications early.
8. Can I return to sports after BHR?
Many patients are able to return to low-impact activities like swimming and cycling within a few months post-surgery. High-impact sports such as running or contact sports may be resumed after a longer period, depending on individual recovery and surgeon recommendations. It's crucial to follow your surgeon's advice and gradually increase activity levels to ensure the longevity of the implant.
9. What is the typical hospital stay after BHR surgery?
The average hospital stay following BHR surgery is approximately 2 to 3 days. Patients are monitored for complications and begin rehabilitation exercises during this time. Discharge planning includes instructions on pain management, mobility aids, and follow-up appointments.
10. How often should I have follow-up appointments after BHR?
Follow-up schedules can vary based on individual circumstances, but a typical regimen includes visits at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and then annually thereafter. These appointments allow your healthcare provider to monitor the implant's condition and address any concerns promptly.


