Introduction to Bladder Biopsy
A bladder biopsy is a diagnostic procedure in which a small piece of tissue is
removed from the lining or wall of the urinary bladder so it can be examined
under the microscope. This test is typically performed when abnormalities
of the bladder are identified - for example during a visual examination of the
bladder (cystoscopy) - or when there is suspicion of disease such as a
tumour.
While the term "biopsy" may evoke fear, the procedure is relatively common in
urology, and plays a key role in identifying benign vs malignant conditions of
the bladder, as well as guiding further treatment. For the reader, understanding
bladder biopsy is important because it is often one of the first steps when
there is blood in the urine, bladder symptoms, or imaging findings. It's not a
"disease" by itself, but a diagnostic tool - though it does carry some risks and
implications, which will be covered in the later sections.
This article will cover the causes and risks, symptoms and signs that lead to a bladder biopsy, how it is diagnosed/taken, what treatment options follow, prevention or mitigation, possible complications, and how to live with the condition when a biopsy (and its findings) has taken place.
Causes and Risk of Bladder Biopsy
In this context, "causes" refers to the reasons why a bladder biopsy is conducted. That is, what underlying conditions or risk factors prompt the need for a biopsy of bladder tissue.
Why a biopsy might be needed
-
The presence of blood in the urine (haematuria), either visible or microscopic, is a common reason.
-
Other urinary symptoms such as frequent urination, pain or burning on urination, urgency, or abnormal findings on bladder imaging or cystoscopy.
-
During a cystoscopic examination, if the bladder wall appears abnormal (e.g., a visible tumour, mass, irregularity), a biopsy is often taken to determine whether cancer or other disease is present.
-
Sometimes for monitoring of known bladder disease or to investigate persistent unexplained bladder symptoms.
Risk factors and patient characteristics
While the biopsy itself is a procedural decision, underlying risk factors for bladder pathology (which drive the decision to biopsy) include:
-
Smoking: a major risk factor for bladder cancer (hence increased need for biopsy when abnormalities are found).
-
Exposure to certain industrial chemicals (aniline dyes, aromatic amines) and environmental toxins.
-
Chronic bladder inflammation or infections.
-
Prior radiation therapy to the pelvis or bladder.
-
Prior instrumentation of the bladder, long-term catheterization.
-
Age: bladder disease is more common in older adults; thus biopsies are more frequently done in higher-age groups.
Because a bladder biopsy is done when there is suspicion of pathology, you might think of the risk of "having a biopsy" as essentially the risk of the underlying bladder condition; but also the procedure carries its own risk (bleeding, infection) which we'll discuss later.
Symptoms and Signs Leading to Bladder Biopsy
This section describes the clinical presentation that may lead a physician to recommend a bladder biopsy.
Typical signs and symptoms
-
Haematuria (blood in the urine): this is often the most prominent - either visible red blood or detected on testing.
-
Painful urination (dysuria) and/or burning sensation when passing urine.
-
Frequent urination or urgency: changes in bladder habits may prompt investigation.
-
Lower back or flank pain: in some cases if the bladder lesion causes obstruction or irritation.
-
Occasionally, irritative bladder symptoms (feeling of incomplete emptying, need to void frequently at night) or unexplained urinary tract infections.
What the patient and clinician should note
-
If there is persistent or recurrent blood in the urine, especially in adults over 40, this warrants evaluation (and possibly biopsy).
-
Accompanying symptoms like weight loss, fatigue, or other systemic signs may raise concern for more serious pathology.
-
The absence of symptoms does not rule out important bladder pathology: sometimes irregularities are found incidentally on imaging or during cystoscopy for other reasons.
Thus, when these signs are present, particularly in a person with risk factors, a bladder biopsy becomes a key diagnostic next-step.
Diagnosis of Bladder Biopsy (i.e., how the biopsy is performed and processed)
Here we describe the procedure, preparation, what the biopsy shows, and how results are interpreted.
Pre-procedure preparation
-
The patient will be asked to sign informed consent.
-
You may be asked to empty your bladder just before the procedure.
-
Sometimes antibiotics are given prophylactically if there is risk of infection.
-
Your doctor will review medications (especially anticoagulants/bleeding risk), allergies, prior urinary tract history.
-
Fasting or sedation may be required if the biopsy is done under general anaesthesia (depending on the extent).
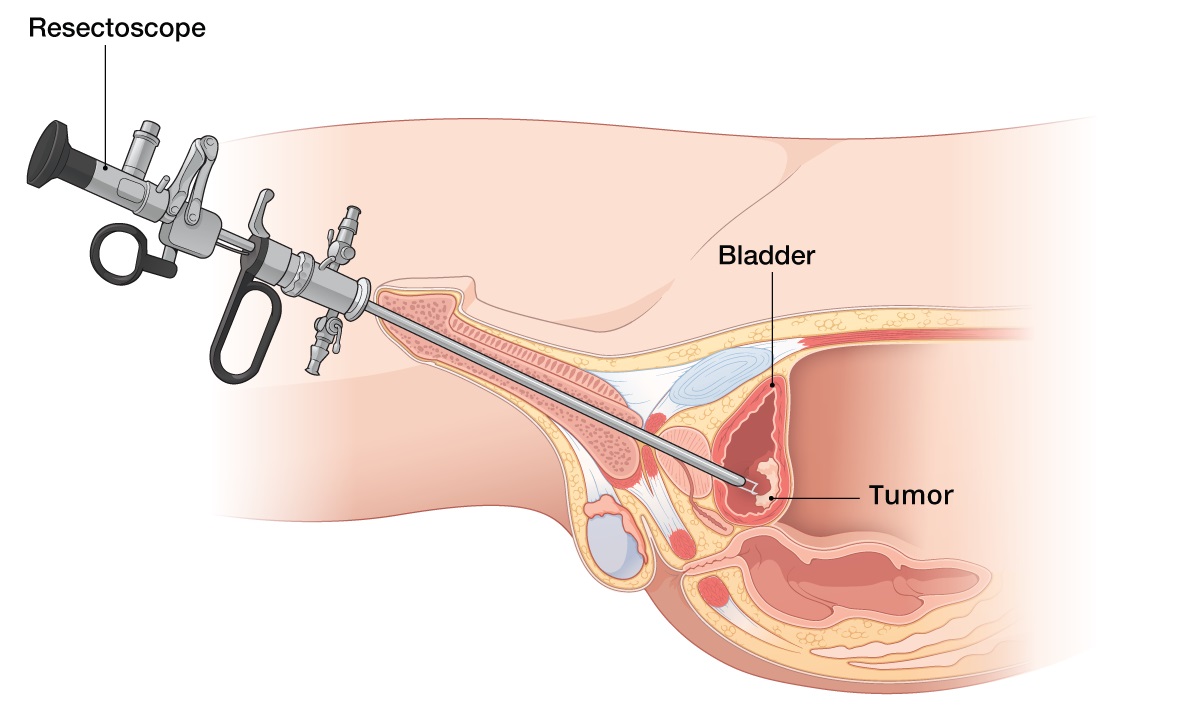
The procedure itself
-
The biopsy is typically done via a cystoscopy: a thin, lighted tube (cystoscope) is inserted through the urethra up into the bladder.
-
The bladder may be filled with a sterile fluid to expand it and allow better visualization.
-
Under direct vision, the urologist identifies suspicious areas and uses biopsy forceps or an electrocautery loop to remove small pieces of tissue.
-
The tissue is sent to pathology for histologic assessment (to determine presence/grade of cancer, depth of invasion, or other bladder wall changes).
What to expect after the procedure
-
The procedure usually takes about 15-30 minutes, in many cases as an outpatient.
-
It is common to see some blood in the urine for a day or two afterwards.
-
You may feel burning on urination, urgency or frequency for a short time.
-
Recovery instructions typically include drinking plenty of fluids, avoiding heavy lifting, and observing for signs of complications.
How results are interpreted
-
The pathology report will indicate whether the tissue is normal, has non-malignant changes (e.g., inflammation, cysts, diverticula), or shows malignant cells.
-
In cancer cases, the report will describe grade (how abnormal the cells look) and stage/invasion (how deep into the bladder wall).
-
These results guide subsequent management (treatment, surveillance, further imaging).
In short: diagnosis via bladder biopsy is straightforward in concept, but the key lies in careful patient preparation, skilled execution, and proper pathology interpretation.
Treatment Options Following Bladder Biopsy
Since the biopsy itself is a diagnostic procedure, "treatment options" refer to what happens following the biopsy, depending on the findings.
If the biopsy is benign or non-malignant
-
If no malignancy is found, but other abnormalities (e.g., inflammation, infection) are present, treatment will focus on the underlying cause (e.g., antibiotics, anti-inflammatory therapy, bladder irrigation).
-
Regular monitoring may be recommended, especially if the biopsy identifies premalignant changes or the patient remains symptomatic.
-
Lifestyle changes (e.g., smoking cessation) may be advised to reduce further risk.
If malignancy is found (bladder cancer)
-
The biopsy results will guide the staging and grading of the cancer, which are critical in deciding treatment: superficial (non-muscle invasive) vs muscle-invasive, low grade vs high grade.
-
Treatment options may include:
-
Transurethral resection of bladder tumour (TURBT) - removal of tumour via cystoscope.
-
Intravesical therapy (e.g., BCG, chemotherapy instilled into the bladder).
-
Radical cystectomy (removal of bladder) in muscle-invasive disease.
-
Systemic chemotherapy, immunotherapy, radiation in advanced cases.
-
-
Close follow-up is mandatory because bladder cancer has a significant recurrence risk.
Post-biopsy care
-
After the biopsy (and any associated procedure), management includes monitoring for bleeding, infection, ensuring adequate hydration, and following instructions (avoid heavy lifting, sexual activity for a short period, etc.).
-
Pain control (usually mild) and bladder rest (fluid flushing) are often advised.
So the "treatment" after a bladder biopsy depends entirely on what the biopsy shows - it is less about the biopsy itself and more about subsequent steps.
Prevention and Management (Post-Procedure Care)
While you cannot "prevent" a bladder biopsy per se (since it is a diagnostic step), you can minimise the need for one by reducing risk of bladder disease, and you can manage your post-procedure care to improve outcomes.
Preventive strategies
-
Smoking cessation: As smoking is a major risk factor for bladder cancer, quitting reduces the risk of needing invasive procedures.
-
Avoid occupational exposures: If you work in industries with exposure to bladder carcinogens (dyes, chemicals), use protective measures.
-
Prompt management of bladder infections or irritations: Chronic bladder inflammation can increase risk of bladder pathology.
-
Regular follow-up: Especially for individuals with prior bladder disease, or prior bladder cancer, keeping scheduled check-ups can catch issues earlier.
Post-procedure management (after biopsy)
-
Hydration: Drinking ample water helps flush the bladder and speeds recovery.
-
Avoid irritants: For a few days, avoiding caffeine, alcohol, acidic foods, and heavy physical exertion may help reduce bladder irritation.
-
Monitor for signs of complications (see next section): bleeding, infection, inability to urinate.
-
Follow-up appointments: Importantly, keep your follow-up visits to review pathology results and determine next steps.
-
Lifestyle modifications: If biopsy indicates risk (e.g., premalignant changes), adopt healthy bladder habits - avoid bladder irritants, maintain normal weight, manage comorbidities like diabetes or hypertension.
By combining risk-factor modification with attentive post-procedure care, patients can optimise outcomes and reduce chances of complications or recurrence.
Complications of Bladder Biopsy
Though the procedure is generally safe, as with any invasive intervention there are potential complications which patients should be aware of.
Common and expected
-
Blood in the urine: Minor bleeding is common and may last a day or two.
-
Burning on urination, urinary frequency or urgency: Because the bladder lining has been disturbed.
Less common but serious
-
Urinary tract infection (UTI): Since instrumentation of the urinary tract can introduce bacteria.
-
Bleeding / clots: If bleeding is more than expected or large clots form, this may block the bladder.
-
Bladder perforation: Rarely, the bladder wall may be inadvertently injured or perforated during the biopsy.
-
Inability to urinate / urinary retention: If swelling or clot blocks the bladder outlet.
-
Need for further surgery: If serious complications or findings require major intervention.
When to seek urgent care
Contact your physician if you experience:
-
Heavy bleeding (bright red stream or larger clots)
-
Fever, chills, signs of infection (cloudy or foul-smelling urine)
-
Painful inability to pass urine
-
Severe pain, or worsening of symptoms after initial improvement.
The key message: While risks are relatively low, staying vigilant for complications ensures prompt management.
Living with the Condition / After a Bladder Biopsy
This section describes what patients should know and how they can adjust after having undergone a bladder biopsy - especially given its results.
Immediately post-procedure
-
Expect some blood-tinged urine, mild discomfort during urination. These should improve within 24-48 hours.
-
Rest the bladder: avoid heavy exercise, intense lifting, sexual activity for a short period as advised by your doctor.
-
Stay hydrated, drink water to flush out the bladder.
If the biopsy finds no disease
-
You may resume your normal life after recovery, but continue healthy bladder habits and regular check-ups if indicated.
-
Remain attentive to new bladder symptoms - recurrence of blood in urine or bladder irritation should prompt follow up.
If the biopsy finds disease (e.g., bladder cancer or other pathology)
-
You will likely embark on a treatment and surveillance path: attending follow-up cystoscopies, monitoring for recurrence, managing treatments (which may include surgery, intravesical therapy).
-
That means lifestyle factors become even more important: quitting smoking, avoiding bladder irritants, maintaining good general health, and adhering to follow-up schedules.
-
Mental health is also important: diagnosis of bladder cancer or premalignant changes can raise anxiety; open discussion with your physician, urologist, or a counsellor can help.
Bladder health habits going forward
-
Hydration: Regular fluid intake helps flush toxins and reduce bladder irritation.
-
Avoiding irritants: Reduce consumption of caffeine, alcohol, spicy foods if you are prone to bladder irritation.
-
Pelvic floor and bladder exercise: Some patients may benefit from bladder-training or pelvic-floor physiotherapy (especially if they have had bladder interventions).
-
Monitoring: Keep track of any changes in urinary habits, new episodes of haematuria, urgency/frequency, pain. Report promptly.
Impact on quality of life and work
-
Most patients return to normal activities once recovered from the biopsy, but if treatment is needed (e.g., for bladder cancer), there may be ongoing adjustments (frequent hospital visits, urinary side-effects, need for periodic surveillance).
-
It helps to plan: for example, staying near healthcare facility, arranging transport, taking time off work if needed, and discussing implications with your employer or social support network.
Follow-up care
-
Your urologist will schedule follow-up appointments, possibly repeat cystoscopies, imaging, and urine tests.
-
Maintaining a good relationship with your healthcare team is key: ask questions, understand your pathology report, know what signs to monitor.
-
Adopting a "watchful" mindset can empower you: rather than fear, view the biopsy outcome (whether benign or malignant) as a starting point for a tailored plan.
Top 10 Frequently Asked Questions about Bladder Biopsy
1. What is a Bladder Biopsy?
A bladder biopsy is a medical procedure in which a small tissue sample is taken from the inner lining of the bladder. This sample is then sent to a laboratory, where a pathologist examines it under a microscope to look for abnormal cells, inflammation, infection, or cancerous growths.
The bladder biopsy is usually performed during a cystoscopy-a procedure that involves inserting a thin, lighted tube called a cystoscope into the bladder through the urethra. This allows the doctor to directly view the inside of the bladder and precisely collect tissue from suspicious areas.
Bladder biopsies are an essential diagnostic step in evaluating urinary tract symptoms or confirming a bladder cancer diagnosis.
2. Why is a Bladder Biopsy Done?
A bladder biopsy is recommended when your doctor suspects abnormalities in the bladder lining based on your symptoms or test results. Common reasons include:
-
Blood in urine (hematuria): Persistent or unexplained blood in urine may signal an infection, inflammation, or bladder tumor.
-
Abnormal cystoscopy findings: If your doctor notices irregular growths, patches, or lesions during cystoscopy, a biopsy helps determine their nature.
-
Recurring urinary tract infections (UTIs): Frequent infections may indicate underlying tissue damage or chronic inflammation.
-
Unusual urine cytology results: If urine tests show abnormal or cancerous cells, a biopsy confirms the diagnosis.
-
Suspected bladder cancer: A biopsy helps identify the type, grade, and stage of cancer.
In short, it provides a definitive diagnosis that guides further treatment and management.
3. How is a Bladder Biopsy Performed?
A bladder biopsy is generally done as an outpatient procedure, meaning you can go home the same day. Here's what happens step-by-step:
-
Preparation:
-
You may be asked to avoid eating or drinking for a few hours before the procedure.
-
A urine sample might be collected to rule out infection.
-
You'll receive either local anesthesia (numbing only the bladder area) or general anesthesia (you'll be asleep).
-
-
During the Procedure:
-
The doctor inserts a cystoscope through the urethra into the bladder.
-
Saline solution is used to fill the bladder, making it easier to see the bladder walls.
-
The doctor carefully inspects the bladder and removes small tissue samples using special instruments attached to the cystoscope.
-
-
After the Procedure:
-
The tissue samples are sent to a lab for microscopic analysis.
-
The entire process usually takes 15 to 30 minutes.
-
You'll be observed for a short while before being allowed to go home.
-
4. Is a Bladder Biopsy Painful?
Most patients experience minimal discomfort during the biopsy. If local anesthesia is used, you may feel a mild burning sensation or pressure when the cystoscope is inserted. After the procedure, it's normal to experience:
-
Mild burning during urination
-
A small amount of blood in the urine
-
Increased urge to urinate
These symptoms usually disappear within 24 to 48 hours. Drinking plenty
of water can help flush out the bladder and ease discomfort.
If you experience severe pain, heavy bleeding, or fever, contact your
doctor immediately.
5. What Should I Expect After the Procedure?
Recovery from a bladder biopsy is typically quick. You can go home the same day and resume light activities. However, doctors often recommend:
-
Drink plenty of fluids to flush your bladder.
-
Avoid heavy lifting or strenuous activity for a few days.
-
Avoid sexual intercourse for about 48 hours or as advised.
-
Take prescribed medications such as antibiotics to prevent infection.
You might notice pinkish urine or slight burning when urinating - this is normal. If bleeding persists or worsens, seek medical help.
6. What Are the Risks and Possible Complications?
Bladder biopsies are considered safe, but like all surgical procedures, they carry a small risk of complications. These may include:
-
Urinary tract infection (UTI): Caused by bacteria entering the bladder.
-
Bleeding (hematuria): Light bleeding is common, but heavy bleeding is rare.
-
Bladder perforation: Extremely rare, but possible if the bladder wall is thin or fragile.
-
Difficulty urinating: Temporary swelling can make it hard to pass urine.
To minimize risks, follow your doctor's instructions closely and complete any prescribed antibiotics.
7. How Long Does It Take to Get the Results?
Typically, it takes 5 to 10 days to receive bladder biopsy results. The pathology lab will examine the tissue and prepare a detailed report, which your doctor will review with you.
The report may describe:
-
Normal findings: No signs of disease.
-
Inflammatory changes: Indicating infection or irritation.
-
Precancerous or cancerous cells: Suggesting bladder cancer or carcinoma in situ (early-stage cancer).
Your doctor will then discuss treatment options or next steps based on the findings.
8. What Do Abnormal Biopsy Results Mean?
Abnormal biopsy results may reveal one of the following conditions:
-
Bladder Cancer: Presence of malignant cells in the bladder lining.
-
Carcinoma in situ (CIS): Early-stage cancer confined to the inner lining.
-
Papillomas or benign growths: Non-cancerous tumors that may require monitoring.
-
Chronic cystitis: Persistent bladder inflammation due to infection or autoimmune disorders.
-
Interstitial cystitis: A painful bladder condition with chronic inflammation but no infection.
Your doctor will create a personalized treatment plan that could involve medication, surgery, or follow-up cystoscopies.
9. How Should I Prepare for a Bladder Biopsy?
Preparation is simple and depends on the type of anesthesia used. Your doctor may advise:
-
Avoid eating or drinking for 6 to 8 hours if general anesthesia is planned.
-
Stop taking blood thinners or anticoagulants several days before the procedure (with doctor approval).
-
Arrange for someone to drive you home after the biopsy.
-
Inform your doctor about all medications and allergies you have.
Proper preparation ensures a smooth and safe procedure.
10. When Should I Call My Doctor After the Procedure?
While minor discomfort is normal, you should contact your doctor immediately if you experience:
-
Heavy bleeding or large blood clots in urine
-
Fever above 101°F (38.3°C)
-
Severe pain in the lower abdomen or back
-
Inability to urinate
-
Signs of infection such as chills or cloudy urine
Prompt attention helps prevent complications and ensures proper recovery.


