Introduction to Bladder Neck Incision
The bladder neck is the region where the urinary bladder meets the urethra (in men typically via the prostatic urethra). When that region becomes narrowed or obstructed, a surgical procedure known as a bladder neck incision (BNI) may be used to relieve the obstruction and restore more normal urinary flow.
In BNI, small cuts or incisions are made in the fibromuscular tissue at the bladder outlet (neck) via an endoscopic instrument passed through the urethra, thereby widening the channel and facilitating urine passage.
This procedure is often considered when less invasive treatments (such as medications or dilation) have been insufficient, particularly in cases of bladder-neck stenosis or contracture, or following prior prostate surgery or other causes of narrowing.
It is minimally invasive, typically done under general or spinal anaesthesia, and recovery is relatively quick compared with more extensive open surgery.
The goal is to improve urinary stream, reduce urinary symptoms (such as hesitancy, weak flow or incomplete emptying), and prevent complications of obstruction (like bladder damage or kidney back-pressure).
Causes and Risk Factors of Bladder Neck Incision
Here we discuss why a bladder-neck incision becomes necessary - i.e., what underlying causes and risk factors lead to bladder-neck obstruction, stenosis, or the need for the operation.
Underlying causes:
-
Bladder neck stenosis/contracture: Scarring at the bladder neck (where the bladder joins the urethra) that narrows the passage. This may result from prior prostate surgery (e.g., Transurethral Resection of the Prostate (TURP), radical prostatectomy) or radiation therapy.
-
Benign prostatic obstruction (BPO) or small prostate with tight bladder-neck: Some men with smaller glands may nonetheless have a high bladder-outlet resistance at the bladder neck and benefit from a BNI rather than full prostate resection.
-
Prior instrumentation or catheterisation: Repeated catheter insertion, prior bladder neck instrumentation can lead to scar and narrowing.
-
Radiation therapy: Pelvic/radiation therapy for prostate cancer can cause fibrosis and narrowing at the bladder neck.
Risk factors:
-
Age: Older men are more likely to develop prostate-related changes and bladder-neck obstruction.
-
Prior prostate surgery or interventions: Any prior endoscopic/ablative prostate procedure raises risk of bladder neck scarring/stenosis.
-
Radiation or prostate cancer treatment: These therapies may predispose to contracture formation.
-
Presence of urinary obstruction symptoms over time (weak stream, incomplete emptying) without treatment may lead to bladder neck damage/stenosis.
Understanding these causes and risk factors helps clinicians identify patients who may benefit from BNI and enables patients to recognise when obstruction symptoms warrant evaluation.
Symptoms and Signs that Indicate Need for Bladder Neck Incision
This section describes what patients typically experience when bladder-neck obstruction is present and BNI may be appropriate.
Common symptoms and signs:
-
Weak urinary stream or slow flow: Difficulty initiating and sustaining a good flow of urine.
-
Straining to void, "hesitancy": Need to push or wait before urine starts.
-
Intermittent stream: Urine starts and stops rather than a smooth flow.
-
Nocturia: Frequent need to urinate at night.
-
Incomplete bladder emptying/unable to empty fully: Sensation that bladder remains partly full, or measurable residual urine.
-
Urgency/frequency, possibly urinary leakage (sometimes from high pressure or overflow).
-
Urinary retention: In severe cases, inability to pass urine, needing catheterisation.
Signs the clinician may observe:
-
Elevated post-void residual urine (on bladder scan)
-
Slowed flow on uroflowmetry
-
Findings of bladder wall thickening or diverticula from chronic obstruction
-
Cystoscopic evidence of narrowing/scarring at bladder-neck / outlet
When such symptoms persist and other treatments (medications, lifestyle) do not suffice, the urologist may assess for bladder-neck obstruction and consider BNI.
Diagnosis of Bladder Neck Obstruction and Suitability for Bladder Neck Incision
Before proceeding to a bladder neck incision, an accurate diagnosis and selection of suitable patients is essential. This section covers evaluation steps.
Pre-operative assessment:
-
History and physical examination: Assess symptoms (flow changes, retention, nocturia), prior surgeries/interventions, radiation history.
-
Urinalysis/urine culture: Rule out infection or other causes of urinary symptoms.
-
Uroflowmetry: Measure urine flow rate and pattern (low peak flow may indicate obstruction).
-
Post-void residual (PVR) measurement: Bladder scan to see how much urine remains after voiding.
-
Imaging or ultrasound: Assess bladder wall thickness, possible diverticula, kidney changes.
-
Cystoscopy: Direct visualization of the bladder neck and urethra to identify narrowing/stenosis or other pathology.
-
Urodynamics (sometimes): In complex cases, to differentiate bladder muscle issues vs outlet obstruction.
Determining suitability for BNI:
-
Confirmed bladder-neck obstruction (narrowing) rather than another cause of symptoms (e.g., bladder muscle weakness, neurological bladder).
-
No active urinary tract infection.
-
General health sufficient to undergo anaesthesia and surgery.
-
Discussion of alternative treatments (medication, observation) and informed consent about risks/benefits.
What the procedure involves (brief overview):
-
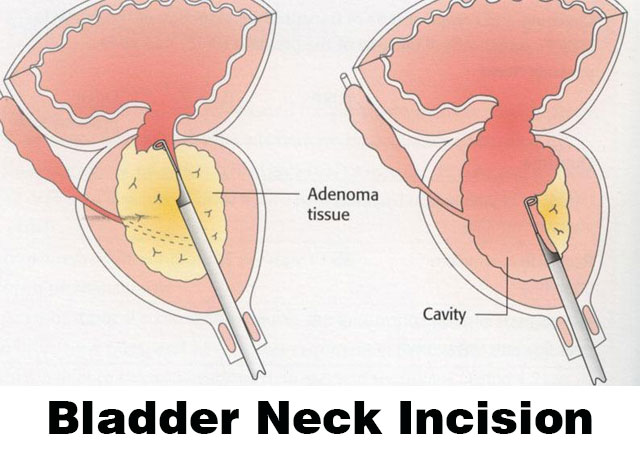
Under general or spinal anaesthesia, the surgeon passes a resectoscope (a telescope via the urethra) into the bladder.
-
Small incisions are made through the bladder-neck (often at 5- and 7-o'clock or bilateral) using a cautery loop or laser fibre, to widen the outlet.
-
A catheter is inserted post-procedure to assist bladder drainage and prevent clotting/irritation.
A well-selected patient with confirmed bladder-neck obstruction can expect significant relief of symptoms after BNI.
Treatment Options: Bladder Neck Incision and Beyond
This section covers the BNI procedure itself, what it offers, alternatives, recovery and what to expect.
Bladder Neck Incision (BNI) - the procedure in detail
-
Typically performed under general or spinal anaesthesia.
-
No skin incision: access is via urethra using a resectoscope.
-
Incisions are made in the bladder neck (and sometimes adjacent prostate tissue) to widen the passage. A thin wire-loop, laser fibre or cautery instrument is used.
-
At the end of the procedure, a catheter is placed; bladder irrigation may be used if there is bleeding.
-
The typical hospital stay is 1-2 days, with catheter removed once urine clears and flow is adequate.
Post-operative care & recovery
-
Expect urine to be blood-tinged for 24-48 hours; burning/urgency may occur.
-
Most men can resume light activities after a few days; full recovery may take up to 4 weeks.
-
Follow-up with urologist to assess symptoms, flow, PVR; monitoring for possible recurrence of obstruction.
Success rate & outcomes
-
Studies show high short-term success (improved flow, symptom relief). One life-table analysis reported that only ~17 % and ~12 % of unilateral and bilateral incisions needed re-operation within 6 years.
-
Recent study for bladder-neck contracture (BNC) found 82 % patency after one endoscopic incision and 94 % after two, using balloon dilation + incision.
Alternatives / adjuncts
-
Medications (alpha-blockers, 5-alpha reductase inhibitors) to relieve outlet obstruction or reduce prostate size - may be preferred in milder cases.
-
Observation with periodic monitoring if symptoms are mild and kidneys not involved.
-
More extensive surgery (e.g., prostate resection or reconstruction) if BNI not sufficient or if large prostate, prior radiation etc.
-
Adjunctive treatments in recurrent stenosis: intralesional injections (e.g., mitomycin C) have been explored.
In summary: For men with confirmed bladder-neck obstruction, BNI is a targeted, effective, minimally invasive option with good outcomes and relatively short recovery. Choosing between BNI and alternatives depends on individual anatomy, prior interventions, prostate size, and overall health.
Prevention and Management of Bladder Neck Issues
Although BNI treats the problem of obstruction, it's also valuable to focus on prevention (where applicable) and management of the underlying condition to reduce recurrence or complications.
Prevention of bladder-neck obstruction or contracture
-
Avoid unnecessary urethral instrumentation (reduce trauma to bladder neck/urethra).
-
Care in prostate surgery: post-operative monitoring and timely management of early bladder-neck narrowing may prevent severe contracture later.
-
Prompt treatment of urinary tract infection or bladder outlet obstruction to prevent secondary damage/scarring of bladder neck.
-
Lifestyle modifications: maintaining healthy weight, avoiding bladder irritants, managing comorbidities (e.g., diabetes, high blood pressure) that may compromise bladder/drainage function.
Post-procedure management to optimise outcome
-
Ensure adequate hydration, avoid bladder irritants (caffeine, alcohol) for a short period post-surgery to reduce bladder irritation.
-
Follow-up visits per urologist's schedule: flow tests, PVR, imaging if needed to detect recurrence of narrowing early.
-
Monitor for symptoms of recurrence: slow stream, increased frequency, incomplete emptying. Early detection means less invasive treatment.
-
Maintain general urologic health: good voiding habits, avoid urinary retention, treat infections early.
By combining procedural treatment with good preventive and management practices, patients maximise the benefit of BNI and minimise risk of re-obstruction.
Complications of Bladder Neck Incision
While BNI is generally safe, like all surgical procedures it carries potential risks and complications. It's important patients are informed.
Common and expected complications
-
Blood in urine (haematuria) for a short time after surgery.
-
Burning on urination, urgency, frequency in the early recovery phase.
Less common but important complications
-
Retrograde ejaculation (semen entering the bladder instead of exiting during orgasm) - occurs because the incision may affect the internal sphincter mechanism. One leaflet describes ≈ 4 out of 10 men may experience this.
-
Urinary incontinence: either temporary or rarely persistent, especially if bladder control mechanisms are affected.
-
Re-narrowing (recurrence of stenosis/contracture): Scar tissue may reform and cause re-obstruction, sometimes requiring repeat intervention.
-
Injury to surrounding structures, e.g., urethra, bladder neck, bladder wall perforation (rare).
-
Post-operative infection, clot retention, need for catheter longer than anticipated.
When to seek immediate medical attention
-
Persistent heavy bleeding or large clots in urine.
-
Signs of infection: fever, chills, cloudy or foul urine, burning pain that worsens.
-
Inability to pass urine post-procedure (urinary retention).
-
New onset severe pain, swelling, or sudden incontinence.
By being aware of possible complications, patients can promptly seek help, which improves outcomes.
Living with the Condition (Before & After Bladder Neck Incision)
This section highlights how patients can manage their condition and their life around the procedure - both pre- and post-BNI - and what to expect in terms of quality of life, follow-up, and long-term outlook.
Before surgery
-
If you have urinary symptoms (weak stream, nocturia, incomplete emptying) discuss with your urologist: early evaluation may lead to less invasive interventions.
-
Prepare for surgery: optimise health (quit smoking, control comorbidities), follow pre-operative instructions (fasting, medication review).
-
Understand the procedure: ask your urologist about expected benefits, risks (especially retrograde ejaculation, recurrence risk), recovery period.
After the BNI procedure
-
Recovery: Many men can resume light activities in 3-5 days; full recovery may take 4 weeks.
-
Post-operative urinary symptoms (urgency, frequency, blood-tinged urine) are common and usually improve.
-
Sexual/ejaculatory changes: Discuss this pre-operatively. Retrograde ejaculation is common; fertility may be affected if you desire children.
-
Follow-up: Regular check-ups with urologist, flow/urine measurements, imaging if needed. Early detection of recurrence means less invasive retreatment.
-
Lifestyle: Maintain healthy voiding habits, avoid bladder irritants, hydrate well, manage comorbidities (e.g., diabetes).
-
Mental health & expectations: Many men experience significant symptom relief and improved quality of life, but for those with prior radiation or multiple prior surgeries, some limitations may persist.
Long-term outlook
-
Good outcome: Many patients achieve improved urinary flow and symptom relief. For example, long-term studies show low re-operation rate (~12-17 %) in selected patients for many years.
-
Recurrence possible: Especially in cases with prior radiation, prior repeated procedures, or severe scar tissue. You may require additional treatment or monitoring.
-
Quality of life: By reducing obstruction, improving bladder emptying and reducing nocturia/frequency, BNI can significantly improve daily life, sleep, and reduce complications (kidney damage, stones, infections) that occur from chronic obstruction.
Tips for patients living with BNI outcome
-
Keep a urinary symptom diary: track flow, frequency, any hesitancy or retention.
-
Avoid holding urine too long; aim to void routinely.
-
Stay on top of any urinary tract infections; treat promptly.
-
Maintain communication with your urologist: if you notice symptoms returning, don't wait - early assessment helps.
-
Engage in healthy lifestyle: good hydration, avoid excess alcohol/caffeine, maintain healthy weight, stay active - all help bladder health.
Top 10 Frequently Asked Questions about Bladder Neck Incision (BNI)
1. What is a Bladder Neck Incision (BNI)?
A Bladder Neck Incision (BNI) is a minimally invasive surgical procedure performed to treat bladder outlet obstruction, a condition where the bladder neck (the junction between the bladder and urethra) becomes narrow and restricts urine flow.
During the procedure, a surgeon uses a resectoscope (a thin telescope-like instrument) inserted through the urethra to make one or more small incisions at the bladder neck. This helps relax and widen the passage, allowing urine to flow freely from the bladder.
BNI is commonly performed in men with bladder neck obstruction, often following prostate surgery or due to scarring, but it can also be done in women with bladder outlet obstruction due to congenital or post-surgical narrowing.
2. Why is a Bladder Neck Incision Needed?
Your doctor may recommend a BNI if you are experiencing symptoms caused by obstruction of urine flow. Common reasons include:
-
Difficulty starting urination (hesitancy)
-
Weak or intermittent urine stream
-
Incomplete bladder emptying
-
Frequent urination, especially at night (nocturia)
-
Urinary retention or recurrent urinary tract infections (UTIs)
BNI is often used to treat primary bladder neck obstruction, post-prostate surgery scarring, or urethral narrowing that cannot be corrected through medication alone.
3. How is a Bladder Neck Incision Performed?
BNI is a minimally invasive, endoscopic surgery performed under general or spinal anesthesia. The steps usually include:
-
Insertion of the resectoscope: A small instrument is passed through the urethra into the bladder.
-
Visualization: The surgeon examines the bladder neck and prostate area using a camera attached to the scope.
-
Incision: One or two small cuts are made in the bladder neck using a tiny electric current or laser to widen the passage.
-
Drainage: A catheter is placed in the bladder at the end of the procedure to allow urine drainage while the area heals.
The entire procedure usually takes 20 to 30 minutes, and most patients go home the same day or after an overnight stay.
4. Is a Bladder Neck Incision the Same as TURP (Transurethral Resection of the Prostate)?
No - while both procedures are performed using similar instruments, they are not the same.
-
BNI involves making small incisions in the bladder neck to relieve obstruction without removing tissue.
-
TURP, on the other hand, involves cutting and removing part of the prostate gland to relieve blockage caused by prostate enlargement (BPH).
BNI is preferred when the obstruction is at the bladder neck rather than within the prostate itself, especially in younger men or those with small prostates.
5. What Should I Expect After a Bladder Neck Incision?
After the procedure, a urinary catheter is usually left in place for 12-24 hours to help the bladder drain. Once removed, you may experience:
-
Mild burning or stinging during urination
-
A frequent urge to urinate
-
A small amount of blood in the urine
These symptoms are temporary and typically resolve within a few days.
You will be advised to drink plenty of water, avoid strenuous
activity, and refrain from sexual intercourse for about 2
weeks to allow healing.
6. What Are the Benefits of a Bladder Neck Incision?
The primary benefits of BNI include:
-
Improved urine flow and bladder emptying
-
Relief from urinary symptoms such as frequency, urgency, and nocturia
-
Reduced risk of urinary retention and infections
-
Quick recovery and minimal hospital stay
-
Lower risk of complications compared to open surgery
Most patients notice significant improvement in symptoms within a few days to a week after the procedure.
7. What Are the Possible Risks or Complications?
Although BNI is a safe and effective procedure, some risks may occur, including:
-
Urinary tract infection (UTI)
-
Temporary blood in urine (hematuria)
-
Retrograde ejaculation (semen enters the bladder instead of exiting through the urethra - harmless but may affect fertility)
-
Stricture formation or scarring (rare)
-
Temporary urinary incontinence
Serious complications are uncommon when performed by an experienced urologist.
8. How Long Does It Take to Recover from a Bladder Neck Incision?
Most patients recover quickly and can return to normal daily activities within
3-5 days.
However, complete healing of the bladder neck may take 4 to 6 weeks.
During this time, you should:
-
Avoid lifting heavy objects or exercising strenuously
-
Refrain from alcohol or caffeine (as they irritate the bladder)
-
Drink plenty of fluids to flush out the urinary system
-
Attend follow-up visits for check-ups and urine flow tests
Your doctor will let you know when it's safe to resume sexual activity and full physical activity.
9. Will I Need the Procedure Again?
In most cases, BNI provides long-term relief, but in a small number of patients, scar tissue can form again, leading to recurrent obstruction.
If this happens, a repeat BNI or other minimally invasive procedure may be required. Regular follow-up with your urologist helps detect any recurrence early.
10. What Are the Long-Term Outcomes After Bladder Neck Incision?
The results of BNI are generally excellent. Most patients experience:
-
Improved urine flow
-
Reduced urinary frequency and urgency
-
Enhanced bladder emptying
-
Better quality of life
While retrograde ejaculation may occur in some men, sexual function and erections are usually not affected. With proper follow-up and lifestyle adjustments, the benefits of BNI can last for many years.


