Introduction to Burr Hole Aspiration
A burr-hole aspiration (or burr-hole drainage/aspiration) is a neurosurgical procedure in which a small hole (a "burr hole") is drilled into the skull to gain access to the intracranial space and evacuate a fluid or blood collection (for example a subdural hematoma, epidural hematoma, or other intracranial bleed) or relieve pressure in the cranial vault. According to the Johns Hopkins Medicine website, burr holes are used "to help relieve pressure on the brain when fluid, such as blood, builds up and starts to compress brain tissue."
The aim of this blog content is to provide a patient- and clinician-friendly yet medically accurate overview of the causes, risks, symptoms/signs, diagnosis, treatment options (including when burr-hole aspiration is indicated), prevention/management, complications, and living with the condition before and after the procedure.
In many cases, burr-hole aspiration is a less-invasive alternative to larger skull surgeries (craniotomy) for selected patients and conditions. For instance, for chronic subdural hematomas, a single burr hole plus drainage may suffice. However, it remains a significant neurosurgical intervention with important risks, and appropriate patient selection and post-operative care are vital.
Causes and Risk of Burr Hole Aspiration
Here we distinguish between why the procedure is needed (i.e., the underlying cause of the intracranial collection) and who is at higher risk of needing such a procedure.
Underlying causes
Some of the common indications for burr-hole aspiration include:
-
Accumulation of blood between the dura and skull (e.g., acute or chronic subdural hematoma) due to head injury, anticoagulation, or spontaneous bleeding.
-
Epidural hematoma (blood between skull and dura) causing mass effect/raised intracranial pressure.
-
Intracranial hemorrhage or intraparenchymal hemorrhage in select cases where minimally invasive evacuation (via burr hole + catheter/aspiration) is feasible.
-
Cerebral abscess or pus collection within the skull which needs drainage (burr holes may be part of the approach) but less common.
-
Hydrocephalus / placement of shunts / access to ventricles in some neurosurgical contexts—but those are somewhat separate but still involve burr holes.
Risk factors
Factors that increase the risk of developing an intracranial collection that might require burr-hole drainage include:
-
Advanced age (especially for chronic subdural hematomas) due to cerebral atrophy, fragile bridging veins.
-
Head trauma (even minor trauma in the elderly) leading to bleeding under the dura.
-
Use of anticoagulant or antiplatelet medications which predispose to spontaneous or delayed bleeding.
-
Cerebral atrophy, or conditions causing increased vulnerability of cerebral vessels.
-
Coagulopathy or bleeding disorders.
-
Neurosurgical comorbidities: e.g., prior craniotomy, shunt placements, previous hemorrhages.
-
Delayed diagnosis (especially of chronic subdural hematoma) leading to progressive accumulation and need for intervention.
-
Poor monitoring or delayed presentation in resource-limited settings (some literature discusses emergency burr hole by non-neurosurgeons in remote settings)
In essence, burr-hole aspiration is not a disease itself, but a treatment for intracranial collections; thus the "cause and risk" section focuses on the conditions that trigger the need for this procedure.
Symptoms and Signs of Burr Hole Aspiration
Since the burr-hole aspiration is performed because of an intracranial collection/pressure, this section covers the symptoms and signs of the underlying condition (e.g., hematoma) that lead to the surgery.
Common symptoms
Patients may present with:
-
Headache (often progressive or worsening)
-
Nausea and vomiting (due to raised intracranial pressure)
-
Altered level of consciousness: confusion, drowsiness, lethargy, even coma in severe cases
-
Focal neurological deficits: weakness on one side of the body, speech difficulty, visual disturbances
-
Seizures (especially with subdural hematomas)
-
In older patients, more subtle symptoms: personality change, gait disturbance, falls, memory problems (especially with chronic subdural hematomas)
Clinical signs
-
On examination: signs of raised intracranial pressure (papilledema, pupillary changes)
-
Focal deficits: e.g., hemiparesis, dysphasia
-
In acute extradural hematoma: "lucid interval" may be followed by rapid decompensation and fixed dilated pupils.
-
Radiologic signs (on CT/MRI): presence of a hematoma, midline shift, effacement of ventricles, compression of cortical structures. Diagnostic imaging is key (see next section).
-
In chronic cases: may see signs of chronic blood collection with minimal acute symptoms but slowly progressive signs.
It's important in your article to emphasise that any of these signs/symptoms warrant urgent neurosurgical evaluation, and once imaging shows a collection causing mass effect, the option of burr-hole aspiration may be discussed.
Diagnosis of Burr Hole For Aspiration
In this section, outline how the decision for burr-hole aspiration is made: clinical assessment + imaging + surgical decision-making.
Clinical assessment
-
Detailed history: onset, progression of symptoms, any trauma event (even minor head injury), medications (anticoagulants/antiplatelets), prior neurosurgical history.
-
Neurological examination: assess level of consciousness (Glasgow Coma Scale), focal deficits, signs of increased intracranial pressure.
-
Assessment of risk/fitness for surgery (general medical condition, comorbidities, age).
Imaging and investigations
-
Non-contrast CT scan of the head is the first-line imaging for suspected intracranial hemorrhage/hematoma. It can rapidly show blood, mass effect, midline shift, subdural vs epidural vs intraparenchymal location.
-
MRI may be used in certain chronic/complex cases for better delineation.
-
In chronic subdural hematoma, CT may show a hypodense or isodense crescentic collection under the dura.
-
Intraoperative imaging or sonography may be used in minimally invasive approaches. For example, ultrasound-guided burr-hole aspiration of spontaneous intracerebral hemorrhage has been studied.
-
Pre-operative labs: coagulation profile, platelet count, full blood count, renal/liver function, etc to assess surgical risk and reversal of anticoagulation if needed.
-
Intra-operative/neuro-navigation considerations: planning of burr-hole site based on imaging, ensuring safe access and drain placement. The procedure is targeted rather than exploratory.
Surgical decision-making (Indications for burr-hole aspiration)
-
The decision to proceed with burr-hole aspiration depends on: size of hematoma/collection, mass effect (e.g., midline shift), neurological deficits, patient's general condition, and the anatomical location of the collection (e.g., is it accessible by burr hole vs requiring craniotomy).
-
For example, one article states: "A small craniotomy with evacuation … and simple aspiration via burr hole are methods of decompression when appropriate."
-
In chronic subdural hematoma with minimal surgical risk and a favourable anatomy, burr-hole + drainage may be preferred.
-
Contraindications or caution: large solid clots, inaccessible location, need for vascular repair, unstable patient requiring more extensive surgery.
For your blog, you might include a table comparing when burr-hole aspiration is suitable vs when more extensive surgical intervention (craniotomy) is needed.
Treatment Options of Burr Hole Aspiration
Here we cover both non-surgical/conservative (if any) and surgical options - emphasising that the burr-hole aspiration is a surgical option but alternatives exist or adjuncts are needed.
Non-surgical / Conservative management
While many intracranial hemorrhages require surgery, in particular patients or small collections, conservative management may be considered (observation, reversal of anticoagulation, medical therapy). However, delayed or progressive collections often require surgery. For chronic subdural hematoma, in selected cases with minimal symptoms and small collections, observation may be feasible. Your blog should note this.
Surgical treatment - Burr-Hole Aspiration / Drainage
This is the core section focused on the procedure:
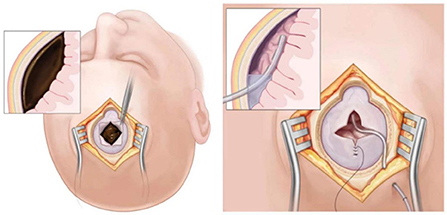
What the procedure involves
-
A small incision is made in the scalp at a planned location.
-
A burr hole is drilled through the skull (typically using a perforator drill).
-
The dura is opened and the hematoma/collection is evacuated/aspirated (sometimes using irrigation and suction/catheter). For chronic subdural hematomas, sometimes a drain is left in place for 24-48 hours.
-
The incision is closed. The patient is monitored in hospital (often ICU or neurosurgical ward).
Advantages and limitations
-
Advantage: less invasive compared to a full craniotomy; quicker recovery in selected patients; short operative time.
-
Limitations: may not be sufficient if the clot is thick/solid (vs liquid), if there's a large intraparenchymal hemorrhage, or if vascular pathology needs repair. Some literature points out that "simple aspiration … doesn't always allow the surgeon to drain the hematoma completely."
Variations / adjuncts
-
Drain placement after burr hole to reduce recurrence in chronic subdural hematoma.
-
Endoscopic assistance or image-guided catheter aspiration for intraparenchymal hemorrhages via burr hole.
-
Minimally invasive stereotactic evacuation techniques (future/under research) but may be supplementary to burr-hole access.
Post-operative care
-
Monitoring for neurological improvement/decline, imaging to assess residual collection or shift.
-
Management of drains (if used) and removal when appropriate.
-
Rehabilitation, prevention of seizures as needed, control of underlying bleeding risk (e.g., reversal of anticoagulants, management of hypertension).
Outcomes
-
For chronic subdural hematomas, burr-hole drainage has been shown to be effective with good outcomes in many cases.
-
However, recurrence remains an issue; residual collection or re-bleeding may require repeat surgery.
-
Patient-specific factors (age, medical comorbidities) impact prognosis significantly.
In your content you can break this section into sub-headings like "When is burr-hole aspiration the right choice?", "What happens during the procedure?", "What are the different techniques/variations?", and "What to expect afterwards?".
Prevention and Management of Burr Hole Aspiration
This covers (a) prevention of the underlying condition that leads to burr-hole aspiration (i.e., prevention of hematomas) and (b) management (medical and lifestyle) around the procedure.
Prevention of intracranial collections requiring burr hole
While you cannot prevent all cases (especially spontaneous ones), risk-reducing measures include:
-
Prevent head injuries: Use of helmets, fall prevention especially in elderly, safe driving.
-
Management of anticoagulant/antiplatelet therapy: Regular monitoring, ensuring correct dosing, reversal when indicated (especially before trauma or after minor head injury).
-
Control of hypertension, vascular disease, and other risk factors for intracranial bleeding.
-
In elderly individuals with brain atrophy, vigilance after even mild head trauma for signs of subdural hematoma. Early imaging helps.
-
Ensuring good neurosurgical/trauma system access so that delayed diagnosis doesn't lead to large collections.
Management around the procedure
-
Pre-operative management: Optimize medical comorbidities (e.g., hypertension, diabetes), reverse anticoagulation if safe/appropriate, evaluate for coagulopathy.
-
Post-operative care: Monitor intracranial pressure, neurological status; manage drains; prevent infection (antibiotics if indicated), prevent seizures (anticonvulsants as per neurosurgeon's decision).
-
Rehabilitation and follow-up: Physical therapy/occupational therapy if deficits are present; neurorehabilitation in cases of significant injury.
-
Lifestyle adaptation: Avoiding activities that may precipitate bleeding until stabilized; falling precautions; adherence to neurologist/neurosurgeon instructions.
-
Long-term monitoring: Imaging follow-up to detect recurrence of collection; monitoring of anticoagulation/antiplatelet therapy if still indicated.
In your blog you might provide a "pre- and post-procedure" checklist for patients and caregivers.
Complications of Burr Hole Aspiration
It's vital to inform about risks and potential complications so patients and caregivers have realistic expectations and consent is properly informed.
Common and less serious complications
-
Residual hematoma or incomplete evacuation, potentially requiring repeat surgery.
-
Infection (wound infection, intracranial infection)
-
Bleeding or re-bleed at the burr hole site
-
Seizures (especially if brain tissue was irritated)
-
Temporary neurological deficits (which may improve)
Serious or rare complications
-
Intracerebral hemorrhage or intraventricular hemorrhage after burr hole drainage (rare but reported)
-
Brainstem hemorrhage after burr-hole drainage (extremely rare)
-
Subdural/epidural hematoma formation or re-accumulation of blood in unexpected area.
-
Brain injury due to surgery (damage to brain tissue, bleeding)
-
Anesthesia risks (in older/medically compromised patients)
-
Mortality risk (especially in older patients, those with large intracranial hemorrhage, comorbidities)
-
Neurological sequelae: persistent deficits, cognitive impairment, gait disturbance, chronic headache
Prognosis post-complications
-
Many complications are manageable with timely recognition (e.g., drain repositioning, antibiotics for infection, anticonvulsants for seizure)
-
However patient outcomes vary significantly: older age, larger initial hematoma, delayed intervention all worsen prognosis.
-
Recurrence of collection in chronic subdural hematoma may require repeat surgery and is a known risk factor.
Including a short table of complication rates (if available) or risk stratification would be helpful for your audience.
Living with the Condition of Burr Hole Aspiration
In this section you address life before and after the procedure: what patients/caregivers should know, how to adapt, what to expect.
Before the procedure (living with intracranial collection)
-
If a patient is diagnosed with a hematoma and a burr-hole procedure is being planned (or if they are in observation), they may experience headaches, cognitive changes, gait problems, and neurological deficits. It's important to provide support and monitoring (frequent check-ups, imaging)
-
Educate the patient and family about signs of deterioration (increasing headache, vomiting, weakness, seizure) so that prompt evaluation happens.
After the procedure
-
Recovery timeline: Many patients recover well if the collection is evacuated early and there were minimal deficits. However, older patients or those who had major deficits may need longer rehabilitation.
-
Hospital stay and follow-up: Typically a few days to a week depending on the case, then outpatient follow-up with neurosurgeon/neuro-rehabilitation.
-
Rehabilitation: Physical therapy (for gait, strength), occupational therapy (for activities of daily living), possibly speech therapy if speech/cognition was affected.
-
Returning to normal life: Gradual return — avoiding high-risk activities (contact sports, falls) until cleared.
-
Medications/lifestyle: If the patient is on anticoagulants/antiplatelets, a neurosurgical/neurology team will coordinate when/if to resume; lifestyle modifications (fall prevention, helmet use if indicated) remain important.
-
Long-term monitoring: There may be a risk of recurrence (especially in chronic subdural hematoma). Symptoms such as headache or cognitive/gait change should trigger evaluation.
-
Emotional/psychological support: Any neurosurgical intervention can be life-changing; some patients may experience anxiety, depression, or cognitive changes — referral to counselling or neuro-psychologist may help.
Patient education & adherence
-
Educate patients and caregivers on signs of recurrence (headache, confusion, weakness)
-
Ensure adherence to follow-up imaging and clinic visits
-
Explain realistic outcomes: While many patients recover well, some may have residual deficits and require ongoing support
-
Emphasise the importance of fall prevention (especially in elderly), safe medication use (especially anticoagulants), and general brain health (control hypertension, diabetes, avoid smoking).
You might include a "what to expect after your burr-hole evacuation" box or FAQ section.
Top 10 Frequently Asked Questions about Burr Hole for Aspiration
1. What is a Burr Hole for Aspiration?
A burr hole for aspiration is a neurosurgical procedure
used to treat conditions that cause abnormal accumulation of fluid, blood, or pus inside
the skull.
In this procedure, the surgeon drills a small circular opening (burr
hole) in the skull to drain (aspirate) substances such as:
-
Blood (in cases of chronic subdural hematoma)
-
Pus (from a brain abscess)
-
Cerebrospinal fluid (in cases of hydrocephalus)
This minimally invasive approach helps relieve pressure on the brain (intracranial pressure) and restore normal neurological function.
2. When is a Burr Hole Aspiration Needed?
Doctors recommend a burr hole aspiration when there is increased intracranial pressure caused by trapped fluid or bleeding that cannot be managed with medication alone.
Common conditions include:
-
Chronic subdural hematoma (SDH): Blood accumulation between the brain and its covering membrane.
-
Brain abscess: A pocket of infection that needs drainage.
-
Hydrocephalus: Excess cerebrospinal fluid buildup.
-
Epidural abscess or empyema: Infection causing pus formation.
This procedure is often life-saving, especially when symptoms like headache, vomiting, confusion, or weakness appear suddenly.
3. How is the Burr Hole Aspiration Procedure Performed?
The procedure is usually done under local or general anesthesia by a
neurosurgeon.
Steps typically include:
-
Positioning and sterilization: The patient's head is positioned, shaved, and cleaned.
-
Incision and drilling: A small incision is made in the scalp, and a burr hole is drilled into the skull.
-
Aspiration: The accumulated blood, pus, or fluid is gently drained using a syringe or suction device.
-
Irrigation: The cavity may be flushed with saline to prevent infection.
-
Closure: The incision is sutured, and a sterile dressing is applied.
In some cases, a drain tube is left in place temporarily to ensure complete fluid removal.
4. What Are the Benefits of Burr Hole for Aspiration?
Burr hole aspiration provides several clinical benefits, such as:
-
Rapid reduction of intracranial pressure
-
Immediate relief of symptoms like headache, drowsiness, and confusion
-
Minimally invasive surgery with small incisions
-
Shorter recovery time compared to craniotomy
-
Effective management of blood clots, abscesses, and fluid buildup
-
Lower complication rate when performed promptly by an experienced neurosurgeon
5. How Long Does the Surgery Take and What is the Recovery Time?
The burr hole procedure usually takes 30 to 90 minutes, depending on the cause and complexity.
Recovery Timeline:
-
Hospital stay: 2-5 days (may vary by condition)
-
Return to daily activities: 2-4 weeks
-
Full recovery: Around 4-6 weeks, depending on overall health
Patients who undergo burr hole aspiration for chronic subdural hematoma typically recover faster than those treated for infections like abscesses.
6. What Are the Possible Risks and Complications?
Although considered a safe neurosurgical procedure, burr hole aspiration carries some risks, including:
-
Bleeding or hematoma recurrence
-
Infection (meningitis or abscess)
-
Seizures
-
Brain swelling
-
Neurological deficits (rare)
-
CSF leakage or wound complications
Strict postoperative care and sterile surgical technique greatly reduce these risks.
7. What Happens After the Surgery? (Postoperative Care)
After the procedure, patients are closely monitored in the ICU or recovery unit. Postoperative care typically includes:
-
Neurological assessments (to check brain function and reflexes)
-
Antibiotics or anti-seizure medications (to prevent infection or convulsions)
-
Imaging (CT or MRI scans) to confirm successful drainage
-
Fluid and nutrition management
-
Gradual mobilization once stable
If a drain is inserted, it is usually removed within 24-48 hours once drainage decreases.
8. What Are the Signs That You Might Need This Procedure Urgently?
You may require an urgent burr hole aspiration if you develop sudden symptoms of brain compression or infection, such as:
-
Severe, persistent headache
-
Vomiting or nausea
-
Loss of consciousness or drowsiness
-
Seizures
-
Weakness or paralysis on one side of the body
-
Vision or speech problems
-
High fever (in case of abscess or infection)
Early medical evaluation and imaging (CT/MRI) can be lifesaving in these scenarios.
9. What is the Success Rate of Burr Hole Aspiration?
The success rate of burr hole aspiration is very high — approximately 85% to 95%, depending on the underlying condition and the patient's general health.
-
For chronic subdural hematoma, recurrence rates are low when proper drainage is achieved.
-
For brain abscesses, combining aspiration with antibiotic therapy ensures effective cure.
Timely surgery and proper postoperative monitoring are key to excellent recovery outcomes.
10. How Can I Prevent Conditions That Lead to Burr Hole Aspiration?
While not all causes are preventable, several measures can reduce the risk of conditions requiring this surgery:
-
Avoid head injuries by wearing helmets and seatbelts.
-
Treat infections promptly to prevent brain abscess formation.
-
Control chronic diseases such as diabetes or hypertension.
-
Avoid blood thinners misuse, which can increase bleeding risk.
-
Regular medical checkups if you've had a prior head injury or surgery.
Maintaining a healthy lifestyle and following your doctor's advice can significantly lower your risk of developing brain pressure complications.


