Introduction to Burr Hole Surgery
In neurosurgery, "burr hole surgery" refers to a procedure in which a small hole (often dime-sized) is drilled into the skull to access the brain beneath. The primary goal is typically to relieve pressure on the brain - for example when fluid or blood has accumulated between brain coverings or in the skull cavity.
Because the brain is enclosed within the rigid skull, any extra fluid (blood, pus, cerebrospinal fluid) can raise intracranial pressure, compress brain tissue, impair perfusion and lead to serious neurologic damage or death. Burr holes provide a relatively less-invasive access point compared to a full craniotomy (removing a larger bone flap).
This procedure is used in a number of clinical situations: acute or chronic subdural hematoma, epidural hematoma, hydrocephalus, brain abscesses, placement of shunts or monitoring devices.
In this article, we will explore what causes the need for burr hole surgery, how patients present, how it is diagnosed, the treatment options (including the procedure itself), prevention/management where relevant, possible complications, and how patients live with the condition afterwards.
Causes and Risk of Burr Hole Surgery
Burr hole surgery is primarily performed to relieve pressure on the brain caused by fluid accumulation, such as blood or cerebrospinal fluid, and carries risks including infection, bleeding, and neurological complications. The procedure is commonly used for conditions like subdural hematomas, epidural hematomas, and hydrocephalus, and while less invasive than craniotomy, it still involves significant potential complications.
Why the procedure becomes necessary
The "cause" of burr hole surgery is not the surgery itself but the underlying condition that necessitates it. Some of the most common indications include:
-
A Chronic Subdural Hematoma (CSH) - where blood slowly accumulates beneath the dura (outer brain covering) over days to weeks, often after mild head injury, particularly in older adults or those taking anticoagulants.
-
An acute subdural or Epidural Hematoma - where bleeding is more rapid, often from traumatic injury.
-
Hydrocephalus or elevated intracranial pressure requiring drainage of cerebrospinal fluid (CSF) or insertion of shunts/catheters via burr holes.
-
Brain abscesses or collections of pus around the meninges (meningitis with loculated collections) requiring drainage.
-
Brain tumor biopsy or placement of monitoring electrodes/devices - burr holes may serve as access points.
Risk factors for needing the procedure
Certain factors increase the likelihood that someone might develop a condition that necessitates burr hole surgery:
-
Age (older adults have more brain atrophy → more space for blood to accumulate slowly)
-
Use of anticoagulant or antiplatelet medications (increasing risk of bleeding)
-
Head trauma (falls, sports injuries, motor vehicle accidents)
-
Alcohol abuse (which can cause brain atrophy, impaired healing, increased bleed risk)
-
Bleeding disorders (e.g., hemophilia) or other medical conditions that weaken blood vessels.
Risks associated with the surgery
As with any neurosurgical intervention, burr hole surgery carries risks (and these become part of the "risk of Burr Hole Surgery" topic). Risks include bleeding, infection, clot formation, brain injury, anesthesia complications, and possibly need for further, more extensive surgery.
Symptoms and Signs of Burr Hole Surgery
Since burr hole surgery is a treatment rather than a disease, this section refers to the symptoms and signs of underlying conditions that lead to the procedure, and also what signs may occur that suggest something has gone wrong post-surgery.
Symptoms of underlying condition
When blood or fluid builds up around the brain, typical symptoms include:
-
Headache (often worsening, persistent)
-
Confusion or change in mental status (especially in older adults)
-
Seizures or new onset fits (blood irritates cortex)
-
Weakness or numbness on one side of body (hemiparesis)
-
Drowsiness, decreased level of consciousness, even coma if pressure is very high.
-
In older, chronic cases: mild gait disturbance, personality change, fall risk.
Signs of the surgery/monitoring that something may require the surgery
In surgical or postoperative context, signs that burr hole drainage might be in process:
-
On imaging: accumulation of blood under the skull (subdural/epidural hematoma) → visible on CT/MRI.
-
Clinical deterioration after head injury: enlarging pupil, hemiplegia, rapid drop in GCS (Glasgow Coma Scale) → suggesting pressure build-up.
Postoperative signs and monitoring
After the procedure, the surgical & intensive care team will watch for:
-
Head wound site: signs of bleeding, swelling, infection
-
Neurologic status: improvement of pre-operative deficits or signs of new deficits
-
Intracranial pressure signs: headache, vomiting, confusion, new seizures
-
General post-op complications: fever, wound drainage, CSF leak, DVT/PE (deep-vein thrombosis/pulmonary embolism) as neurosurgical patients are at risk.
Diagnosis of Burr Hole Surgery
Diagnosis for burr hole surgery involves identifying intracranial conditions that cause elevated brain pressure or space-occupying lesions such as hematomas or fluid collections. The diagnosis is made through a combination of clinical evaluation, imaging studies, and neurological assessment to determine if decompression or drainage is necessary.
Medical history & physical exam
A clinician will take a detailed history: head trauma or falls, anticoagulant use, progressive symptoms of headache/confusion/weakness. Physical neurological exam will check for focal deficits, signs of increased intracranial pressure (papilloedema on ophthalmologic exam), altered consciousness.
Imaging studies
Imaging is essential to detect fluid/blood accumulation, assess size, location, and guide surgical planning. Typical studies:
-
Non-contrast CT scan of the head: excellent for detecting acute blood, subdural/epidural hematoma.
-
MRI may be used for more detailed anatomy, chronic subdural hematoma, or if tumour/abscess suspected.
-
In some cases, CT/MR + contrast to examine for a brain abscess or tumour.
Pre-operative assessment & planning
Once imaging confirms a space-occupying lesion (blood, fluid), the neurosurgical
team reviews location, thickness, potential brain shift, and decides whether
burr hole drainage is appropriate or whether a craniotomy is needed (for larger
clot, firm organized hematoma).
Additional assessments:
-
Laboratory tests: coagulation profile, platelet count, blood type, cross-match if bleeding risk.
-
Medical optimization: control of blood pressure, reversal of anticoagulants (if safe), ensure no active infection, anesthesia fitness.
Decision-making algorithm
Essentially, the decision to proceed with a burr hole procedure depends on:
-
Size and location of the hematoma/fluid collection
-
Presence of neurological deficits and rate of deterioration
-
Patient's overall condition (age, comorbidities)
-
Whether the hematoma is chronic (liquid) vs acute with thick clot (may need open surgery)
Treatment Options of Burr Hole Surgery
Treatment for burr hole surgery involves carefully planned surgical intervention to drain fluid, relieve brain pressure, or access brain tissue for diagnostic or therapeutic purposes. It is a minimally invasive neurosurgical technique used for subdural hematoma, hydrocephalus, brain abscesses, and related conditions.
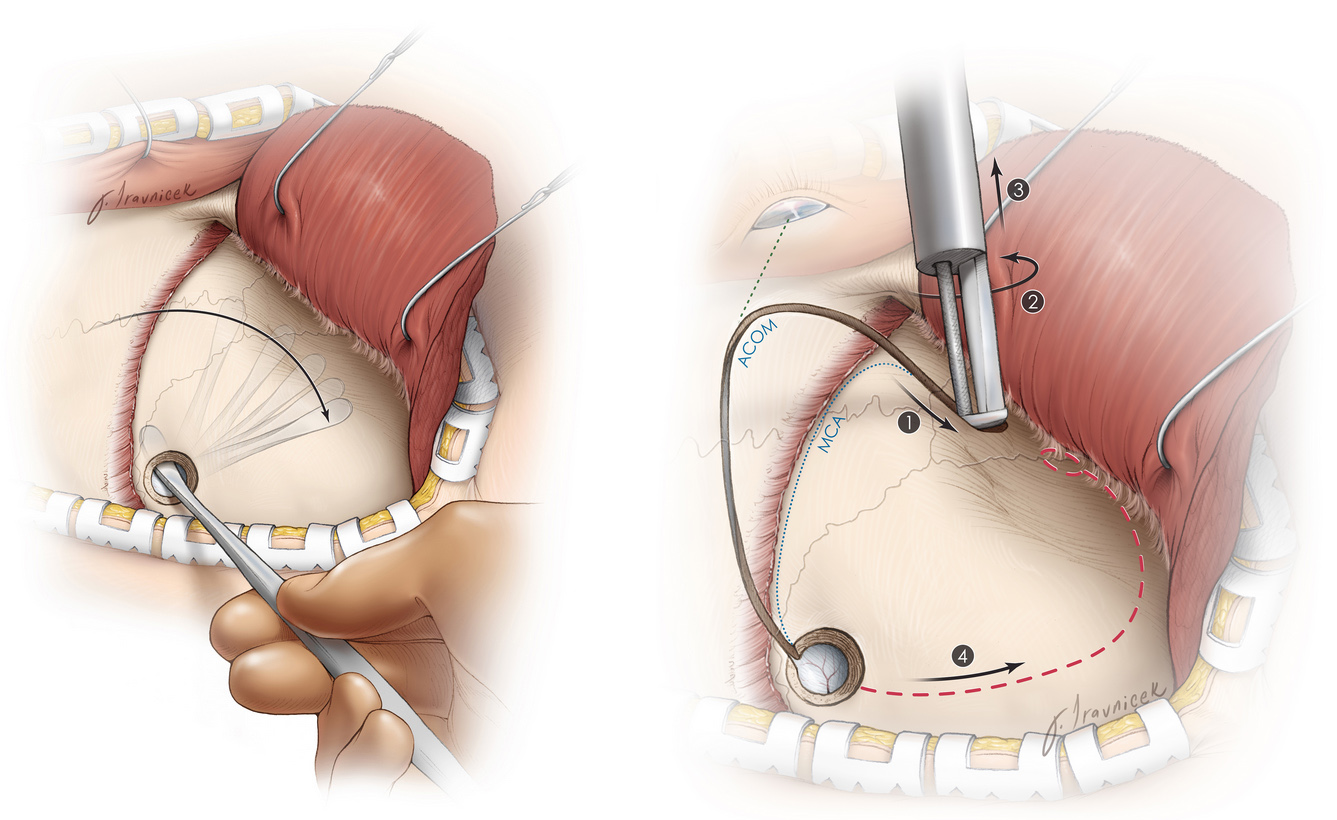
The burr hole procedure
Here is a typical sequence of the procedure:
-
The patient is placed under general anaesthesia (sometimes local anaesthesia with sedation in well-selected cases).
-
The scalp is shaved (or hair trimmed) and cleaned with antiseptic solution.
-
A small incision is made in the scalp, the skull bone is exposed. A special drill creates one or more burr holes into the skull (often sized ~dime-size).
-
The dura (outer meningeal layer) is opened, and the fluid or blood is drained. A thin tube or drain may be placed to continue drainage over 24-48 hours.
-
The incision is closed, and the patient transferred to recovery/ICU for monitoring.
Alternative or adjunct treatments
-
In cases where burr hole is insufficient (e.g., thick clotted hematoma), a more extensive procedure - Craniotomy - may be required.
-
Endoscopic variations: burr holes may be used as entry points for endoscopic procedures (for example, endoscopic third ventriculostomy) in hydrocephalus.
-
Conservative monitoring: if hematoma is small, asymptomatic, the neurosurgeon may monitor and delay surgery.
-
Adjunctive therapies: management of raised intracranial pressure, reversal of anticoagulation, seizure prophylaxis, rehabilitation.
-
Emerging techniques: for example, in chronic subdural hematoma, combining burr hole drainage with middle meningeal artery embolization has been explored.
Postoperative care
-
Monitoring vital signs, neurologic status, wound site
-
Pain management (scalp pain, discomfort)
-
Avoidance of head trauma, strict bed rest may be advised for 1-2 days (especially with drains)
-
Imaging (repeat CT) may be performed post-operatively to ensure adequate evacuation and no recurrence.
Prevention and Management of Burr Hole Surgery
Burr hole surgery is a minimally invasive neurosurgical technique primarily used to drain chronic subdural hematoma (CSDH) or relieve elevated intracranial pressure. Its prevention and management focus on surgical precision, minimizing recurrence, infection control, and optimizing healing postoperatively.
Prevention
-
Fall prevention, especially in older adults: minimize tripping hazards, use assistive devices, manage vision and balance issues.
-
Control anticoagulant/antiplatelet medications carefully; ensure regular monitoring, and when trauma risk is high, evaluate benefit vs risk.
-
Limit excessive alcohol use (a factor for brain atrophy and bleed risk).
-
Protective head gear in high-risk activities (sports, biking, construction).
-
Manage high blood pressure, vascular disease, and bleeding disorders with care.
-
In patients with known subdural collections, regular follow-up and imaging may detect progression before requiring surgery.
Long-term management
-
After surgery, rehabilitation may be needed for neurologic deficits (physical therapy, occupational therapy, speech therapy if applicable).
-
Monitoring for recurrence: especially in chronic subdural hematoma, recurrence risk is meaningful and follow-up imaging may be required.
-
Lifestyle modifications: avoiding head injuries, wearing helmet when indicated, avoiding heavy lifting/straining early post-op.
-
Medical optimization: controlling comorbidities (diabetes, hypertension), ensuring good nutrition and bone health (skull healing).
-
Patient and caregiver education: recognizing symptoms of recurrence (headache, confusion, weakness) so that early medical attention can be sought.
Complications of Burr Hole Surgery
Complications of burr hole surgery can involve both surgical and medical issues, ranging from mild infections to severe intracranial hemorrhage or postoperative recurrence. A 2025 cohort analysis from the Karolinska University Hospital and other recent studies provide a clear picture of modern complication rates and management strategies.
Intra- and post-operative complications
-
Bleeding (re-accumulation of hematoma, hemorrhage) - particularly if the underlying bleed source remains or if coagulopathy is present.
-
Infection (wound infection, meningitis, brain abscess) - given that the skull has been penetrated and a drain may be used.
-
Brain injury: unintentional damage to brain tissue or blood vessels during drilling or drainage.
-
Seizures: new onset seizures may be triggered by brain manipulation or residual irritative tissue.
-
Cerebrospinal fluid (CSF) leak or subdural air (pneumocephalus) - especially if drains or irrigation are used.
-
Recurrence of the hematoma or fluid collection - particularly in chronic cases.
-
General surgical/anesthesia risks: DVT/PE, heart attack, stroke, pulmonary complications.
Long-term issues
-
Residual neurologic deficits (depending on pre-operative brain injury severity)
-
Cognitive impairment or personality change (especially in older patients)
-
Post-operative headache or scalp pain
-
Cosmetic issues: hair loss or scar at incision site
-
Need for further surgeries if recurrence occurs
It is important that patients and families receive thorough counselling on these risks before the procedure and that postoperative care is vigilant to detect early complications.
Living with the Condition of Burr Hole Surgery
Living after burr hole surgery usually involves a gradual recovery phase that focuses on physical healing, neurological stabilization, and lifestyle adjustments to prevent future complications. Most patients regain normal function within weeks, although recovery speed depends on age, underlying condition, and overall health.
Recovery and rehabilitation
-
Most patients will spend a few days in hospital after the procedure - often in intensive care or high-dependency unit if neurological issues were significant.
-
The length of hospital stay and recovery largely depend on: the severity of the hematoma/fluid prior to surgery, the patient's baseline health, presence of neurologic deficits, and whether additional surgery (craniotomy) was needed.
-
After discharge, rehabilitation may include: physical therapy (for weakness or gait problems), occupational therapy (fine motor/ADL skills), speech therapy (if language or swallowing affected).
-
Patients may need to restrict certain activities (no heavy lifting, no head trauma / sports) for a period of time as advised by the neurosurgeon.
Lifestyle and follow-up
-
Regular follow-up with neurosurgeon and neurologist; imaging may be scheduled to monitor for recurrence especially in chronic subdural hematoma.
-
Avoidance of future head injuries: wearing helmet, fall precautions for elderly, careful with anticoagulants/antiplatelets under physician supervision.
-
Effective management of comorbidities: hypertension, diabetes, anticoagulation, alcohol use, etc to reduce further risk.
-
Cognitive and psychological support: patients may undergo mood or memory changes after brain surgery; counselling may help.
-
Gradual resumption of normal life: driving, working, sports must be cleared by physician; usually after neurologic status stabilises and imaging is satisfactory.
Prognosis
-
Many patients who undergo burr hole drainage for hematomas improve markedly, especially if the procedure is done timely before irreversible brain damage.
-
The outcome depends on: how quickly the hematoma was treated, how much brain compression occurred, patient's age and comorbidities.
-
In chronic cases with minimal deficits, patients may return to near-normal life; in more severe cases, ongoing residual deficits may persist and need long-term care or adaptive devices.
When to seek medical attention
Patients/caregivers should watch for:
-
New or worsening headache
-
New confusion, changes in behaviour or consciousness
-
New weakness or numbness
-
Seizure (first time or recurrence)
-
Persistent wound redness, swelling, drainage or fever (signs of infection)
-
Any fall or head trauma after surgery - immediate medical review is warranted
Top 10 Frequently Asked Questions about Burr Hole Surgery
1. What is Burr Hole Surgery and Why is it Done?
Burr hole surgery is a minimally invasive neurosurgical procedure in which a small circular hole (called a "burr hole") is drilled into the skull using a specialized surgical tool. This procedure gives surgeons access to the brain without performing a full craniotomy (which involves removing a large portion of the skull).
It is primarily done to drain accumulated blood, pus, or cerebrospinal fluid and to relieve intracranial pressure. Common conditions treated with burr hole surgery include:
-
Chronic Subdural Hematoma: Blood accumulation between the brain surface and skull due to trauma or aging.
-
Brain Abscess: A collection of pus caused by bacterial or fungal infection.
-
Hydrocephalus: A buildup of cerebrospinal fluid (CSF) in the brain's ventricles.
-
Severe Head Injury: To relieve pressure from bleeding or swelling.
-
Diagnostic Procedures: In some cases, it helps in biopsy or electrode placement for brain monitoring.
This surgery is often lifesaving and provides immediate relief from brain compression symptoms such as headaches, confusion, drowsiness, or weakness.
2. How is Burr Hole Surgery Performed?
The procedure is usually performed under local or general anesthesia, depending on the patient's condition and the reason for surgery.
Here's a step-by-step overview of the process:
-
Preparation: The patient's head is shaved and cleaned to maintain a sterile surgical field.
-
Anesthesia: Local anesthesia numbs the scalp area, while general anesthesia may be used for complex or emergency cases.
-
Incision and Drilling: The surgeon makes a small incision in the scalp and drills one or more holes in the skull using a high-speed surgical drill.
-
Drainage or Access: The underlying fluid, blood clot, or pus is carefully drained through the burr hole. In some cases, a catheter or drain is left in place for continuous drainage.
-
Closure: The incision is closed with sutures or staples, and a dressing is applied to protect the site.
The surgery typically lasts between one to two hours and is often performed using imaging guidance such as CT or MRI scans to ensure accuracy and safety.
3. What Are the Indications for Burr Hole Surgery?
Doctors recommend burr hole surgery when there is a need to reduce intracranial pressure or to access the brain without performing a more invasive procedure. Common indications include:
-
Subdural Hematoma (acute or chronic) - caused by head injury or aging blood vessels.
-
Epidural or Intracerebral Hemorrhage - when drainage can prevent further brain damage.
-
Brain Abscess - to drain infected pus and prevent spread of infection.
-
Hydrocephalus - to insert shunts that help drain excess CSF.
-
Diagnostic Use - to obtain brain tissue samples or insert electrodes for monitoring seizures.
The choice of burr hole surgery depends on imaging results, patient stability, and the neurosurgeon's judgment.
4. What Are the Benefits of Burr Hole Surgery?
Burr hole surgery offers several advantages compared to more invasive brain surgeries:
-
Minimally Invasive: Only small holes are drilled, reducing surgical trauma.
-
Faster Recovery: Patients usually recover within days rather than weeks.
-
Effective Pressure Relief: Rapidly alleviates brain compression and associated symptoms.
-
Reduced Risk of Complications: Less blood loss and lower infection rates compared to open craniotomy.
-
Shorter Hospital Stay: Many patients are discharged within a few days post-surgery.
Because it is a targeted and precise procedure, it can often be performed on elderly or high-risk patients safely.
5. What Are the Risks or Complications of Burr Hole Surgery?
Although burr hole surgery is considered safe, it carries some risks like all surgical procedures. Potential complications include:
-
Bleeding or Recurrent Hematoma: The blood clot can sometimes reaccumulate.
-
Infection: Wound or intracranial infection, though rare, can occur.
-
Seizures: Post-operative seizures may happen in some patients.
-
Brain Swelling or Damage: Minimal risk if performed by experienced surgeons.
-
Neurological Deficits: Temporary weakness, confusion, or speech difficulties may occur post-surgery.
-
Scarring or Cosmetic Concerns: Minimal due to the small incision size.
Surgeons take all necessary precautions, including antibiotic prophylaxis and careful post-operative monitoring, to minimize these risks.
6. What is the Recovery Process Like After Burr Hole Surgery?
Recovery depends on the patient's age, overall health, and underlying condition. Here's what the typical recovery process involves:
-
Hospital Stay: Most patients remain hospitalized for 2-7 days.
-
Observation: Doctors monitor neurological function, drainage output, and signs of infection.
-
Pain Management: Mild headaches or discomfort are common and easily managed with medication.
-
Wound Care: The incision area should be kept clean and dry until fully healed.
-
Rehabilitation: Some patients may need physical therapy or occupational therapy if neurological symptoms persist.
Full recovery can take a few weeks to a couple of months, depending on the severity of the initial condition.
7. What Should Patients Expect After Discharge?
After being discharged, patients should:
-
Avoid strenuous physical activities for several weeks.
-
Keep the surgical site clean and dry.
-
Take prescribed antibiotics and painkillers as directed.
-
Attend regular follow-up appointments for neurological assessments.
-
Watch for warning signs such as fever, severe headache, vomiting, drowsiness, confusion, or seizure—these may require immediate medical attention.
Doctors usually perform a follow-up CT or MRI scan to ensure the brain has returned to normal and no new bleeding has occurred.
8. Can Burr Hole Surgery Be Performed as an Emergency Procedure?
Yes. Burr hole surgery is often performed in emergency situations, particularly when
there is acute bleeding or a rapidly expanding hematoma that causes
severe pressure on the brain.
In such cases, the goal is to immediately relieve intracranial pressure
and prevent irreversible brain damage. Emergency burr hole procedures can be lifesaving,
especially after head trauma or sudden neurological deterioration.
9. Is Burr Hole Surgery a Permanent Solution?
For most patients, burr hole surgery provides long-term relief and complete recovery. However, the outcome depends on the cause of the pressure buildup:
-
Chronic Subdural Hematoma: Often successfully treated with a single procedure, though recurrence can occur in about 5-10% of cases.
-
Hydrocephalus: May require additional procedures or permanent shunt placement.
-
Brain Abscess: Requires follow-up antibiotic therapy to ensure full resolution.
Regular monitoring and imaging help ensure the problem does not recur.
10. What is the Success Rate of Burr Hole Surgery?
Burr hole surgery is highly successful, particularly when performed by skilled
neurosurgeons and when the underlying cause is diagnosed early.
The success rate is typically over 90%, especially for chronic subdural
hematoma cases. Most patients experience a dramatic improvement in symptoms such as
headaches, confusion, or weakness within a few days.


