Introduction to Caesarean Section
A caesarean section (C-section) is the surgical delivery of a baby by making incisions in the mother's abdomen (laparotomy) and uterus (hysterotomy) rather than vaginal delivery. Historically, C-sections were performed only when the mother was dying or already dead; nowadays, improvements in surgical techniques, anaesthesia and obstetric care have made the procedure much safer.
In many contexts the C-section has become one of the most common major surgical procedures during childbirth. From a public-health perspective, the role of C-section is two-fold: it can be life-saving when indicated (for mother and/or baby) and yet it also carries risks and costs, especially when used unnecessarily.
Global patterns show an increase in C-section rates in both low-income and high-income settings. For example, the World Health Organization (WHO) notes that while the procedure can be essential in certain obstetric complications, rates above a certain threshold do not appear to yield additional benefits in terms of maternal or neonatal mortality.
Because of this duality - lifesaving versus potentially over-used - it is important for pregnant women and their families, and for healthcare providers, to understand when a C-section is indicated, the risks and benefits, what the surgery involves, how to manage recovery, and how to plan for future pregnancies. This article will explore causes and risks, symptoms/signs (of indications and of post-operative state), diagnosis/decision-making, treatment/surgery, prevention management, complications, and living with/post C-section care.
Causes and Risk of Caesarean Section
A caesarean section (C-section) is a major surgical intervention used to deliver a baby through an incision made in the mother's lower abdomen and uterus. Although it is generally safe when medically indicated, the procedure carries both short-term and long-term risks. Its causes can be medical, obstetric, or elective in nature.
Indications (When a C-section may be required)
A C-section is generally indicated when a vaginal delivery would pose a greater risk than a surgical delivery to the mother, the baby, or both. Some of the common situations include:
-
Fetal distress: If the baby's heart rate shows signs of compromise, or if there is umbilical cord prolapse or other cord/placental issues.
-
Labour not progressing (dystocia): For example, poor cervical dilation or failure of descent of the fetal head despite adequate contractions.
-
Abnormal fetal presentation: Breech (baby buttocks or feet first), transverse lie, or when multiple pregnancies complicate vaginal delivery.
-
Placental abnormalities: Placenta praevia (placenta covering the cervix), placental abruption (early separation), placenta accreta spectrum in future pregnancies.
-
Maternal health conditions: Severe pre-eclampsia/eclampsia, uncontrolled hypertension, maternal infections (e.g., active genital herpes at time of labour), prior classical uterine incision, or other contraindications to vaginal birth.
-
Previous C-section: In some cases, if the previous uterine incision or other factors make a repeat C-section the safer option.
Risk Factors and Trends
Beyond strictly medical indications, there are risk-factors and systemic/societal dynamics that influence C-section. For example:
-
Advanced maternal age, higher body mass index (BMI), assisted reproductive technologies, and comorbidities such as diabetes and hypertension increase the likelihood of needing a C-section.
-
Institutional and provider factors: Some hospitals or providers have higher C-section rates due to scheduling convenience, fears of litigation, declining skills in vaginal birth (especially complex deliveries) or non-clinical drivers.
-
According to WHO, while increasing C-section rates up to about 10 % of births is associated with reductions in maternal and newborn mortality, beyond that threshold there is no clear evidence of further benefit in mortality terms.
Risks Associated with C-Section
While C-section can be safety-enhancing when indicated, it is still major surgery with associated risks:
-
For the mother: greater blood loss, risk of infection, slower recovery, longer hospital stay, risk in future pregnancies (e.g., abnormal placentation, uterine rupture)
-
For the baby: In elective C-section (especially before onset of labour) baby may have higher risk of respiratory distress, delayed breastfeeding, and other neonatal transitions.
-
For health systems: High rates of C-section that are not clinically indicated may increase cost and burden without commensurate improvement in outcomes.
In summary: A C-section is often a necessary, potentially lifesaving procedure when indicated - but the decision to perform one should always balance the benefits versus risks, and non-clinical drivers of C-section should be addressed.
Symptoms and Signs of Caesarean Section
Recovering from a caesarean section (C-section) is a gradual process that involves physical healing, hormonal adjustment, and emotional adaptation. Since it is a major abdominal surgery, recovery may take up to six weeks or more, depending on the mother's health, surgical outcome, and the presence of any complications.
3.1 Indications / Warning Signs During Labour
These are conditions or observations that may trigger the decision for C-section:
-
Labour that is not progressing: After membranes have ruptured, if despite adequate uterine contractions there is no cervical change or fetal descent for a defined period (for example: ≥ 6 cm dilation with ruptured membranes and ≥ 4 hours of adequate contractions with no change)
-
Second stage arrest: Prolonged second stage of labour (e.g., beyond 2 h in multiparous or 3 h in nulliparous women under regional anaesthesia) may indicate need for intervention.
-
Non-reassuring fetal heart rate tracings (fetal distress) or other signs of fetal compromise.
-
Maternal compromise: e.g., severe hypertensive crisis, uncontrolled bleeding, acute infection, or maternal exhaustion.
-
Malpresentation of the fetus (breech, transverse lie), placenta/cord issues (placental previa, abruption, cord prolapse) - these may be identified via examination/ultrasound and lead to decision for C-section.
3.2 Signs and Symptoms After Caesarean Section (Post-operative period)
After the surgery, the mother and baby should be monitored and the mother should be aware of common (normal) and warning signs (abnormal). Typical postoperative signs:
-
Normal: Pain at incision site (expected), uterine cramping as the uterus contracts back, some vaginal bleeding (lochia), fatigue (due to surgery + childbirth), difficulty mobilising initially.
-
Abnormal / Warning signs:
-
Fever (suggesting infection)
-
Redness, swelling, discharge at incision site (wound infection or dehiscence)
-
Increasing pain or pain that does not improve, heavy bleeding (postpartum haemorrhage)
-
Leg swelling, pain in calf or thigh, or chest pain/breathlessness (suggestive of deep vein thrombosis or pulmonary embolism)
-
Signs of bladder or bowel injury (rare) - e.g., inability to pass urine, persistent abdominal pain, distension
-
Delayed return of bowel function (if prolonged) or signs of ileus/obstruction (nausea, vomiting, distension)
-
Patient education and early recognition of these warning signs is critical for timely intervention.
Diagnosis of Caesarean Section
The diagnosis of a Caesarean Section (C-section) is not about detecting a disease, but rather identifying medical or obstetric conditions in which vaginal delivery poses a risk to the mother or baby. Diagnosis includes clinical evaluation, maternal and fetal assessments, laboratory tests, and imaging techniques to determine whether a C-section is required and how it should be performed.
4.1 Assessment of Indications
The obstetric team assesses the mother and fetus to determine if a C-section is indicated. This involves:
-
Maternal history: obstetric history (prior surgeries, previous C-section(s)), comorbidities (e.g., hypertension, diabetes, cardiac disease), obstetric complications (placenta previa, abruption), fertility treatments.
-
Fetal assessment: ultrasound for fetal presentation (head-first, breech, transverse), estimated fetal weight, amniotic fluid volume, placental location, cord issues.
-
Labour assessment: cervical dilation, membrane status (ruptured or intact), uterine contraction adequacy, fetal descent, maternal and fetal vital signs, monitoring of fetal heart rate patterns.
-
Classification of urgency: Many institutions use an urgency classification for C-section (e.g., Category 1 for immediate threat to life, Category 2 for maternal/fetal compromise but not immediate threat) which helps guide decision-to-delivery interval. (See guideline sources for further details.)
4.2 Pre-operative Evaluation and Preparation
Once a decision is made (or is being considered), the preparatory phase includes:
-
Laboratory tests: Complete blood count (haemoglobin/platelets), blood type & cross-match, coagulation profile if indicated, screening for infections (HIV/Hepatitis), antibody screen.
-
Anaesthesia assessment: Evaluate maternal airway, co-morbidities, plan for regional (spinal/epidural) vs general anaesthesia.
-
Consent: Discussion of risks and benefits of the C-section vs alternative (if feasible), discussion of potential complications, recovery expectations. For example, in elective C-section on maternal request, guidance recommends thorough counselling.
-
Surgical planning: Decide incision type (skin and uterine), presence of previous uterine scars, plan for haemorrhage risk, known placenta/adhesion issues. Guidelines for intraoperative technique have been updated recently.
-
Timing: Ensure optimal timing (e.g., in elective cases after 39 weeks gestation if no other indication) to reduce neonatal risks.
-
Pre-operative prophylaxis: Administer antibiotics (ideally before skin incision) to reduce maternal infection risk; thromboprophylaxis should be considered due to combined pregnancy + surgery risk.
4.3 Decision-making and Shared Discussion
Important in the process is shared decision-making: the obstetrician should discuss with the woman (and family) about risks/benefits, possible alternatives, prospects for recovery, implications for future pregnancies. For elective C-section on maternal request (without maternal/fetal indication), guidelines recommend a vaginal delivery plan is safe and appropriate unless other factors exist.
In summary: Diagnosis in this context is about evaluation and decision-making rather than a typical “disease diagnosis”. The process ensures that the correct indication exists, the patient is optimally prepared, and potential risks mitigated.
Treatment Options of Caesarean Section
The treatment of a Caesarean Section involves performing surgical delivery through a carefully controlled operative technique, supported by preoperative preparation, intraoperative management, and postoperative care. The objective is to safeguard both mother and baby while minimizing complications.
5.1 When and How the Surgery Is Performed
-
Elective vs Emergency: Elective (planned) C-sections are scheduled in advance (for example, for placenta praevia, prior classical uterine incision, known malpresentation). Emergency C-sections occur when a complication arises during labour or pregnancy requiring immediate delivery.
-
Anaesthesia: Typically, regional anaesthesia (spinal or epidural) is used so the mother is awake but numbed from the waist down. General anaesthesia may be required in emergencies or when regional is contraindicated.
-
Surgical technique (overview):
-
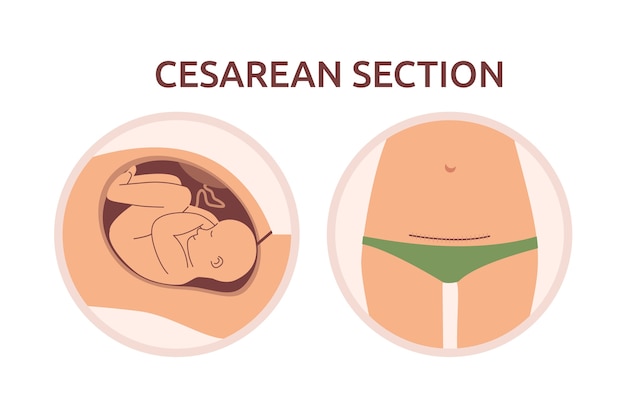
Skin incision (most commonly low transverse “bikini” incision) → abdominal wall opened → bladder flap formed, lower uterine segment exposed.
-
Uterine incision (usually low transverse) → baby delivered → placenta removed → uterine incision closed (single-layer or double-layer depending on setting).
-
Abdominal wall closure: peritoneum may or may not be closed (evidence shows non-closure can reduce operating time and analgesic requirements)
-
-
Recent guidelines for intraoperative and postoperative care (ERAS protocols) are being updated (see article from 2025).
5.2 Postoperative Care
-
Immediate care: Monitoring of vital signs (maternal and fetal), bleeding, urine output, pain control, mobilisation (early walking), catheter removal (often within 12-24 hours if regional anaesthesia used).
-
Antibiotics and infection prevention: Prophylactic antibiotics given before skin incision reduce risk of maternal wound/uterine infection.
-
Thromboprophylaxis: Because pregnancy and surgery both increase risk for venous thromboembolism, prophylaxis (compression stockings, mobilisation, low-molecular-weight heparin if indicated) is recommended.
-
Early feeding and mobilisation: Rather than extended bed rest, early mobilisation and oral intake are encouraged when safe, as these improve recovery.
5.3 Alternatives / Considerations for Future Pregnancies
-
Vaginal Birth After Caesarean (VBAC): For women who have had a previous C-section, a planned attempt at vaginal delivery (trial of labour after caesarean - TOLAC) may be possible if conditions are favourable (e.g., prior low transverse uterine incision, no contraindications). This offers reduced risks of repeated surgery, but must be weighed against risk of uterine rupture etc.
-
Elective C-section on maternal request: Some women request C-section even without medical indication. Professional bodies recommend thorough counselling; for example, in absence of other indications, delivery should not be scheduled before 39 weeks gestation.
-
Shared decision-making: In all cases, the discussion should include risks/benefits for mother and baby, implications for future pregnancies, recovery, and the possibility of choosing a vaginal approach when safe.
5.4 Summary of Treatment Flow
-
Indication identified → 2. Pre-operative preparation → 3. Surgical procedure → 4. Post-operative care and recovery support → 5. Planning for discharge and future pregnancies.
The overall aim is to ensure safety, minimise complications, enable early recovery, promote mother-baby bonding (skin-to-skin, breastfeeding) and support the mother physically and emotionally.
Prevention and Management of Caesarean Section
Prevention and management of a Caesarean Section (C-section) focus on minimizing unnecessary surgical births, reducing postoperative complications, and ensuring rapid maternal recovery through evidence-based clinical practices. These include preoperative optimization, intraoperative safety protocols, and enhanced postoperative recovery strategies guided by current global standards.
6.1 Preventing Unnecessary C-Sections
-
Improve labour management: For example, guidelines suggest recognising that early labour (latent phase) does not always require intervention; active labour may be defined at dilation of ~6 cm. Arrest of labour at earlier dilation may lead to unnecessary C-section.
-
Institutional quality-improvement strategies: For instance, the AIM-bundle (5 R's: Readiness; Recognition & Prevention; Response; Reporting & Systems Learning; Respectful, Equitable & Supportive Care) to safely reduce primary caesarean birth.
-
Non-clinical interventions: According to WHO, addressing drivers of unnecessary C-sections (women's and providers' preferences, fear, convenience, organisational incentives) is key.
-
Education and informed choice: Empowering women with information about benefits/risks of vaginal vs C-section, and supporting vaginal birth when safe, may reduce C-sections on demand.
-
Monitoring and audit: Use of classification systems (e.g., Robson classification) to monitor C-section rates, indications and outcomes at a hospital or regional level helps identify areas for improvement.
6.2 Management Optimisation (When C-section is being planned or necessary)
-
Pre-pregnancy optimisation: Managing maternal health (e.g., controlling diabetes, managing hypertension, achieving healthy weight, treating anaemia) improves obstetric outcomes and may reduce need for surgical delivery.
-
Labour-care strategies: Minimising unnecessary labour interventions (induction, augmentation) when not medically indicated, allowing adequate labour time, monitoring progress appropriately.
-
Best surgical practices: Standardised protocols for surgical technique, antibiotic prophylaxis, thromboprophylaxis, wound care, early mobilisation. (See guideline references earlier)
-
Post-operative care protocols: Enhanced Recovery After Surgery (ERAS) adapted for caesarean births; early mobilization, early feeding, pain management, support for mother-baby contact and breastfeeding.
-
Follow-up and future pregnancy planning: After a C-section, discussion around future delivery mode, timing of next pregnancy (often waiting 18-24 months recommended though local guidelines vary), planning for monitoring placenta/uterine scar in future pregnancy.
6.3 Practical Tips for Pregnant Women and Families
-
During pregnancy: Attend regular antenatal care, discuss delivery plan with obstetrician early, ask about the possibility of vaginal birth and what conditions might lead to C-section.
-
During labour: Ask about progress, understand if interventions are needed, ask for second opinion if C-section is recommended without clear indication.
-
After the surgery: Follow hospital instructions for wound care, mobilise early, maintain good nutrition and hydration, watch for warning signs, attend follow-up.
-
For future pregnancies: Keep records of uterine incision type, placental history, discuss VBAC possibility if appropriate, and plan with your obstetrician.
In essence: While not all C-sections can or should be prevented (many are essential), through good care systems, patient education, and evidence-based practice, unnecessary C-sections can be reduced and outcomes optimised.
Complications of Caesarean Section
A Caesarean Section (C-section), while generally safe and lifesaving, is a major surgical procedure that carries potential short-term and long-term complications for both mother and baby. These complications depend on the patient's health, surgical technique, and timing (emergency vs. elective).
7.1 Short-Term Complications
-
Hemorrhage: Greater blood loss compared to vaginal delivery; may require transfusion.
-
Wound complications: infection (wound, uterine), dehiscence (splitting), haematoma. Evidence: ~8 % of women who have had C-section may develop endometritis, urinary-tract infection or wound infection.
-
Anaesthesia complications: especially if general anaesthesia used (airway risk, aspiration, etc).
-
Injury to adjacent organs: bladder, ureter, bowel may be accidentally injured during the procedure (rare).
-
Thromboembolic events: Deep vein thrombosis (DVT), pulmonary embolism (PE) risk is higher in surgical delivery.
-
Neonatal risks: Babies born by elective C-section (especially before labour and before 39 weeks) may have increased risk of breathing problems (transient tachypnoea), NICU admission, delayed initiation of breastfeeding.
-
Adhesions: Although adhesion formation is a longer-term issue, it may begin early and cause pain or bowel obstruction later.
7.2 Long-Term Complications
-
Maternal:
-
Increased risk of abnormal placentation in future pregnancies - e.g., placenta accreta spectrum (where placenta invades past uterine wall) - associated with higher number of previous C-sections.
-
Uterine rupture: Particularly if future labour attempted after a prior uterine incision of certain types (classical vertical incision) or multiple prior C-sections.
-
Pelvic adhesions: Leading to chronic pelvic pain, infertility, bowel obstruction, difficulty in subsequent surgeries.
-
Incisional hernia: At the abdominal incision site.
-
Longer recovery: Compared with vaginal delivery, the recovery after C-section is often longer and may impact mother-baby bonding, early mobility, breastfeeding initiation.
-
-
Neonatal / Child: Some studies suggest higher risk of asthma, obesity, and altered immune function in children born by C-section (though causality is complex and multifactorial).
-
For future pregnancies: Higher risks of placenta praevia, placental abruption, stillbirth, infertility, hysterectomy (in extreme cases) if complications of prior C-section scar/placenta occur.
7.3 Implications and Mitigation
To mitigate complications:
-
Use C-section only when clearly indicated.
-
Employ best surgical and postoperative protocols (antibiotics, thromboprophylaxis, early mobilisation).
-
In future pregnancies, ensure careful monitoring of placenta/uterine scar and discuss delivery mode well in advance.
-
Educate mothers and families about warning signs and need for follow-up.
In short: While many mothers and babies fare well with C-sections, the possibility of complications underscores the importance of judicious use, high-quality surgical care, and attentive follow-up.
Living with the Condition of Caesarean Section
Living with the condition of a Caesarean Section (C-section) involves a combination of physical recovery, emotional adaptation, and lifestyle adjustment during the postpartum period. Since it is a major abdominal surgery, a woman's recovery can take several weeks, depending on her overall health, type of incision, and level of postnatal support.
8.1 Recovery Timeline and Home Care
-
Typical recovery: Many women begin normal activities within 4-8 weeks after a C-section, but complete healing (especially of the uterine scar, abdominal wall, internal healing) takes longer and varies by individual.
-
Incision care: Keep the incision clean and dry, monitor for signs of infection (redness, swelling, discharge, increasing pain), avoid soaking in a bathtub until cleared by doctor.
-
Mobilisation: Early walking (within hours of surgery if medically safe) is encouraged to reduce risk of thrombosis and improve recovery. Avoid heavy lifting (anything heavier than the baby) for typically 6-8 weeks (or as advised).
-
Nutrition: Balanced diet rich in protein, vitamins and fluids supports healing and energy for mother and baby. Preventing constipation (a common issue after surgery) via fibre, fluids and mobilisation is important.
-
Pain management: Use of analgesics as advised; avoid over-use of narcotics; consider non-pharmacologic supports.
-
Breastfeeding and mother-baby bonding: Encourage skin-to-skin contact as soon as mother is awake/alert, help support positioning (e.g., football hold, side-lying) to reduce pressure on incision. Guidelines emphasise early skin-to-skin and breastfeeding support even after C-section.
-
Emotional/psychological support: Some women may feel disappointment if they planned for vaginal birth and ended with C-section, or feel anxious about recovery or future pregnancies. Emotional support, counselling or peer groups may help.
-
Warning signs: Educate about fever, increasing pain, excessive bleeding, leg swelling/pain, chest pain/breathlessness, persistent nausea/vomiting or inability to pass urine/bowel - all warrant prompt medical attention.
8.2 Planning for Future Pregnancies
-
Keep record of type of uterine incision, any complications from the surgery, placenta history, and discuss future delivery with obstetrician.
-
If considering VBAC: Assess eligibility (type of previous incision, number of prior C-sections, interval since last delivery, maternal/fetal health, facility capability).
-
Discuss timing of next pregnancy: Some guidelines recommend an inter-pregnancy interval of 18-24 months to reduce risk of uterine rupture or placenta complications, though local guidelines may differ.
-
Monitor early in pregnancy for placental abnormalities (praevia, accreta) especially if previous C-section(s) present.
-
Maintain healthy lifestyle: Normalise weight, control any chronic conditions (diabetes, hypertension), ensure good antenatal care, and discuss birth plan early.
8.3 Long-Term Considerations and Lifestyle
-
Scar care: Some may experience numbness, itching or discomfort around the incision site; gentle exercise and abdominal strengthening (once cleared) may help.
-
Pelvic floor and core rehabilitation: Because recovery from C-section may still impact abdominal/pelvic muscles, consider physiotherapy or gentle core/pelvic floor exercises when authorised by physician.
-
Discuss childbirth mode with each pregnancy: Even if previous C-section occurred, VBAC may still be an option in many cases - but needs individual assessment.
-
Mental health: Post-partum depression risk exists whether vaginal or C-section delivery; but if recovery is slower or there are complications, extra vigilance may be needed.
-
Family/personal planning: Recovery affects mobility, ability to care for baby, household tasks - having support (family, friends, professional) in the first 4-6 weeks is especially beneficial.
8.4 Encouragement and Outlook
For most women who undergo C-section, with good care and follow-up, full recovery is achievable and they go on to have healthy subsequent pregnancies and deliveries. The key is being informed, supported, and in partnership with your healthcare team. Encourage open dialogue with your obstetrician about your delivery plan, recovery expectations, future pregnancies, and lifestyle modifications.
Top 10 Frequently Asked Questions about Caesarean Section
1. What is a Caesarean Section?
A Caesarean Section (C-Section) is a surgical procedure used to deliver a baby through incisions made in the mother's abdomen and uterus. This method is employed when a vaginal delivery would pose a risk to the mother or baby. While vaginal birth is the preferred method of delivery, C-sections are sometimes necessary for medical reasons.
2. Why Might a C-Section Be Recommended?
A C-section may be recommended for various reasons, including:
-
Fetal Distress: Signs that the baby is not receiving enough oxygen.
-
Breech Presentation: When the baby is positioned feet or buttocks first.
-
Placental Complications: Such as placenta previa or placental abruption.
-
Multiple Births: Delivering twins or more, especially if one or more are in abnormal positions.
-
Failure to Progress in Labor: When labor stalls despite efforts to stimulate it.
-
Maternal Health Conditions: Including high blood pressure, heart disease, or active genital herpes infection.
3. Will I Be Awake During the Procedure?
In most cases, the mother remains awake during a C-section. Regional anesthesia, such as an epidural or spinal block, is administered to numb the lower half of the body. This allows the mother to be alert and to see and hold her baby immediately after birth. General anesthesia, which puts the mother to sleep, is typically reserved for emergency situations.
4. What Kind of Scar Can I Expect?
The most common type of incision used in C-sections is called a "bikini cut", a horizontal incision made just above the pubic hairline. This type of incision is often preferred as it is less noticeable and heals well. In some cases, especially during emergency C-sections, a vertical incision may be made. The length of the incision is usually about 4 to 6 inches, sufficient to allow the baby to be delivered safely.
5. How Long Does the Surgery Take?
The actual surgical procedure typically takes about 45 minutes to an hour. This includes making the incisions, delivering the baby, and closing the incisions. However, the total time in the operating room may be longer due to preparation and recovery time.
6. What Is the Recovery Time After a C-Section?
Recovery from a C-section generally takes longer than from a vaginal birth. Most women stay in the hospital for about 2 to 4 days after the surgery. Full recovery, including returning to normal activities, can take about 6 to 8 weeks. During this time, it's important to rest, avoid heavy lifting, and follow your healthcare provider's instructions to ensure proper healing.
7. Are There Risks Associated with a C-Section?
Like any major surgery, a C-section carries certain risks, including:
-
Infection: At the incision site or in the uterus.
-
Heavy Bleeding: More common than with vaginal birth.
-
Blood Clots: Increased risk of deep vein thrombosis or pulmonary embolism.
-
Injury to Organs: Rare, but possible damage to the bladder or bowel.
-
Anesthesia Complications: Reactions to the anesthesia used during the procedure.
8. Can I Have a Vaginal Birth After a C-Section (VBAC)?
In some cases, a vaginal birth after a C-section (VBAC) is possible. However, it depends on various factors, including the type of incision made during the previous C-section, the reason for the initial C-section, and the overall health of the mother and baby. It's essential to discuss VBAC options with your healthcare provider to determine the safest delivery method for your situation.
9. How Will a C-Section Affect Future Pregnancies?
Having a C-section can impact future pregnancies. The risks associated with multiple C-sections include:
-
Placenta Previa: The placenta covers the cervix, which can cause complications during delivery.
-
Placenta Accreta: The placenta grows too deeply into the uterine wall, increasing the risk of severe bleeding.
-
Uterine Rupture: A tear in the uterus at the site of the previous C-section scar, which can be life-threatening.
It's important to discuss these risks with your healthcare provider when planning future pregnancies.
10. Can I Breastfeed After a C-Section?
Yes, you can breastfeed after a C-section. In fact, early skin-to-skin contact and breastfeeding can help with bonding and may promote better recovery. While you may experience some discomfort, especially if your incision is healing, many mothers find breastfeeding to be a rewarding experience. If you encounter difficulties, such as pain or latch issues, lactation consultants are available to provide support and guidance.


