Introduction to Cardiac Mapping
Cardiac Mapping is a sophisticated and minimally invasive medical procedure used to study and analyze the heart's electrical activity. It helps doctors pinpoint the exact location and cause of irregular heartbeats, also known as arrhythmias. The heart functions through a precise rhythm of electrical impulses that travel through specific pathways, ensuring that it beats in an organized and efficient manner. When these electrical signals are disrupted or misdirected, the heart can beat too fast, too slow, or irregularly - potentially leading to symptoms like dizziness, palpitations, fainting, or even cardiac arrest.
The cardiac mapping procedure allows cardiologists and electrophysiologists (heart rhythm specialists) to create a detailed map of the electrical conduction patterns inside the heart. This “map” visually represents how electrical impulses move through various chambers, helping to identify abnormal areas that may be triggering the arrhythmia. Once identified, these areas can be treated with targeted procedures such as catheter ablation to restore a normal rhythm.
Over the years, cardiac mapping technology has advanced tremendously. Today, doctors can use three-dimensional (3D) electroanatomical mapping systems that provide real-time images of the heart's electrical activity. These systems not only improve accuracy but also reduce procedure times and radiation exposure. In some cases, non-invasive mapping systems can detect arrhythmias through sensors placed on the chest without needing to insert catheters.
In essence, cardiac mapping is both a diagnostic and therapeutic tool - offering patients a pathway toward personalized, precise treatment for complex heart rhythm disorders.
Causes and Risks Leading to Cardiac Mapping
Cardiac mapping itself is not a disease; rather, it is a medical procedure performed to diagnose or treat electrical disorders of the heart. Several underlying causes and risk factors can lead to the need for cardiac mapping.
Common Causes:
-
Arrhythmias: This includes conditions such as atrial
fibrillation, atrial flutter, supraventricular tachycardia (SVT), and
ventricular tachycardia (VT). Mapping helps identify the origin of these
abnormal electrical circuits.
-
Heart Attack (Myocardial Infarction): After a heart
attack, scar tissue can form in the heart muscle, which disrupts the
normal electrical pathways, leading to dangerous rhythm disturbances.
-
Heart Failure: When the heart's pumping ability
declines, electrical conduction can also be affected, resulting in
irregular rhythms.
-
Congenital Heart Defects: Some people are born with
abnormal electrical circuits or accessory pathways that cause
arrhythmias from a young age.
-
Post-Surgical Arrhythmias: After heart surgery, scar
tissue or changes in anatomy may trigger abnormal rhythms.
Risk Factors That Increase the Need for Cardiac Mapping:
-
High blood pressure and coronary artery disease
-
Diabetes and obesity
-
Excessive alcohol or caffeine intake
-
Smoking and chronic stress
-
Family history of arrhythmias
-
Electrolyte imbalances (especially potassium and magnesium)
-
Use of certain medications or stimulants that affect the heart's rhythm
Arrhythmias: This includes conditions such as atrial fibrillation, atrial flutter, supraventricular tachycardia (SVT), and ventricular tachycardia (VT). Mapping helps identify the origin of these abnormal electrical circuits.
Heart Attack (Myocardial Infarction): After a heart attack, scar tissue can form in the heart muscle, which disrupts the normal electrical pathways, leading to dangerous rhythm disturbances.
Heart Failure: When the heart's pumping ability declines, electrical conduction can also be affected, resulting in irregular rhythms.
Congenital Heart Defects: Some people are born with abnormal electrical circuits or accessory pathways that cause arrhythmias from a young age.
Post-Surgical Arrhythmias: After heart surgery, scar tissue or changes in anatomy may trigger abnormal rhythms.
-
High blood pressure and coronary artery disease
-
Diabetes and obesity
-
Excessive alcohol or caffeine intake
-
Smoking and chronic stress
-
Family history of arrhythmias
-
Electrolyte imbalances (especially potassium and magnesium)
-
Use of certain medications or stimulants that affect the heart's rhythm
Mapping becomes especially important for patients at risk of sudden cardiac arrest or those who have experienced fainting episodes (syncope) or palpitations that could not be diagnosed through standard ECG tests.
While cardiac mapping is generally safe, the risks are slightly higher in individuals with advanced heart failure, severe coronary blockages, or bleeding disorders. However, in the hands of skilled cardiac electrophysiologists, complications are rare, and the benefits far outweigh the risks.
Symptoms and Signs Leading to Cardiac Mapping
The symptoms that bring patients to cardiac mapping are often related to abnormal electrical activity of the heart. Many of these symptoms are intermittent, making them difficult to capture on routine ECG tests, which is why cardiac mapping is often recommended.
Common Symptoms Include:
-
Palpitations: A sensation of fluttering, pounding, or
racing heartbeat. Some patients describe it as their heart “skipping a
beat.”
-
Dizziness or Fainting (Syncope): Caused by sudden drops
in blood flow when the heart beats too fast or too slowly.
-
Shortness of Breath: When irregular rhythms prevent the
heart from pumping efficiently, oxygen delivery to the body decreases.
-
Chest Pain or Discomfort: Arrhythmias can cause chest
pressure or discomfort similar to angina.
-
Fatigue or Weakness: Due to reduced cardiac output
caused by irregular heartbeats.
-
Anxiety and Restlessness: Patients may experience
uneasiness or panic during episodes of rapid heartbeats.
Physical and Clinical Signs:
-
Irregular pulse or fluctuating heart rate during examination.
-
ECG abnormalities showing premature beats, conduction delays, or
sustained tachycardia.
-
Evidence of heart failure, such as ankle swelling or fluid buildup in the
lungs.
Palpitations: A sensation of fluttering, pounding, or racing heartbeat. Some patients describe it as their heart “skipping a beat.”
Dizziness or Fainting (Syncope): Caused by sudden drops in blood flow when the heart beats too fast or too slowly.
Shortness of Breath: When irregular rhythms prevent the heart from pumping efficiently, oxygen delivery to the body decreases.
Chest Pain or Discomfort: Arrhythmias can cause chest pressure or discomfort similar to angina.
Fatigue or Weakness: Due to reduced cardiac output caused by irregular heartbeats.
Anxiety and Restlessness: Patients may experience uneasiness or panic during episodes of rapid heartbeats.
-
Irregular pulse or fluctuating heart rate during examination.
-
ECG abnormalities showing premature beats, conduction delays, or sustained tachycardia.
-
Evidence of heart failure, such as ankle swelling or fluid buildup in the lungs.
Patients presenting with these signs and symptoms - especially if they are recurrent or unexplained - are often referred for an electrophysiology (EP) study that includes cardiac mapping to pinpoint the cause.
Diagnosis Using Cardiac Mapping
The diagnosis of heart rhythm problems often begins with standard non-invasive tests like ECG, Holter monitoring, or echocardiography. However, when these tests are inconclusive or when complex arrhythmias are suspected, cardiac mapping is the next step.
How the Procedure Works:
Cardiac mapping is usually performed in a specialized lab called an electrophysiology lab (EP lab). The procedure involves inserting thin, flexible catheters into a vein, usually in the groin or wrist. These catheters are guided to the heart using real-time imaging. Tiny electrodes at the tip of the catheter record electrical signals from different areas inside the heart.
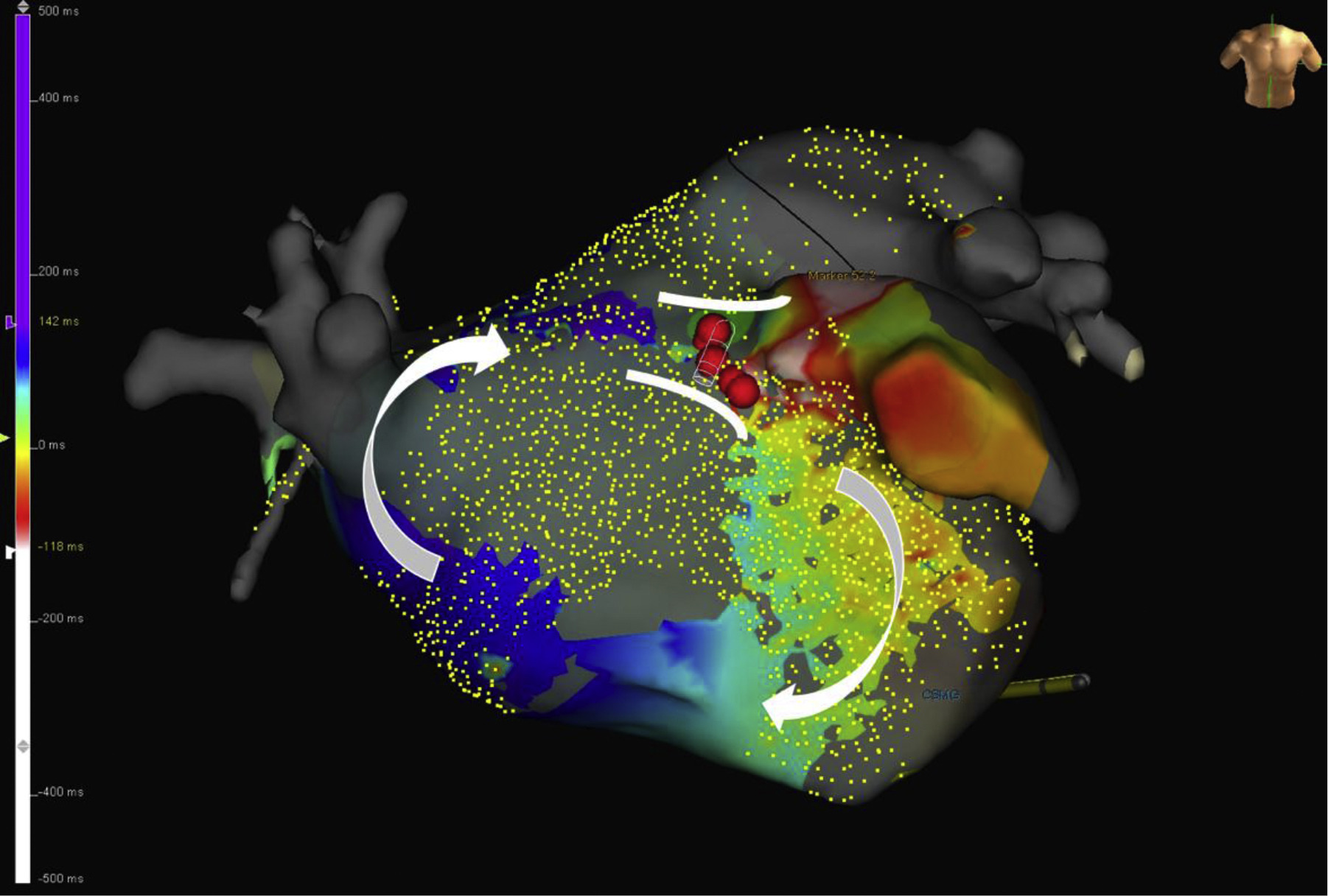
The data collected is processed by advanced software to create a detailed, 3D map that shows the electrical activity throughout the heart chambers. This map allows doctors to identify areas that are firing abnormally or conducting impulses incorrectly.
Types of Mapping:
-
Activation Mapping: Identifies the sequence of
electrical activation during an arrhythmia.
-
Voltage Mapping: Measures the strength of electrical
signals to detect scarred or damaged areas.
-
Phase Mapping: Used in complex cases like atrial
fibrillation to visualise rotational wavefronts.
-
Non-Invasive Mapping: Uses sensors placed on the chest
to reconstruct electrical patterns without catheter insertion.
Activation Mapping: Identifies the sequence of electrical activation during an arrhythmia.
Voltage Mapping: Measures the strength of electrical signals to detect scarred or damaged areas.
Phase Mapping: Used in complex cases like atrial fibrillation to visualise rotational wavefronts.
Non-Invasive Mapping: Uses sensors placed on the chest to reconstruct electrical patterns without catheter insertion.
Once the abnormal area is identified, the physician may proceed with an ablation in the same session, destroying or isolating the tissue responsible for the irregular rhythm.
Treatment Options Related to Cardiac Mapping
Cardiac mapping is an essential gateway to treating heart rhythm disorders. It provides the information needed to plan and perform precise and effective interventions.
Primary Treatment Approaches Include:
-
Catheter Ablation: The most common follow-up treatment.
Using the mapping results, doctors apply heat (radiofrequency ablation)
or cold energy (cryoablation) to destroy the small area of heart tissue
causing the abnormal rhythm.
-
Medication Management: If the mapped arrhythmia is mild
or infrequent, anti-arrhythmic medications or rate-control drugs may be
prescribed to regulate heart rhythm.
-
Device Implantation: In patients with life-threatening
rhythm problems, mapping helps determine the need for an
implantable cardioverter-defibrillator (ICD) or
pacemaker.
-
Surgical Intervention: In rare cases where catheter
ablation is not suitable, surgical procedures may be performed, guided
by the mapping results.
Recent Technological Advances:
Catheter Ablation: The most common follow-up treatment. Using the mapping results, doctors apply heat (radiofrequency ablation) or cold energy (cryoablation) to destroy the small area of heart tissue causing the abnormal rhythm.
Medication Management: If the mapped arrhythmia is mild or infrequent, anti-arrhythmic medications or rate-control drugs may be prescribed to regulate heart rhythm.
Device Implantation: In patients with life-threatening rhythm problems, mapping helps determine the need for an implantable cardioverter-defibrillator (ICD) or pacemaker.
Surgical Intervention: In rare cases where catheter ablation is not suitable, surgical procedures may be performed, guided by the mapping results.
Modern cardiac mapping systems have dramatically improved accuracy and safety. High-density mapping catheters now collect thousands of data points in seconds, providing real-time imaging with unmatched precision. Integration with imaging technologies like MRI or CT allows for combined anatomical and electrical views of the heart, enhancing treatment outcomes.
Prevention and Management of Cardiac Mapping Conditions
While cardiac mapping is primarily a diagnostic tool, many arrhythmias that require it can be prevented or managed with a healthy lifestyle and proper medical care.
Prevention Strategies:
-
Maintain a Heart-Healthy Lifestyle: Eat a balanced diet
rich in fruits, vegetables, whole grains, and lean proteins while
limiting processed foods, sugar, and saturated fats.
-
Control Risk Factors: Manage blood pressure,
cholesterol, and diabetes with regular checkups and medications.
-
Stay Active: Engage in at least 30 minutes of moderate
exercise most days of the week.
-
Avoid Triggers: Limit caffeine, alcohol, and energy
drinks that may provoke irregular rhythms.
-
Quit Smoking: Smoking damages the heart's electrical
system and blood vessels.
-
Manage Stress: Chronic stress can increase heart rate
and trigger arrhythmias; meditation and yoga may help.
Post-Mapping Management:
Maintain a Heart-Healthy Lifestyle: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting processed foods, sugar, and saturated fats.
Control Risk Factors: Manage blood pressure, cholesterol, and diabetes with regular checkups and medications.
Stay Active: Engage in at least 30 minutes of moderate exercise most days of the week.
Avoid Triggers: Limit caffeine, alcohol, and energy drinks that may provoke irregular rhythms.
Quit Smoking: Smoking damages the heart's electrical system and blood vessels.
Manage Stress: Chronic stress can increase heart rate and trigger arrhythmias; meditation and yoga may help.
After the mapping procedure, patients are typically observed for several hours. Most can resume normal activities within a day or two. If ablation was performed, mild fatigue or soreness at the catheter site is normal for a few days.
Patients should follow their doctor's advice on medications, physical activity, and follow-up appointments. Long-term management focuses on preventing recurrence, monitoring heart rhythm, and maintaining heart health.
Complications of Cardiac Mapping
Cardiac mapping is considered safe, especially when performed in specialized centers by experienced cardiologists. However, as with any invasive procedure, there are potential risks and complications to be aware of.
Possible Complications Include:
-
Bleeding or Bruising: At the catheter insertion site,
usually in the groin or wrist.
-
Vascular Damage: Rare injury to blood vessels during
catheter insertion.
-
Arrhythmia Induction: The procedure may temporarily
provoke irregular rhythms.
-
Cardiac Perforation: Very rare but serious complication
where the catheter punctures the heart wall, leading to fluid
accumulation around the heart.
-
Allergic Reactions: To the contrast dye or medications
used during the procedure.
-
Infection: Minimal risk at the insertion site.
-
Kidney Effects: Rare in patients with pre-existing
kidney disease due to contrast dye.
Bleeding or Bruising: At the catheter insertion site, usually in the groin or wrist.
Vascular Damage: Rare injury to blood vessels during catheter insertion.
Arrhythmia Induction: The procedure may temporarily provoke irregular rhythms.
Cardiac Perforation: Very rare but serious complication where the catheter punctures the heart wall, leading to fluid accumulation around the heart.
Allergic Reactions: To the contrast dye or medications used during the procedure.
Infection: Minimal risk at the insertion site.
Kidney Effects: Rare in patients with pre-existing kidney disease due to contrast dye.
To minimize risks, patients undergo pre-procedure assessments, and the procedure is conducted under continuous monitoring using advanced imaging systems. With modern technology, serious complications occur in less than 1% of cases.
Living with the Condition After Cardiac Mapping
Life after cardiac mapping - and any subsequent treatment such as ablation or device implantation - is typically positive and empowering. Patients often experience relief from symptoms and a significant improvement in quality of life.
Early Recovery:
-
Rest for the first 24 hours and avoid strenuous activity for a few days.
-
Keep the catheter site clean and dry.
-
Stay hydrated to help flush out contrast material.
-
Report any unusual symptoms such as bleeding, swelling, or severe pain to
your doctor immediately.
Long-Term Lifestyle:
-
Continue heart-healthy habits and maintain follow-up appointments.
-
Take medications exactly as prescribed, especially anticoagulants if
recommended.
-
Monitor your heart rhythm through periodic ECG or Holter tests.
-
Participate in a cardiac rehabilitation program if advised.
-
Manage emotional well-being - anxiety after an arrhythmia episode is
common, and counseling or support groups can be helpful.
Prognosis and Outlook:
Rest for the first 24 hours and avoid strenuous activity for a few days.
Keep the catheter site clean and dry.
Stay hydrated to help flush out contrast material.
Report any unusual symptoms such as bleeding, swelling, or severe pain to your doctor immediately.
-
Continue heart-healthy habits and maintain follow-up appointments.
-
Take medications exactly as prescribed, especially anticoagulants if recommended.
-
Monitor your heart rhythm through periodic ECG or Holter tests.
-
Participate in a cardiac rehabilitation program if advised.
-
Manage emotional well-being - anxiety after an arrhythmia episode is common, and counseling or support groups can be helpful.
Prognosis and Outlook:
Most patients treated based on cardiac mapping enjoy long-lasting results, with reduced symptoms and improved overall health. Advanced mapping and ablation techniques have high success rates, especially for common arrhythmias like atrial fibrillation and SVT.
By adopting a proactive approach - combining medical care with healthy living - patients can maintain stable heart rhythms and lead active, fulfilling lives for many years after treatment.
Top 10 Frequently Asked Questions about Cardiac Mapping
1. What is Cardiac Mapping and why is it important?
Cardiac Mapping is an advanced diagnostic technique that allows doctors to study the electrical activity of the heart in real time. It helps locate the exact source of abnormal electrical signals responsible for irregular heart rhythms or arrhythmias.
During this procedure, catheters equipped with tiny electrodes are inserted into the heart through a blood vessel, and a specialized computer records the electrical signals. This creates a three-dimensional map showing how electrical impulses travel through different areas of the heart.
Cardiac mapping plays a critical role in diagnosing and treating heart rhythm problems such as atrial fibrillation (AFib), atrial flutter, ventricular tachycardia (VT), and supraventricular tachycardia (SVT). It allows doctors to precisely identify abnormal tissues and plan procedures like catheter ablation to restore a normal heartbeat.
2. When is Cardiac Mapping recommended?
Doctors may recommend cardiac mapping if you have symptoms such as:
-
Rapid or irregular heartbeats (palpitations)
-
Fainting or dizziness
-
Shortness of breath or chest discomfort
-
Fatigue or weakness related to an irregular pulse
It's also used when standard tests like ECG, Holter monitoring, or echocardiograms fail to pinpoint the cause of the arrhythmia. Cardiac mapping is often performed before catheter ablation, helping the electrophysiologist locate the abnormal pathway that causes irregular electrical activity.
In some cases, cardiac mapping is used to evaluate the success of prior ablations or other heart surgeries, or to plan complex arrhythmia treatments.
3. How is the Cardiac Mapping procedure performed?
Cardiac mapping is performed by a cardiac electrophysiologist in a specialized lab known as an electrophysiology (EP) lab.
Here's a step-by-step overview:
-
Preparation: You'll lie on a special table, and local anesthesia will be given near the insertion site (typically in the groin or neck). You may also receive light sedation to help you relax.
-
Catheter Insertion: Thin, flexible tubes called catheters are gently inserted into your vein or artery and guided into the heart using real-time X-ray imaging.
-
Data Collection: The catheters contain sensors that detect and record the heart's electrical signals from various regions.
-
Mapping: These signals are sent to a computer system that generates a 3D map of the heart's electrical pathways, showing normal and abnormal activity.
-
Diagnosis or Treatment: If abnormal areas are found, your doctor may perform catheter ablation during the same session to treat the arrhythmia.
The entire procedure typically takes 2 to 4 hours, depending on the complexity of your condition.
4. Is Cardiac Mapping painful or uncomfortable?
Most patients experience little to no pain during cardiac mapping. The procedure is performed under local anesthesia and sedation, so you remain comfortable and relaxed.
You may feel mild pressure at the catheter insertion site or a fluttering sensation in the chest when the doctor stimulates your heart to analyze electrical patterns. Afterward, you might notice slight bruising or soreness at the site, but this usually resolves within a few days.
Pain is minimal, and serious discomfort is extremely rare.
5. What are the different types of Cardiac Mapping systems?
Modern cardiology uses several advanced mapping systems, including:
-
Contact Mapping: Uses catheters that directly touch the heart's surface to record electrical activity.
-
Non-Contact Mapping: Creates detailed maps using electrodes placed inside the heart chamber without needing direct contact.
-
3D Electroanatomical Mapping (EAM): Combines electrical data with anatomical images of the heart to create a precise, real-time 3D model.
-
High-Density Mapping Systems: Capture thousands of data points in seconds, offering greater accuracy in complex arrhythmias.
The choice of system depends on the type of arrhythmia and the specific area of the heart being studied.
6. What are the risks or complications of Cardiac Mapping?
Cardiac mapping is generally a safe and low-risk procedure, but as with any invasive technique, some risks exist. These include:
-
Minor bleeding or bruising at the catheter site
-
Infection (rare)
-
Damage to blood vessels or the heart wall (very rare)
-
Allergic reaction to contrast dye or anesthesia
-
Temporary irregular heartbeats during testing
Complications are rare and are minimized by performing the procedure in advanced electrophysiology labs with experienced specialists.
7. How should I prepare for Cardiac Mapping?
Preparation is crucial for a safe and accurate procedure. You'll likely be advised to:
-
Avoid food and drink for 6–8 hours before the procedure.
-
Inform your doctor about all medications, especially blood thinners, diabetes medicines, or antiarrhythmics.
-
Stop certain medications temporarily, as they may interfere with the results.
-
Wear comfortable clothing and remove jewelry or metal objects.
-
Arrange for someone to drive you home afterward.
Your healthcare team will provide customized instructions based on your health condition and medications.
8. What happens after Cardiac Mapping?
After the procedure:
-
You'll be monitored in a recovery area for a few hours.
-
Pressure will be applied to the catheter site to prevent bleeding.
-
Most patients can go home the same day or after an overnight stay, depending on whether an ablation was done.
-
Avoid strenuous activity or heavy lifting for 24–48 hours.
Your doctor will discuss the results and recommend the next steps - whether that's medication adjustment, catheter ablation, or further follow-up.
9. What are the benefits of Cardiac Mapping?
Cardiac mapping offers several significant advantages:
-
Accurate diagnosis of the exact source of arrhythmias.
-
Reduced procedure time during ablation.
-
Improved success rates of arrhythmia treatment.
-
Fewer complications, as the abnormal tissue is precisely targeted.
-
Real-time 3D visualization of the heart's electrical system for better decision-making.
This technology has transformed how cardiac arrhythmias are diagnosed and treated, leading to safer and more effective outcomes.
10. What is the success rate and long-term outcome of Cardiac Mapping?
Cardiac mapping itself is a diagnostic tool, but when combined with catheter ablation, it dramatically increases treatment success rates. Studies show that:
-
Success rates for treating arrhythmias like AFib and SVT exceed 80–90%.
-
Most patients experience a significant reduction or complete resolution of arrhythmia symptoms.
-
Complication rates remain very low, especially in specialized cardiac centers.
With modern mapping technology, patients not only gain relief from symptoms but also reduce their long-term risk of heart failure, stroke, and other heart-related complications.


