Introduction to Carotid Endarterectomy
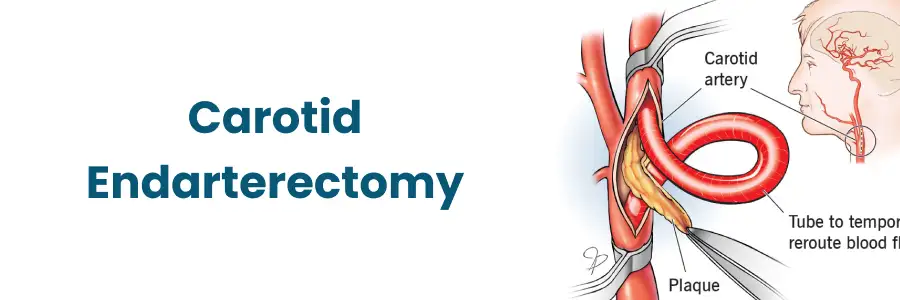
Carotid endarterectomy is a surgical procedure aimed at reducing the risk of stroke by removing plaque from the carotid artery, the major blood vessel in the neck responsible for supplying oxygen-rich blood to the brain. When the carotid artery becomes significantly narrowed (stenosed) due to atherosclerosis - the buildup of fatty deposits, cholesterol, and inflammatory material - blood flow to the brain may be compromised, or plaque fragments may break off and cause embolic strokes. CEA involves making an incision in the neck, exposing the affected artery (typically the internal carotid artery or the common carotid bifurcation), clamping the artery, opening it lengthwise, removing the plaque and potentially repairing or patching the artery.
In modern practice, carotid endarterectomy remains considered the “gold standard” for certain patients with carotid stenosis who are at elevated risk of stroke, particularly those with symptomatic significant narrowing. Recent analyses reaffirm that despite advances in medical therapy and alternative interventions like stenting, CEA continues to provide robust outcomes in appropriately selected patients.
This surgery is a key component in the management of carotid artery disease because it addresses both the mechanical narrowing and the risk of plaque embolization. In short: when standard medical therapy may not sufficiently reduce stroke risk in a high-risk artery, CEA offers a proactive, proven approach to restore blood flow, remove the hazard of the plaque itself, and thereby improve long-term brain protection.
Causes and Risk of Carotid Endarterectomy
Carotid endarterectomy (CEA) is a vascular surgical procedure performed to remove atherosclerotic plaque from the carotid arteries—main blood vessels supplying blood to the brain. It is primarily indicated to prevent stroke or transient ischemic attack (TIA) caused by carotid artery narrowing (stenosis).
Underlying Causes of Carotid Artery Disease
-
Atherosclerosis: The primary culprit-fatty, fibrous plaques accumulate in the inner wall (intima) of the carotid arteries, gradually narrowing the lumen, reducing blood flow, and creating unstable plaque that may rupture or shed emboli.
-
Hypertension (high blood pressure): Chronically elevated pressure damages the arterial wall's inner lining, facilitating plaque formation and progression.
-
Dyslipidemia: Particularly elevated LDL (“bad”) cholesterol, low HDL (“good”) cholesterol, increased triglycerides. These lipid-abnormalities promote plaque growth.
-
Diabetes mellitus: Elevated glucose levels and insulin resistance accelerate vascular damage and atherosclerosis.
-
Smoking/tobacco use: Tobacco toxins injure the endothelium, enhance inflammation, increase plaque vulnerability, and raise the risk of embolization.
-
Age and gender: Older age increases risk; historically males have had higher risk though women are not exempt and post-menopausal status may raise risk.
-
Family history and genetics: A family history of stroke, coronary artery disease, or carotid disease suggests a predisposition.
-
Additional risk-factors: Obesity, sedentary lifestyle, poor diet (high in saturated fat, low in vegetables/fibre), chronic kidney disease, sleep-apnoea, inflammatory and rheumatologic conditions.
Risk Context of the Surgery
-
CEA is not without risk: Patients undergoing carotid endarterectomy have to be selected carefully because the procedure is done to reduce risk of stroke, but it itself carries a small risk of peri-operative stroke, myocardial infarction, nerve injury, bleeding, or wound complications.
-
Indications and thresholds: Guidelines generally support CEA for symptomatic patients with stenosis usually >50%-70% (depending on study criteria) and for asymptomatic patients in selected settings (e.g., >60%-70% stenosis and low surgical risk). Over time, because medical therapy has improved, the benefit/risk balance is being re-examined.
-
Advances in medical therapy: Recent analyses suggest that modern optimal medical therapy may reduce the absolute benefit of surgery in some lower-risk patients, so risk-stratification is more important than ever.
Symptoms and Signs of Carotid Endarterectomy
The symptoms and signs of carotid endarterectomy (CEA) can be classified according to the preoperative (before surgery) and postoperative (after surgery) stages. Before CEA, symptoms are caused by carotid artery stenosis, while after surgery, certain local and systemic effects may be observed as part of recovery or as warning signs of complications.
Common Symptoms and Warning Signs
-
Transient ischemic attacks (TIAs): Brief episodes of neurological dysfunction (minutes to hours) such as sudden weakness or numbness of the face, arm or leg (especially on one side), sudden difficulty speaking or understanding speech, temporary loss or blurring of vision in one eye (amaurosis fugax). These are classic warning signs for carotid territory embolization.
-
Sudden weakness or numbness on one side: If a piece of plaque or clot embolizes to the brain, it may cause symptoms indicative of a minor stroke.
-
Difficulty with speech (aphasia) or confusion: Sudden onset of slurred speech or inability to form words or comprehend can be carotid in origin.
-
Vision problems: Temporary monocular blindness (“a curtain coming down” over the eye), or sudden blurred vision in one eye.
-
Dizziness, loss of coordination or balance: Though less specific, these may indicate compromised cerebral perfusion or embolic events.
-
Severe headache of sudden onset (less common in carotid disease but may indicate a major stroke event).
Signs on Examination
-
A bruit (whooshing sound) heard over the carotid artery on auscultation in the neck-indicates turbulent flow due to narrowing.
-
Neurologic deficits on exam: weakness, facial droop, abnormal gait, cognitive impairment, depending on prior strokes or TIAs.
-
In advanced disease, signs of chronic ischemia may appear: cognitive decline, subtle gait changes, or ocular ischemia.
Diagnosis of Carotid Endarterectomy
The diagnosis for carotid endarterectomy (CEA) is based on confirming carotid artery stenosis (narrowing) and assessing the severity, symptoms, and stroke risk to determine if surgery is indicated. Diagnostic evaluation involves clinical assessment, imaging studies, and risk stratification to ensure patients meet criteria for surgical intervention.
Diagnostic Process
-
Medical history & physical exam: Assess for symptoms (TIAs, strokes), risk-factors (hypertension, diabetes, smoking, hyperlipidaemia), neurologic and cardiovascular status, and listen for carotid bruit.
-
Non-invasive vascular imaging:
-
Carotid duplex ultrasonography (ultrasound): first-line test to assess degree of stenosis, plaque morphology, flow velocities.
-
CT angiography (CTA) or MR angiography (MRA): provide detailed imaging of the carotid arteries, plaque characteristics (ulceration, intraplaque hemorrhage), and collateral circulation.
-
Updated recommendations now provide standardized velocity criteria for >50% stenosis to improve accuracy.
-
-
Invasive angiography: In selected cases, cerebral angiography may be used to precisely define the lesion and plan the surgical approach.
-
Pre-operative evaluation: Cardiac evaluation (given risk of MI in surgery), assessment of other vascular beds, blood tests (lipids, glucose, kidney function, coagulation), neurological baseline, and sometimes cerebral perfusion studies.
-
Risk-stratification: Using tools like the CAR (Carotid Artery Risk) score (which factors in age, sex, MI history, hypertension, diabetes, peripheral vascular disease, time from symptom onset) to estimate benefit vs risk of surgery in modern era.
-
Determination of surgical candidacy: Considering the severity of stenosis (eg. >70% symptomatic, >60% asymptomatic in many guidelines), patient comorbidities, life-expectancy, and presence of high-risk plaque features or hemodynamic compromise.
Treatment Options of Carotid Endarterectomy
The treatment options for carotid endarterectomy (CEA) focus on restoring normal cerebral blood flow by removing atherosclerotic plaque from the carotid artery, thereby preventing future strokes or transient ischemic attacks (TIAs). The approach may include open surgical techniques and adjunctive management strategies for optimal outcomes.
Overview of Treatment Pathways
Once diagnosis is confirmed and candidacy assessed, treatment falls into three broad categories:
-
Optimal medical therapy (OMT): Risk-factor control (blood pressure, lipids, diabetes), antiplatelet therapy, lifestyle changes. In many patients (especially asymptomatic or lower-risk), OMT may be sufficient. Recent trials suggest medical therapy alone may be adequate for some.
-
Carotid endarterectomy (CEA): The surgical removal of plaque and restoration of normal blood flow. This remains the standard for many patients with symptomatic high-grade stenosis.
-
Alternatives such as carotid artery stenting (CAS) or transcarotid revascularization (TCAR): Less invasive options, generally reserved for high-surgical-risk patients (e.g., prior neck radiation, anatomical challenges, severe comorbidities) but with somewhat higher risk of peri-procedural stroke compared to CEA in many studies.
Key Details of CEA
-
Indications: For symptomatic carotid stenosis (e.g., TIA or minor stroke) with ipsilateral internal carotid artery stenosis of typically ≥50% or more (depending on criteria) and for asymptomatic stenosis often ≥60-70% in selected patients with low perioperative risk.
-
Timing: For symptomatic patients, sooner is better-ideally within two weeks of the neurologic event if patient is stable, because benefit is greatest early.
-
Surgical technique: Under general or local anaesthesia; expose carotid artery, clamp proximal/distal, open artery, remove plaque, possibly insert shunt to maintain cerebral perfusion intra-operatively, then close artery often with patch angioplasty to minimize restenosis. Monitoring of neurologic status, cerebral oximetry, or intraoperative EEG/SSEP may be used.
-
Outcomes: Numerous landmark trials (e.g., NASCET, ECST) have demonstrated significant stroke-risk reduction when CEA is done in selected patients. Recent data reaffirm benefit and also highlight that in asymptomatic low-risk patients, modern medical therapy may reduce the marginal benefit of surgery. For example, a nationwide French cohort found that peri-operative stroke or death at 30 days was 1.5% for CEA vs higher for CAS.
-
Choice between CEA and alternatives: Current guidelines generally prefer CEA for standard surgical risk patients with appropriate anatomy; alternatives reserved for high-risk patients. A 2021 guideline from the Society for Vascular Surgery recommended CEA over transfemoral CAS for low- and standard-risk patients with >50% symptomatic carotid stenosis.
Shared Decision-Making
Each patient should be counselled about benefits, risks, and alternative options. Given improvements in medical therapy and evolving evidence (e.g., the CAR score model suggesting many patients may safely be managed medically), decision-making must be individualized-taking into account life expectancy, comorbidities, plaque morphology, patient preference, and institutional peri-operative risk.
Prevention and Management of Carotid Endarterectomy
The prevention and management of carotid endarterectomy (CEA) involve preoperative optimization, meticulous surgical care, and vigilant postoperative management to reduce the risk of complications such as stroke, hypertension, or restenosis. Successful outcomes depend on a multidisciplinary approach focusing on vascular health maintenance, medication adherence, and long-term surveillance.
Primary Prevention (Before Significant Disease)
-
Maintain optimal blood pressure control (often <130/80 mmHg unless contraindicated)
-
Healthy lipid management: statins, lifestyle-diet modifications (Mediterranean diet, reduced saturated fat, increased fibre)
-
Smoking cessation: quitting smoking is one of the most impactful steps.
-
Diabetes management: good glycaemic control reduces vascular complications.
-
Physical activity: aim for at least 30 minutes moderate aerobic exercise most days of the week.
-
Weight management: keep body mass index in healthy range, avoid central obesity.
-
Healthy diet: rich in fruits, vegetables, whole grains, lean protein, low in refined sugars and processed foods.
-
Lifestyle modifications: limit alcohol, correct sleep-apnoea if present, manage other comorbidities (kidney disease, inflammatory disease).
Secondary Prevention & Post-operative Management
After CEA or diagnosis of carotid disease:
-
Continue antiplatelet therapy (e.g., aspirin) unless contraindicated.
-
Continue statin therapy even if lipid-levels appear normal - statins stabilize plaque.
-
Maintain aggressive risk-factor control (blood pressure, glycaemic, lipids).
-
Regular imaging surveillance: After CEA, periodic duplex ultrasound to monitor for restenosis or progression in the contralateral carotid.
-
Lifestyle adherence: As above, but now in the context of known disease, the urgency of lifestyle change is greater.
-
Patient education: Recognize signs of stroke/TIA (sudden numbness/weakness, speech difficulty, vision loss) and know to seek immediate care.
-
Coordination of care: Vascular surgeon, neurologist, primary care physician, rehabilitation (if prior stroke), and possibly cardiologist involvement for concomitant coronary disease.
-
Manage other vascular beds: Patients with carotid disease often have coronary artery disease or peripheral vascular disease-comprehensive vascular risk management is essential.
-
Post-operative considerations: Monitor for blood pressure spikes (which could lead to hyperperfusion syndrome), cranial nerve dysfunction, wound care, and ensure good recovery.
Complications of Carotid Endarterectomy
Carotid endarterectomy (CEA) is a major vascular procedure with well-established benefits in preventing ischemic stroke, but it carries a range of potential surgical and medical complications. While complication rates are low in experienced centres, early recognition and management are crucial for patient recovery and long-term success.
While carotid endarterectomy is generally safe in experienced hands, complications can occur. Some of the key complications include:
-
Peri-operative stroke or transient ischemic attack: The most feared complication-the very outcome surgery is trying to prevent. Risk is low in properly selected patients but must be discussed.
-
Myocardial infarction (heart attack): Many patients have multi-vascular disease; surgery adds cardiac stress.
-
Cranial nerve injury: Because of proximity of nerves in the carotid sheath (e.g., hypoglossal, glossopharyngeal, vagus, accessory), patients may experience temporary or rarely permanent hoarseness, swallowing difficulty, tongue deviation, shoulder weakness.
-
Bleeding / haematoma: Post-operative neck hematoma can compress airway-a surgical emergency.
-
Wound infection: Particularly in patients with prior neck irradiation, diabetes, or immunocompromise.
-
Restenosis (re-narrowing) of the carotid artery: Although patch repair and modern techniques reduce risk, restenosis can occur and may require re-intervention.
-
Hyperperfusion syndrome: After restoration of blood flow, some patients may develop cerebral edema, headache, seizures, or intracerebral hemorrhage-often associated with uncontrolled hypertension post-operatively.
-
Contralateral carotid occlusion or poor collateral circulation: May increase risk of peri-operative cerebral ischemia.
-
General surgical risks: Anaesthetic complications, deep-vein thrombosis, pulmonary complications, renal impairment, etc.
It is essential to counsel patients about these risks and to ensure that the institution's peri-operative stroke/MI/death rates are acceptably low (e.g., <3% in many guidelines for asymptomatic patients) before proceeding.
Living with the Condition of Carotid Endarterectomy
Living with the condition following a carotid endarterectomy (CEA) involves recovery, lifestyle adjustments, and long-term preventive care to maintain healthy blood flow to the brain and prevent complications such as restenosis or stroke. Most people return to normal life within a few weeks, but ongoing management of cardiovascular health is critical.
Post-Treatment Follow-Up
-
Regular outpatient visits: Vascular surgeon or neurologist checks, primary care follow-up for risk-factor management.
-
Periodic vascular imaging: Duplex ultrasound of the treated and contralateral carotid arteries to detect restenosis or progression - commonly at 6 months, 12 months, then yearly or bi-yearly depending on findings.
-
Medication adherence: Lifelong antiplatelet therapy (often aspirin), statins, blood pressure medications, diabetes medications.
-
Lifestyle maintenance: The same healthy habits become even more vital after treatment: healthy diet, exercise, smoking avoidance, weight control, sleep hygiene.
Stroke Awareness & Rehabilitation
-
Patients must be educated on stroke signs (FAST: Face droop, Arm weakness, Speech difficulty, Time to call emergency).
-
If patient had a prior TIA or minor stroke, physical therapy, occupational therapy, speech therapy may be required to maximise recovery and quality of life.
-
Cognitive and psychological support: Vascular disease often impacts quality of life; screening for depression, cognitive decline, or sleep problems may be needed.
Quality of Life Considerations
-
Many patients return to normal or near-normal activities post-CEA if recovery is uncomplicated; however some adjustment in lifestyle is required.
-
Driving, sports, travel: After recovery and with physician guidance, most patients can resume, but must keep appointments and adhere to therapy.
-
Long-term vascular health: Patients should understand they have systemic vascular disease - carotids are one manifestation; the same disease process affects coronary and peripheral vessels.
Shared Responsibility & Education
-
Patient and family should engage in shared decision-making and ongoing education: understanding the condition, therapy rationale, risk signs, and lifestyle implications.
-
Engagement with a multidisciplinary care team (vascular surgeon, neurologist, cardiologist, primary care) improves outcomes.
Preventing Recurrence
-
Even after successful CEA, progression of atherosclerosis can occur; thus ongoing surveillance and prevention remain cornerstones.
-
Encouraging biomarkers: For example, maintaining LDL at target levels, HbA1c under control, blood pressure at goal, and regular exercise reduce risk of future events.
-
Addressing comorbidities: Sleep-apnoea therapy, treatment of atrial fibrillation (if present), carotid plaque morphology evaluation (ulceration, intraplaque hemorrhage) may provide additional insight and prevention.
Top 10 Frequently Asked Questions about Carotid Endarterectomy
1. What is Carotid Endarterectomy and why is it performed?
Carotid endarterectomy is a surgical procedure designed to remove plaque buildup from the carotid arteries, which supply blood to the brain. Plaque accumulation can cause narrowing (stenosis) of the arteries, reducing blood flow and increasing the risk of stroke or transient ischemic attacks (TIA).
The surgery involves opening the artery and removing the fatty deposits, which restores normal blood flow. In some cases, a small patch is used to widen the artery and ensure smooth circulation.
Purpose of the procedure:
-
Reduce the risk of stroke in patients with symptomatic carotid artery disease
-
Improve blood flow to the brain
-
Stabilize existing plaques to prevent rupture
-
Alleviate symptoms such as dizziness, weakness, or temporary vision changes caused by reduced cerebral perfusion
2. Who is a candidate for Carotid Endarterectomy?
Carotid endarterectomy is recommended for patients with significant carotid artery narrowing, particularly those who are at high risk of stroke.
Candidates typically include:
-
Patients with 50-70% narrowing of the carotid artery who have symptoms such as transient ischemic attacks or minor strokes
-
Patients with severe stenosis (>70%), even if asymptomatic, based on risk assessment
-
Individuals with rapidly progressing plaque or unstable plaques detected on imaging
-
Patients who cannot be treated adequately with medication or lifestyle modifications alone
Contraindications:
-
Severe heart or lung disease making surgery risky
-
Previous major stroke leaving significant neurological deficits
-
Patients who may benefit more from carotid artery stenting due to anatomical or medical considerations
3. How is the Carotid Endarterectomy procedure performed?
The procedure is performed under general or local anesthesia and typically takes 1-3 hours. The steps include:
-
Anesthesia: The patient is given general anesthesia or a combination of local anesthesia with sedation. Local anesthesia allows monitoring of neurological function during surgery.
-
Incision: A small incision is made along the side of the neck to expose the carotid artery.
-
Clamping: The artery is temporarily clamped to prevent blood flow to the area being operated on.
-
Plaque Removal: The surgeon carefully opens the artery and removes the atherosclerotic plaque causing the blockage.
-
Closure: The artery is closed, sometimes with a patch graft to widen it, and the incision is sutured.
-
Monitoring: Blood flow to the brain is carefully monitored throughout the procedure using specialized equipment to minimize stroke risk.
Some patients may undergo shunting, where a temporary tube diverts blood around the surgical site to maintain brain perfusion during plaque removal.
4. What are the benefits of Carotid Endarterectomy?
Carotid endarterectomy provides significant benefits for eligible patients:
-
Stroke Prevention: Dramatically reduces the risk of stroke in patients with symptomatic stenosis.
-
Improved Blood Flow: Restores adequate oxygen and nutrient supply to the brain.
-
Stabilization of Plaques: Removes unstable plaque that could rupture and cause a blockage.
-
Symptom Relief: Reduces neurological symptoms such as transient weakness, dizziness, or speech difficulties caused by impaired blood flow.
-
Long-term Protection: Helps reduce the likelihood of recurrent strokes if combined with lifestyle changes and medication management.
5. What are the risks and complications associated with Carotid Endarterectomy?
While carotid endarterectomy is generally safe, complications can occur:
Common Risks:
-
Minor bleeding or bruising at the incision site
-
Temporary nerve injury causing numbness, tingling, or mild weakness of facial muscles
-
Infection at the incision
Serious Risks:
-
Stroke (rare, but the primary risk the surgery seeks to prevent)
-
Heart attack or cardiac complications during or after surgery
-
Severe bleeding requiring additional intervention
-
Re-narrowing of the carotid artery (restenosis) over time
Risk factors: Age, pre-existing heart disease, diabetes, and severe artery narrowing may increase complication risks. Choosing an experienced vascular surgeon is key to minimizing complications.
6. How should I prepare for Carotid Endarterectomy?
Proper preparation is critical for a safe and successful procedure:
-
Medication Management: Patients may need to stop blood thinners temporarily and continue essential medications under doctor supervision.
-
Fasting: Avoid food or drink for several hours before surgery as instructed.
-
Preoperative Tests: Blood tests, ECG, carotid ultrasound, CT/MRI angiography may be performed.
-
Lifestyle Preparation: Avoid smoking and maintain hydration.
-
Transportation: Arrange for someone to drive you home or accompany you if staying overnight.
Discuss all existing medical conditions with your surgeon to optimize safety during surgery.
7. What is the recovery process like after Carotid Endarterectomy?
Recovery varies depending on individual health, but general expectations include:
-
Hospital Stay: 1-2 days for monitoring
-
Incision Care: Mild swelling or bruising is normal; the incision heals over 2-3 weeks
-
Activity Restrictions: Avoid heavy lifting or strenuous activity for several weeks
-
Follow-Up: Regular imaging or ultrasound to ensure the artery remains open and monitor for restenosis
-
Lifestyle Changes: Heart-healthy diet, regular exercise, and managing blood pressure and cholesterol are crucial for long-term success
Most patients resume normal daily activities within 2-4 weeks, with full neurological monitoring during follow-up appointments.
8. Are there alternatives to Carotid Endarterectomy?
Yes, alternatives exist depending on anatomy and patient risk:
-
Carotid Artery Stenting (CAS):
-
A minimally invasive procedure where a stent is placed inside the artery to keep it open.
-
Often preferred for patients at high risk for surgery or with complex anatomy.
-
-
Medical Management:
-
Lifestyle modifications: heart-healthy diet, exercise, smoking cessation
-
Medications: antiplatelet therapy (aspirin, clopidogrel), cholesterol-lowering drugs, blood pressure control
-
Your vascular surgeon or neurologist will recommend the safest and most effective option based on blockage severity, symptoms, and overall health.
9. What lifestyle changes are recommended after surgery?
Long-term success of carotid endarterectomy depends on preventing further plaque buildup:
-
Diet: Reduce saturated fats, trans fats, and cholesterol; increase fruits, vegetables, and whole grains
-
Exercise: Regular, moderate physical activity improves cardiovascular health
-
Quit Smoking: Smoking accelerates plaque formation and artery damage
-
Medication Adherence: Continue prescribed drugs to control cholesterol, blood pressure, and prevent clot formation
-
Routine Checkups: Regular imaging to monitor carotid arteries
These measures help ensure long-term stroke prevention and overall cardiovascular health.
10. What are the signs of complications after Carotid Endarterectomy?
After surgery, it is important to watch for:
-
Sudden weakness, numbness, or tingling in the face, arm, or leg
-
Difficulty speaking, slurred speech, or vision changes
-
Severe headache or dizziness
-
Increased swelling, redness, or bleeding at the incision site
-
Chest pain or shortness of breath
If any of these symptoms occur, seek immediate medical attention, as they may indicate a stroke or other serious complication.


