Introduction to Cataract & Glaucoma
Cataract and glaucoma are two of the most common and serious eye conditions affecting millions of people worldwide, particularly in the aging population. Both can lead to significant visual impairment and, if left untreated, permanent blindness. While they are separate diseases, cataract and glaucoma often coexist, especially in older adults, and understanding their differences and interrelationship is critical for effective diagnosis and treatment.
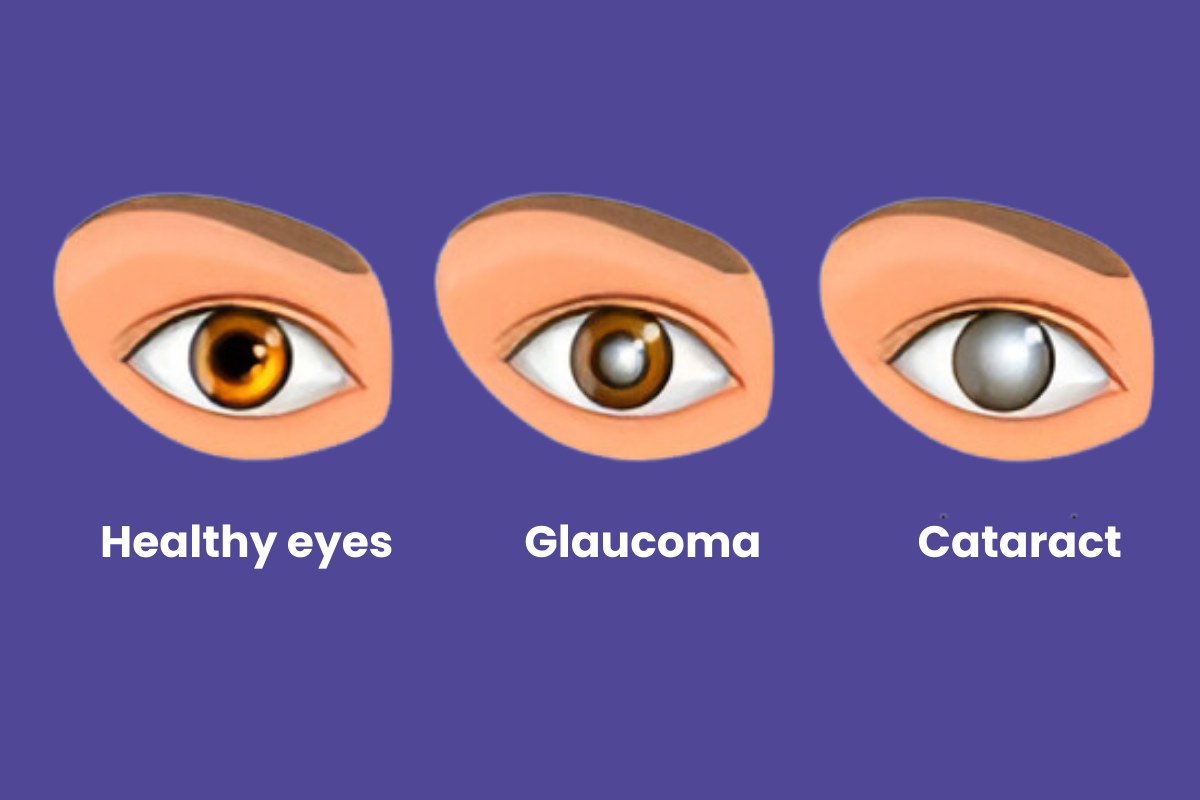
A cataract is a condition in which the natural lens of the eye becomes cloudy or opaque, leading to blurred vision, glare sensitivity, and faded colors. The lens, which normally focuses light onto the retina, loses transparency due to protein breakdown or accumulation over time. Cataract formation is usually gradual and can occur in one or both eyes.
Glaucoma, on the other hand, is a group of eye diseases that damage the optic nerve, which connects the eye to the brain. The damage is often (but not always) caused by abnormally high pressure inside the eye known as intraocular pressure (IOP). Over time, this pressure can lead to progressive and irreversible vision loss, starting from the periphery and moving inward. Glaucoma is often called the “silent thief of sight” because it may progress without noticeable symptoms until significant damage has occurred.
Both cataract and glaucoma represent leading causes of blindness globally. However, the good news is that early detection, regular eye examinations, and appropriate treatment can effectively prevent most vision loss. Cataract can be cured through surgery, while glaucoma can be controlled with medical or surgical management.
Causes and Risks of Cataract & Glaucoma
Cataract and glaucoma are two common but distinct eye conditions that can impair vision and, if left untreated, lead to blindness. Cataract primarily involves the clouding of the eye's lens, while glaucoma results from progressive optic nerve damage, often related to increased intraocular pressure (IOP). Both share lifestyle and health-related risk factors, especially aging and metabolic disorders.
Cataract Causes and Risk Factors
The most common cause of cataract is aging. As we grow older, the proteins in the lens begin to clump together, forming a cloudy area that interferes with the passage of light. However, cataracts can also develop from other causes, such as:
-
Prolonged exposure to ultraviolet (UV) rays, which accelerates the breakdown of lens proteins.
-
Diabetes mellitus, where fluctuating blood sugar levels lead to metabolic changes in the lens.
-
Smoking and excessive alcohol consumption, which increase oxidative stress in the eye.
-
Eye injuries or trauma, which can damage the lens capsule.
-
Prolonged use of corticosteroids, both oral and topical.
-
Congenital cataracts, present from birth due to genetic or maternal infections.
Risk factors include aging, poor nutrition, radiation exposure, and a family history of cataracts.
Glaucoma Causes and Risk Factors
Glaucoma develops when the delicate optic nerve fibers are damaged, usually due to elevated intraocular pressure caused by excess fluid buildup in the eye. However, not all glaucoma cases involve high pressure - in some, the nerve is more sensitive or blood supply to the optic nerve is reduced.
Major causes and risk factors include:
-
High intraocular pressure (IOP) due to poor drainage of aqueous humor.
-
Age, especially above 40 years.
-
Family history of glaucoma, as genetic predisposition plays a key role.
-
Medical conditions such as diabetes, hypertension, and thyroid disease.
-
Ethnic background, with higher prevalence in people of African and Asian descent.
-
Use of corticosteroids for long periods, which can raise eye pressure.
-
Severe eye injuries or surgeries that damage the drainage system.
When cataract and glaucoma occur together, treatment must be carefully planned because each condition affects the eye's internal pressure and vision in different ways.
Symptoms and Signs of Cataract & Glaucoma
Both cataract and glaucoma are progressive eye conditions that can lead to vision loss but differ in origin, symptoms, and reversibility. Cataracts cloud the eye's lens, blurring vision, while glaucoma damages the optic nerve, often due to increased eye pressure. Recognizing their signs early is crucial to prevent permanent vision impairment.
Symptoms of Cataract
Cataract symptoms generally develop slowly and painlessly. Many patients may not realize their vision is declining until daily activities are affected. Common symptoms include:
-
Blurry or cloudy vision, as if looking through a fogged window.
-
Sensitivity to light and glare, especially at night while driving.
-
Faded or yellowed colors, making it harder to distinguish between shades.
-
Halos around lights, especially bright lights at night.
-
Frequent changes in eyeglass prescription as the lens opacity progresses.
-
Double vision in one eye in advanced cases.
Cataract does not cause eye pain or redness, and vision loss is typically reversible with surgery.
Symptoms of Glaucoma
Glaucoma can present in several forms, but open-angle glaucoma and angle-closure glaucoma are the most common.
-
Open-angle glaucoma progresses slowly and painlessly. Symptoms appear late and include gradual loss of side (peripheral) vision, tunnel vision in advanced stages, and difficulty adjusting to darkness.
-
Angle-closure glaucoma, on the other hand, can appear suddenly and is a medical emergency. Symptoms include severe eye pain, headache, nausea, blurred vision, halos around lights, and redness of the eye.
Because early glaucoma is often symptomless, routine eye exams are the only way to detect it before significant vision loss occurs.
Diagnosis of Cataract & Glaucoma
The diagnosis of cataract and glaucoma requires specific ophthalmic examinations that evaluate the lens, retina, optic nerve, and intraocular pressure. While cataracts are diagnosed by identifying lens opacities, glaucoma diagnosis focuses on detecting optic nerve damage and abnormal fluid pressure within the eye.
Cataract Diagnosis
Diagnosis of cataract is straightforward and involves a comprehensive eye examination. Key diagnostic procedures include:
-
Visual acuity testing, to measure clarity of vision.
-
Slit-lamp examination, to visualize the clouding of the lens.
-
Retinal examination, to ensure the retina and optic nerve are healthy.
-
Contrast sensitivity tests, to determine how cataract affects vision in dim light or glare.
-
Biometry, if surgery is planned, to calculate the correct power of the artificial intraocular lens (IOL) implant.
Glaucoma Diagnosis
Diagnosing glaucoma requires more specialized testing since optic nerve damage must be detected before major vision loss occurs. Tests include:
-
Tonometry, which measures intraocular pressure.
-
Ophthalmoscopy, to inspect the optic nerve for thinning or cupping.
-
Perimetry (visual field test), to check for blind spots in peripheral vision.
-
Optical Coherence Tomography (OCT), which provides high-resolution images of the optic nerve and retinal nerve fiber layer.
-
Gonioscopy, used to examine the drainage angle of the eye and determine the type of glaucoma.
Because cataracts can sometimes make it difficult to perform detailed glaucoma testing, ophthalmologists may treat one condition first before accurately monitoring the other.
Treatment Options for Cataract & Glaucoma
Cataract and glaucoma treatments in 2025 have advanced considerably, combining surgical precision, artificial intelligence (AI), and minimally invasive techniques to enhance safety and visual outcomes. Cataract treatment primarily replaces the clouded lens, while glaucoma management focuses on lowering intraocular pressure (IOP) to prevent optic nerve damage.
Cataract Treatment
In the early stages, cataracts can be managed with lifestyle modifications such as using stronger lighting, magnifying lenses, or updated eyeglass prescriptions. However, as the lens clouding advances and vision deteriorates, surgery becomes necessary.
Cataract surgery is one of the most common and safest procedures worldwide. During surgery, the cloudy natural lens is removed and replaced with a clear artificial intraocular lens (IOL). Modern techniques include phacoemulsification, where ultrasound waves break up the cloudy lens for removal through a tiny incision. The recovery is quick, painless, and restores vision almost immediately.
Glaucoma Treatment
Unlike cataract, the damage caused by glaucoma is irreversible - but early and proper treatment can slow or stop further vision loss. Treatment focuses on reducing intraocular pressure (IOP):
-
Eye drops to reduce fluid production or increase drainage (prostaglandin analogs, beta blockers, alpha agonists, carbonic anhydrase inhibitors).
-
Laser therapy, such as selective laser trabeculoplasty (SLT), which improves fluid outflow.
-
Surgical options, including trabeculectomy, tube shunt surgery, and minimally invasive glaucoma surgeries (MIGS).
-
In patients with both conditions, combined cataract-glaucoma surgery may be recommended to treat both issues in one procedure.
Prevention and Management of Cataract & Glaucoma
Both cataract and glaucoma are leading global causes of visual impairment, but they differ in their nature - cataracts cause lens opacity that can be surgically removed, while glaucoma damages the optic nerve irreversibly. Prevention emphasizes lifestyle, regular screening, and early intervention, while management depends on disease stage and technology-driven treatment approaches.
Preventing Cataract
-
Protect your eyes from UV exposure by wearing sunglasses and hats.
-
Maintain good control of diabetes and systemic health.
-
Avoid smoking and excessive alcohol consumption.
-
Eat a diet rich in antioxidants, vitamins A, C, and E, leafy greens, and omega-3 fatty acids.
-
Get regular eye checkups, especially after age 40.
Preventing Glaucoma
-
Regular eye exams to detect early IOP changes and optic nerve damage.
-
Know your family history, as genetics play a role.
-
Maintain healthy blood pressure and blood sugar levels.
-
Avoid self-medicating with steroid eye drops unless prescribed.
-
Stay physically active, as moderate exercise supports healthy eye pressure.
Ongoing Management
After treatment or surgery, regular follow-up visits are crucial. For cataract patients, eye health must be monitored to prevent infection or lens capsule opacification. For glaucoma patients, adherence to prescribed medications and regular pressure monitoring are essential for maintaining vision.
Complications of Cataract & Glaucoma
Both cataract surgery and glaucoma management generally have high success rates with modern ophthalmic technology. However, they can be associated with certain short-term and long-term complications, some minor and others vision-threatening.
Cataract Complications
Although cataract surgery is highly successful, potential complications include infection, inflammation, swelling, bleeding, dislocation of the IOL, and posterior capsule opacification (secondary cataract). Fortunately, these are rare and treatable with prompt medical attention.
Glaucoma Complications
If untreated or poorly controlled, glaucoma can cause irreversible optic nerve damage, leading to partial or complete blindness. Surgical treatments carry their own risks, such as infection, bleeding, or excessive lowering of eye pressure, but these are generally well-managed under expert care.
When both cataract and glaucoma exist, surgery must be carefully planned. Cataract surgery can sometimes lower eye pressure, but in other cases, it may worsen glaucoma temporarily if not monitored properly.
Living with Cataract & Glaucoma
Living with cataract and glaucoma requires a combination of medical adherence, lifestyle awareness, and consistent ophthalmic care. Both are chronic visual conditions, and while cataracts are curable with surgery, glaucoma is a lifelong condition requiring continuous pressure management to protect optic nerve health.
After cataract surgery:
-
Many patients experience marked improvement in vision and quality of life. Recoveries are rapid with modern techniques (outpatient, minimal discomfort).
-
Post-operative care: protect the eye from injury, follow-up visits, correct glasses as needed, manage other eye diseases.
With glaucoma:
-
Because glaucoma is a chronic condition, patients need ongoing care—medication adherence, regular check-ups, visual-field and optic-nerve monitoring.
-
Vision-rehabilitation: If glaucoma has caused vision loss, patients may benefit from low-vision aids, field-loss awareness, occupational therapy.
Living positively:
-
Despite these eye diseases, many people lead normal, active lives with appropriate treatment and care. Emphasise that early diagnosis and timely management lead to better outcomes.
-
Practical lifestyle advice: protect your eyes (UV, injury), maintain general health (blood pressure, diabetes), avoid habits that may raise eye pressure, adapt home/office lighting for cataract or glaucoma-related challenges (glare, contrast sensitivity).
-
Patient empowerment: Understand your eye condition, know your IOP targets (in glaucoma), ask your ophthalmologist about combined cataract-glaucoma strategies, keep a written record of eye-drops and follow-up schedule, and report any new symptoms (e.g., sudden vision change, eye pain).
- Supportive resources: local support groups, vision rehabilitation services, educational materials and regular communication with your eye-care provider.
Top 10 Frequently Asked Questions about Cataract & Glaucoma
1. What is Cataract & Glaucoma Surgery?
Cataract & Glaucoma Surgery is a combined procedure that addresses both cataracts and glaucoma in a single operation. Cataract surgery involves removing the clouded lens of the eye and replacing it with a clear artificial lens. Glaucoma surgery aims to reduce intraocular pressure (IOP) to prevent damage to the optic nerve. Combining these surgeries can be beneficial for patients who have both conditions simultaneously.
2. Why is Combined Surgery Recommended?
Combining cataract and glaucoma surgery offers several advantages:
-
Reduced Surgical Burden: Undergoing one procedure instead of two minimizes overall surgical risk and recovery time.
-
Improved Medication Adherence: Patients may require fewer glaucoma medications post-surgery.
-
Enhanced Visual Outcomes: Addressing both conditions simultaneously can lead to better overall vision quality.
Studies have shown that combining cataract and glaucoma surgery can lead to improved intraocular pressure control and visual outcomes compared to performing the surgeries separately.
3. Who is a Candidate for Combined Surgery?
Ideal candidates for combined cataract and glaucoma surgery include:
-
Patients with both cataracts and glaucoma.
-
Individuals whose glaucoma is not adequately controlled with medication.
-
Patients with mild to moderate glaucoma and significant cataract-induced vision impairment.
A thorough eye examination and assessment by an ophthalmologist are necessary to determine suitability for combined surgery.
4. What Are the Types of Glaucoma Procedures Used in Combination?
Several minimally invasive glaucoma surgeries (MIGS) can be performed alongside cataract surgery:
-
iStent: A small device implanted to improve fluid drainage and reduce IOP.
-
Hydrus Microstent: A larger device that dilates Schlemm's canal to enhance aqueous humor outflow.
-
Kahook Dual Blade: A surgical instrument that removes trabecular tissue to facilitate fluid drainage.
-
XEN Gel Stent: A tube inserted to create a drainage pathway for aqueous humor.
The choice of procedure depends on the type and severity of glaucoma, as well as individual patient factors.
5. How Is the Combined Surgery Performed?
The combined procedure typically involves:
-
Anesthesia: Local anesthesia is administered to numb the eye.
-
Cataract Surgery: The clouded lens is removed, and an intraocular lens (IOL) is implanted.
-
Glaucoma Procedure: A MIGS device or technique is employed to reduce IOP.
-
Closure: The incision is closed, and a protective shield is placed over the eye.
The entire procedure usually takes about 30 to 60 minutes and is performed on an outpatient basis.
6. What Are the Benefits of Combined Surgery?
Benefits include:
-
Single Recovery Period: Eliminates the need for separate recovery times.
-
Cost-Effective: Reduces overall medical expenses.
-
Enhanced Vision: Improves both clarity and field of vision.
-
Reduced Medication Use: May decrease the need for glaucoma medications post-surgery.
Patients often experience improved quality of life due to better vision and reduced reliance on medications.
7. What Are the Risks and Complications?
As with any surgery, risks include:
-
Infection: Postoperative infections can occur.
-
Increased IOP: Elevated eye pressure may persist or recur.
-
Vision Changes: Temporary blurred vision or glare.
-
Bleeding or Swelling: Rare but possible complications.
Discussing potential risks with your ophthalmologist helps in making an informed decision.
8. What Is the Recovery Process?
Post-surgery recovery typically involves:
-
Rest: Avoiding strenuous activities for a few weeks.
-
Medications: Using prescribed eye drops to prevent infection and reduce inflammation.
-
Follow-Up Visits: Regular check-ups to monitor healing and IOP.
Most patients resume normal activities within 1 to 2 weeks, with full recovery taking up to 4 to 6 weeks.
9. Will I Still Need Glaucoma Medications After Surgery?
Some patients may experience a reduction or elimination of the need for glaucoma medications following combined surgery. However, others may still require medication to maintain optimal IOP control. Your ophthalmologist will monitor your condition and adjust treatment as necessary.
10. How Can I Prepare for Combined Cataract & Glaucoma Surgery?
Preparation steps include:
-
Preoperative Testing: Undergoing eye exams and imaging studies.
-
Medication Review: Discussing current medications with your
doctor.
-
Postoperative Care Plan: Arranging for assistance at home during
recovery.
-
Lifestyle Adjustments: Avoiding certain activities as advised by
your surgeon.
Following your ophthalmologist's instructions ensures the best possible outcome.
Preoperative Testing: Undergoing eye exams and imaging studies.
Medication Review: Discussing current medications with your doctor.
Postoperative Care Plan: Arranging for assistance at home during recovery.
Lifestyle Adjustments: Avoiding certain activities as advised by your surgeon.


