Introduction to Cervical Cancer Surgery
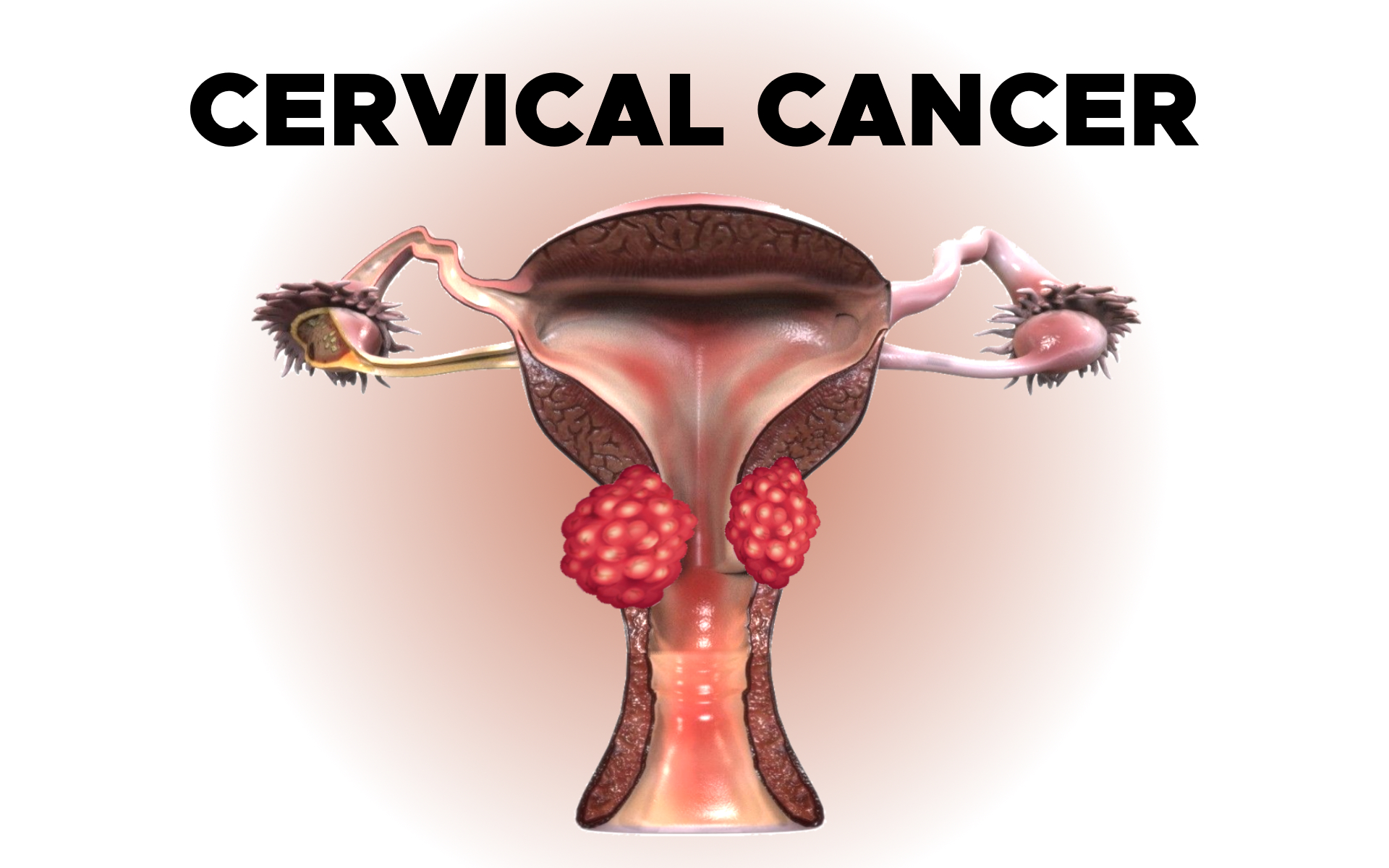
Cervical cancer is one of the most common cancers affecting women worldwide, particularly in developing nations where screening and vaccination programs are limited. It originates in the cervix, the lower part of the uterus that connects to the vagina. The disease develops gradually, often beginning as pre-cancerous changes called dysplasia before progressing into invasive cancer if left untreated.
Cervical cancer surgery plays a pivotal role in the treatment and management of this condition. In early stages, surgery may be curative, while in advanced cases, it is often part of a combined approach that includes radiation and chemotherapy. The primary goal of surgery is to completely remove the cancerous tissue, prevent further spread, and in some cases, preserve fertility when possible.
The type and extent of surgery depend on various factors, including the stage of the cancer, tumor size, patient's age, overall health, and desire for future pregnancy. Modern surgical techniques, ranging from conservative cone biopsies to radical hysterectomies, offer patients improved outcomes with fewer complications. Minimally invasive approaches, such as laparoscopic and robotic-assisted surgeries, are increasingly being used where appropriate, though open surgery remains standard for certain stages.
With advances in early detection through Pap smears, HPV testing, and vaccination, the need for extensive surgery is declining — highlighting the importance of prevention and timely medical care.
Causes and Risk Factors of Cervical Cancer
Cervical cancer is primarily caused by persistent infection with high-risk strains of the Human Papillomavirus (HPV). HPV is a common sexually transmitted infection, and while most infections resolve spontaneously, persistent infection with certain high-risk types (especially HPV-16 and HPV-18) can cause changes in cervical cells that lead to cancer over time.
Major Causes and Risk Factors Include:
-
Human Papillomavirus (HPV) Infection: The most significant cause; responsible for more than 90% of cervical cancer cases.
-
Smoking: Tobacco use doubles the risk of cervical cancer by damaging the DNA of cervical cells and weakening the immune system.
-
Weakened Immune System: Women with HIV or those on long-term immunosuppressive drugs have a higher risk of developing cervical cancer.
-
Multiple Sexual Partners or Early Sexual Activity: Increases exposure to HPV infection.
-
Long-Term Oral Contraceptive Use: Extended use (more than five years) slightly increases risk.
-
Poor Hygiene and Socioeconomic Factors: Limited access to healthcare and lack of awareness lead to delayed detection.
-
Family History: Genetic predisposition can increase risk in some women.
Understanding these factors is vital because risk reduction strategies—such as HPV vaccination, regular screening, and lifestyle modifications—can prevent most cases of cervical cancer, minimizing the need for invasive surgical treatment.
Symptoms and Signs of Cervical Cancer
Cervical cancer often develops silently and may not cause noticeable symptoms in its early stages. This is why regular screening is essential. When symptoms do appear, they may indicate that the disease has progressed.
Common Symptoms Include:
-
Abnormal Vaginal Bleeding: This is the most common early sign. It may occur between menstrual periods, after sexual intercourse, or after menopause.
-
Unusual Vaginal Discharge: Watery, bloody, or foul-smelling discharge may occur due to tissue breakdown and infection.
-
Pelvic Pain: Persistent lower abdominal or pelvic pain, particularly during intercourse, can be a warning sign.
-
Pain During Urination or Bowel Movements: These may appear when the cancer has spread locally to surrounding organs.
-
Swelling or Pain in the Legs: Occurs when the tumor presses on pelvic nerves or lymph nodes.
In more advanced cases, symptoms may include weight loss, fatigue, and loss of appetite. Any persistent or unusual symptom warrants immediate medical evaluation. Early detection through Pap tests or HPV screening can identify precancerous changes long before symptoms appear, allowing treatment through less extensive surgery.
Diagnosis of Cervical Cancer Surgery
The diagnosis of cervical cancer involves multiple steps to confirm the presence of cancer, determine its type, and establish how far it has spread (staging). Accurate diagnosis and staging are crucial for planning the appropriate surgical approach.
Key Diagnostic Methods:
-
Pap Smear (Pap Test): A screening test that detects abnormal cervical cells before they become cancerous.
-
HPV Testing: Identifies high-risk HPV types that can cause cervical cancer.
-
Colposcopy: A specialized visual examination of the cervix using a colposcope to identify abnormal areas for biopsy.
-
Biopsy: Removal of a small tissue sample from the cervix for microscopic analysis to confirm cancer.
-
Imaging Studies: MRI, CT scan, and PET scan are used to determine the extent of the disease and whether it has spread to nearby tissues or lymph nodes.
-
Pelvic Examination Under Anesthesia: In some cases, doctors perform an examination to evaluate tumor size and spread.
Cervical cancer is staged according to the FIGO system (International Federation of Gynecology and Obstetrics), ranging from Stage 0 (pre-cancerous lesions) to Stage IV (cancer spread to distant organs). Surgery is typically recommended for early stages (IA to IIA), while advanced stages may require a combination of radiation and chemotherapy.
Treatment Options - Types of Cervical Cancer Surgery
The choice of surgery depends on the cancer's stage, size, and patient's reproductive goals. Here are the major surgical procedures used in cervical cancer treatment:
1. Cone Biopsy (Conization)
A small, cone-shaped piece of tissue is removed from the cervix using a scalpel, laser, or loop electrosurgical excision procedure (LEEP). It is both diagnostic and therapeutic for very early cancers (Stage 0 or IA1) and can preserve fertility.
2. Simple Hysterectomy
Removes the uterus and cervix. It's recommended for very early-stage cancers or pre-cancerous lesions that cannot be treated conservatively. Fertility is lost after this procedure.
3. Radical Hysterectomy
This is the most common surgery for early-stage invasive cervical cancer. It involves removing the uterus, cervix, part of the vagina, and nearby tissues (parametrium), often with pelvic lymph node removal. It offers high cure rates when cancer is confined to the cervix.
4. Radical Trachelectomy
A fertility-sparing procedure for women with small, early-stage tumors who wish to become pregnant in the future. It involves removing the cervix and nearby lymph nodes but leaving the uterus intact.
5. Pelvic Exenteration
A highly complex surgery used in cases of recurrent or advanced cervical cancer limited to the pelvic area. It may involve removal of the uterus, cervix, vagina, bladder, and part of the rectum. It is typically considered only after other treatments have failed.
6. Lymph Node Dissection
Often performed along with major surgeries to assess cancer spread. Lymph nodes in the pelvis are examined to determine whether additional treatments are required.
Surgery is often followed by adjuvant therapy—such as radiation or chemotherapy—if cancer cells are found at the margins or lymph nodes.
Prevention and Management of Cervical Cancer Surgery
Prevention
Preventing cervical cancer begins with understanding its causes and addressing them through simple yet powerful public health measures:
-
HPV Vaccination: The HPV vaccine protects against the strains most likely to cause cervical cancer. Vaccination is most effective when given before sexual activity begins, typically to girls aged 9-14.
-
Regular Screening: Routine Pap and HPV tests can detect abnormal cells early, allowing prompt treatment before cancer develops.
-
Safe Sexual Practices: Using protection and limiting the number of sexual partners reduces HPV exposure.
-
Smoking Cessation: Quitting smoking lowers risk significantly.
-
Boosting Immunity: Maintaining a healthy lifestyle and managing conditions like HIV improves immune defense against HPV infections.
Management After Surgery
Proper post-operative management is essential for recovery and long-term health. This includes:
-
Hospital Stay and Recovery: Most patients stay in the hospital for 3-7 days, depending on the surgery. Full recovery may take several weeks.
-
Wound Care: Proper hygiene, avoiding heavy lifting, and following doctor's instructions prevent infection.
-
Emotional and Physical Support: Counseling, physiotherapy, and nutrition play crucial roles in recovery.
-
Follow-Up Visits: Regular check-ups every 3-6 months for the first two years, then annually, help detect recurrences early.
Complications of Cervical Cancer Surgery
Every surgical procedure carries some risks. While cervical cancer surgery is generally safe and effective, patients should be aware of potential complications.
Short-Term Complications:
-
Excessive bleeding or infection
-
Damage to nearby organs (bladder, bowel, ureters)
-
Deep vein thrombosis (blood clots)
-
Pain, fatigue, or temporary urinary problems
Long-Term Complications:
-
Fertility Loss: After hysterectomy or radical surgery, pregnancy becomes impossible.
-
Early Menopause: Removal of ovaries or damage to blood supply may trigger premature menopause.
-
Bladder or Bowel Dysfunction: Nerve damage during surgery can cause incontinence or constipation.
-
Sexual Dysfunction: Vaginal shortening, dryness, or pain during intercourse may occur.
-
Lymphedema: Swelling of the legs due to lymph node removal.
-
Emotional Impact: Anxiety, depression, and body image issues can affect quality of life.
Prompt management, physical therapy, and emotional support can help overcome most of these issues, improving the patient's overall well-being.
Living with Cervical Cancer After Surgery
Life after cervical cancer surgery involves both physical and emotional healing. Most women who undergo successful surgery for early-stage cancer go on to live long, healthy lives.
Key Aspects of Long-Term Care:
-
Regular Follow-Up: Routine pelvic exams, imaging, and Pap tests (if part of the cervix remains) are crucial for early detection of recurrence.
-
Fertility Considerations: Women who undergo fertility-sparing surgery should discuss pregnancy plans with specialists. High-risk pregnancies require close monitoring.
-
Hormone Management: Hormone replacement therapy may help relieve menopausal symptoms after ovary removal.
-
Physical Rehabilitation: Gentle exercises, pelvic floor therapy, and maintaining a healthy weight aid recovery.
-
Emotional and Mental Health: Support groups, counseling, and family involvement play a major role in emotional healing.
-
Lifestyle Modifications: A balanced diet, regular exercise, adequate sleep, and avoiding smoking and alcohol enhance recovery and reduce recurrence risk.
Living with and beyond cervical cancer is not only about physical recovery—it's also about regaining confidence, maintaining intimacy, and restoring overall wellness.
Top 10 Frequently Asked Questions about Cervical Cancer Surgery
1. What is Cervical Cancer Surgery and why is it performed?
Cervical cancer surgery is a medical procedure aimed at removing cancerous tissue from the cervix, the lower portion of the uterus that connects to the vagina. Surgery may be performed alone or in combination with radiation or chemotherapy depending on the stage of cancer.
Purpose of the surgery:
-
Remove cancerous cells and reduce the risk of spreading.
-
Preserve as much healthy tissue as possible.
-
Improve long-term survival and quality of life.
-
Relieve symptoms such as abnormal bleeding, pain, or pelvic discomfort.
There are different types of surgeries for cervical cancer depending on tumor size, cancer stage, and the patient's desire to preserve fertility.
2. What are the types of Cervical Cancer Surgery?
Surgical options vary based on the stage of cancer:
-
Conization (Cone Biopsy)
-
Removes a cone-shaped piece of the cervix containing cancerous tissue.
-
Often used in early-stage cancer.
-
Can preserve fertility.
-
-
Simple Hysterectomy
-
Removes the uterus and cervix.
-
Typically used for very early-stage cancer confined to the cervix.
-
-
Radical Hysterectomy
-
Removes the uterus, cervix, surrounding tissues, part of the vagina, and sometimes lymph nodes.
-
Recommended for more advanced localized cancers.
-
-
Trachelectomy (Fertility-Preserving Surgery)
-
Removes the cervix while preserving the uterus.
-
Suitable for younger women who wish to maintain fertility.
-
-
Lymph Node Dissection
-
Often performed alongside hysterectomy to check for cancer spread.
-
-
Minimally Invasive Surgery (Laparoscopy/Robotic Surgery)
-
Uses small incisions and specialized instruments for precise removal of cancer.
-
Shorter recovery time and less post-operative pain.
-
3. Who is a candidate for Cervical Cancer Surgery?
Surgery is most effective for early-stage cervical cancer (Stages I-II). Candidates usually:
-
Are in good overall health and can tolerate anesthesia.
-
Have cancer confined to the cervix or localized tissues.
-
Desire fertility preservation (for trachelectomy).
Advanced-stage cervical cancer may require chemotherapy, radiation, or a combination before or instead of surgery.
Your oncologist will perform a thorough evaluation, including imaging tests, biopsies, and blood work, to determine the best surgical approach.
4. How is Cervical Cancer Surgery performed?
Surgical techniques depend on the type and stage of cancer:
-
Open Surgery (Laparotomy): Traditional abdominal incision to access the uterus and surrounding tissues.
-
Minimally Invasive Surgery (Laparoscopy/Robotic): Small incisions with a camera and robotic instruments allow precise removal of cancerous tissue.
-
Vaginal Approach: Certain hysterectomies or trachelectomies may be performed through the vagina.
During surgery, the surgeon removes cancerous tissue, checks lymph nodes for metastasis, and reconstructs affected areas as needed. Procedures may last 2-6 hours depending on complexity.
5. What are the risks and complications of Cervical Cancer Surgery?
While generally safe, cervical cancer surgery carries some risks:
-
Bleeding during or after surgery.
-
Infection at the surgical site or urinary tract.
-
Injury to nearby organs, such as the bladder, ureters, or rectum.
-
Urinary or bowel dysfunction post-surgery.
-
Blood clots in the legs or lungs (deep vein thrombosis or pulmonary embolism).
-
Fertility loss, depending on the type of surgery.
-
Emotional distress, as patients may struggle with changes to body image or reproductive capability.
Careful pre-operative planning, skilled surgeons, and post-operative care minimize these risks.
6. How long is the recovery period after Cervical Cancer Surgery?
Recovery depends on the type of surgery and individual health:
-
Minimally invasive procedures: 2-4 weeks.
-
Open radical hysterectomy: 6-8 weeks.
-
Fertility-preserving procedures: Recovery similar to minimally invasive surgeries but may require additional monitoring.
During recovery, patients may experience:
-
Fatigue and mild pain.
-
Changes in urinary or bowel habits.
-
Emotional and psychological adjustments.
Follow-up visits are essential for monitoring healing, detecting recurrence, and managing side effects.
7. Will I lose fertility after Cervical Cancer Surgery?
Fertility impact depends on the type of surgery:
-
Trachelectomy: Preserves the uterus; patients may conceive after recovery.
-
Simple or Radical Hysterectomy: Removes the uterus, resulting in permanent loss of fertility.
Women wishing to preserve fertility should discuss all surgical options with their oncologist and consider alternatives like egg or embryo preservation before surgery.
8. What is the success rate of Cervical Cancer Surgery?
Cervical cancer surgery is highly effective for early-stage disease:
-
Stage I: 5-year survival rates exceed 90%.
-
Stage II: 5-year survival rates range from 70-80%.
-
Success depends on tumor size, lymph node involvement, and overall health.
-
Combined treatment with radiation or chemotherapy may improve outcomes in more advanced cases.
9. Are there alternatives to Cervical Cancer Surgery?
Alternatives may include:
-
Radiation Therapy: Often used for early-stage inoperable tumors or as adjuvant therapy.
-
Chemotherapy: For advanced-stage disease, sometimes combined with radiation.
-
Targeted Therapy: For specific genetic profiles in advanced or recurrent cancers.
The choice depends on cancer stage, tumor location, patient health, and fertility considerations.
10. How can I prepare for Cervical Cancer Surgery?
Proper preparation helps ensure a successful procedure:
-
Pre-operative Testing: Imaging scans, blood tests, and anesthetic evaluation.
-
Medication Review: Certain medications, especially blood thinners, may need adjustment.
-
Lifestyle Modifications: Healthy diet, exercise, and quitting smoking.
-
Emotional Preparation: Counseling or support groups may help cope with fertility loss and post-surgery recovery.
-
Post-Operative Planning: Arrange for support at home during the recovery period.
Following your surgeon's instructions carefully maximizes recovery and reduces complications.


