Introduction to Chemoembolization
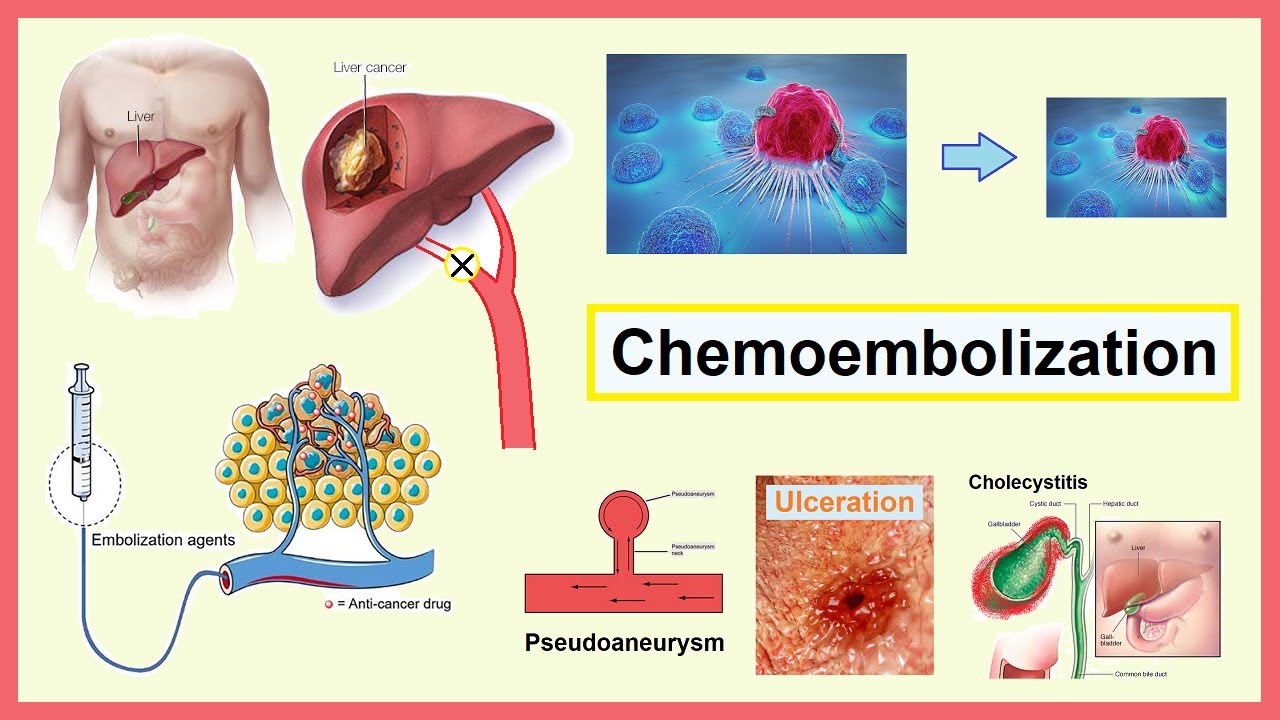
Chemoembolization, also known as Transarterial Chemoembolization (TACE), is a minimally invasive, targeted therapy used primarily to treat liver cancer and certain metastatic tumours that spread to the liver. Unlike traditional chemotherapy that travels throughout the body, chemoembolization delivers high doses of chemotherapy drugs directly to the tumour while blocking its blood supply. This dual action - chemotherapy plus embolization - helps destroy cancer cells while sparing most of the surrounding healthy liver tissue.
The procedure is performed by an interventional radiologist using imaging guidance. A thin, flexible catheter is inserted into a blood vessel (usually in the groin or wrist) and guided through the arteries to reach the hepatic artery feeding the tumour. Once the catheter is in position, a mixture of chemotherapy medication and embolic particles (tiny beads or an oily solution) is injected. The embolic material blocks the blood flow to the tumour, trapping the chemotherapy inside and depriving the tumour of oxygen and nutrients.
Chemoembolization is most commonly used for patients with hepatocellular carcinoma (HCC), the most common type of primary liver cancer, especially when surgery or liver transplantation is not an option. It may also be used to treat secondary liver cancers, where tumours have spread from other organs such as the colon, pancreas, or breast.
This treatment offers several advantages - it prolongs survival, reduces symptoms, and improves quality of life in patients with intermediate or advanced liver cancer. It can also be repeated several times depending on the patient's condition and tumour response. Over the years, new techniques like Drug-Eluting Bead TACE (DEB-TACE) have been developed, improving safety and effectiveness by allowing the chemotherapy drug to be released slowly and steadily at the tumour site.
Causes and Risk of Chemoembolization
Chemoembolization is not a disease but a treatment - therefore, understanding what causes the underlying condition helps explain why the procedure may be necessary. The primary disease that leads to the need for chemoembolization is liver cancer, most commonly hepatocellular carcinoma (HCC).
The main causes and risk factors for liver cancer include:
-
Chronic viral infections such as Hepatitis B and Hepatitis C, which cause long-term liver inflammation and damage.
-
Cirrhosis of the liver, regardless of its cause, which increases the risk of developing cancer. Cirrhosis may result from alcohol abuse, fatty liver disease, or viral hepatitis.
-
Non-Alcoholic Fatty Liver Disease (NAFLD) and its advanced form, non-alcoholic steatohepatitis (NASH), which are increasingly common due to obesity and diabetes.
-
Exposure to toxins, such as aflatoxins found in contaminated grains, can also trigger mutations leading to liver cancer.
-
Inherited liver diseases, including hemochromatosis (iron overload) and Wilson's disease (copper buildup).
Patients who develop liver tumours but are not suitable for surgical resection or liver transplantation are the typical candidates for chemoembolization. The treatment is also offered to patients with multiple small tumours that cannot all be removed surgically or when the cancer has not spread outside the liver.
Certain factors influence the success and safety of chemoembolization, including the overall health of the liver, the size and number of tumours, the presence of portal vein thrombosis, and the patient's general condition. Selecting patients carefully based on these parameters helps maximize the treatment benefit and minimize complications.
Symptoms and Signs of Chemoembolization
Patients who undergo chemoembolization usually have symptoms related to the underlying liver tumour rather than the procedure itself. In early stages, liver cancer may not cause any symptoms, but as it grows, several noticeable signs may develop:
-
Persistent pain or a feeling of fullness in the upper right side of the abdomen
-
Unexplained weight loss and loss of appetite
-
Fatigue and weakness
-
Nausea and vomiting
-
Yellowing of the skin and eyes (jaundice)
-
Swelling in the abdomen due to fluid accumulation (ascites)
-
Itchy skin and dark-colored urine
These symptoms indicate a disturbance in liver function or an expanding tumour pressing on nearby structures.
After the chemoembolization procedure, patients may develop what is known as Post-Embolization Syndrome, a temporary reaction due to the tumour's response to treatment. This includes fever, abdominal pain, nausea, vomiting, fatigue, and poor appetite, usually lasting a few days. These side effects are typically managed with medications and rest.
It's important for patients to report severe or persistent symptoms such as worsening pain, high fever, jaundice, confusion, or significant swelling, as they could indicate complications that need immediate attention.
Diagnosis of Chemoembolization
The decision to perform chemoembolization is based on careful diagnostic evaluation and imaging to determine the tumour's size, location, number, and impact on liver function.
A. Diagnostic Imaging
-
Ultrasound (US): Often the first step in detecting liver lesions.
-
Computed Tomography (CT) Scan: Provides detailed cross-sectional images, helping to assess tumour extent and blood supply.
-
Magnetic Resonance Imaging (MRI): Offers excellent soft-tissue contrast to differentiate tumour tissue from healthy liver.
-
Angiography: A special X-ray that visualizes the blood vessels feeding the tumour, crucial for planning TACE.
B. Laboratory Tests
-
Liver Function Tests (LFTs): Measure bilirubin, ALT, AST, albumin, and prothrombin time to evaluate hepatic performance.
-
Alpha-Fetoprotein (AFP): Elevated in many liver cancer cases, serving as a tumour marker.
-
Kidney Function Tests: Ensure safe contrast dye use.
-
Complete Blood Count (CBC): To evaluate overall health and readiness for the procedure.
C. Clinical Evaluation
Doctors also evaluate the patient's general condition, nutritional status, and degree of liver cirrhosis. The Barcelona Clinic Liver Cancer (BCLC) staging system is commonly used to determine if TACE is the optimal therapy.
Patients with well-compensated liver disease and tumours confined to the liver typically benefit the most from chemoembolization.
Treatment Options of Chemoembolization
The chemoembolization procedure is typically performed in a hospital's interventional radiology suite under local anesthesia and mild sedation. The process can take one to three hours, depending on tumour complexity.
Here's how the procedure generally works:
-
The interventional radiologist inserts a small catheter into an artery (usually in the groin or wrist).
-
Using live X-ray imaging, the catheter is carefully guided through the arteries to reach the hepatic artery that supplies blood to the tumour.
-
A mixture of chemotherapy drugs and embolic materials is injected. The embolic agents block the blood flow to the tumour, trapping the chemotherapy and causing tumour cells to die.
-
Once the embolization is complete, the catheter is removed, and the insertion site is bandaged.
Two main types of TACE are used:
-
Conventional TACE (cTACE): Involves injecting chemotherapy mixed with an oily contrast medium (such as Lipiodol) followed by particles that block the blood flow.
-
Drug-Eluting Bead TACE (DEB-TACE): Uses microspheres loaded with chemotherapy that slowly release the drug over time, providing longer tumour exposure and fewer systemic side effects.
After the procedure, patients are monitored for several hours or overnight. Most can go home within 24-48 hours, though some may need a longer stay depending on recovery.
Prevention and Management of Chemoembolization
Preventing the need for chemoembolization begins with preventing liver disease and detecting liver cancer early. Key preventive strategies include:
-
Vaccination and treatment for hepatitis B and C infections.
-
Avoiding alcohol abuse and maintaining a healthy weight to prevent fatty liver disease.
-
Regular liver screening for people with chronic liver conditions.
-
Eating a balanced diet rich in fruits, vegetables, and whole grains while avoiding foods contaminated with mould or toxins.
Before the procedure, doctors optimize liver function and overall health. Patients are advised to stop certain medications that may increase bleeding risk and to stay well hydrated.
After chemoembolization, management focuses on recovery and liver protection:
-
Medications for pain, fever, and nausea.
-
Adequate rest and hydration.
-
Follow-up imaging to monitor tumour response and detect recurrence.
-
Avoiding alcohol and maintaining good nutrition to support liver healing.
If the cancer responds well, the procedure can be repeated after a few months to further control the tumour.
Complications of Chemoembolization
Chemoembolization is a safe procedure when performed by experienced specialists, but like all medical interventions, it carries potential risks. The most common side effect is Post-Embolization Syndrome, which includes mild fever, nausea, fatigue, and abdominal discomfort that resolve within a few days.
More serious, though less frequent, complications include:
-
Liver failure or worsening liver function, especially in patients with advanced cirrhosis.
-
Biliary injury, such as bile duct inflammation or blockage.
-
Non-target embolization, where embolic particles reach other organs accidentally, causing tissue damage.
-
Infection or abscess formation within the liver.
-
Bleeding or vascular injury at the catheter insertion site.
-
Kidney dysfunction due to the contrast dye used during the procedure.
Most of these complications can be managed effectively with prompt medical attention. Close monitoring after the procedure helps detect and address issues early.
Living with the Condition of Chemoembolization
Living with liver cancer and undergoing chemoembolization can be physically and emotionally demanding. However, many patients continue to live fulfilling lives with proper medical care and lifestyle management.
A. Lifestyle Recommendations
-
Follow a liver-friendly diet rich in vegetables, lean proteins, and whole grains. Avoid fried, processed, and oily foods.
-
Avoid alcohol and unnecessary medications that strain the liver.
-
Stay physically active with light exercises like walking or yoga.
-
Get adequate sleep and manage stress through relaxation techniques or counselling.
B. Regular Medical Follow-up
After chemoembolization, periodic imaging (CT or MRI) is performed to assess tumour response. Blood tests track liver function and tumour markers. Depending on the outcome, further TACE sessions or combination therapies may be planned.
C. Emotional Support
Dealing with cancer treatment can be emotionally challenging. Support groups, counselling, and open communication with family and doctors can greatly help improve quality of life.
Top 10 Frequently Asked Questions about Chemoembolization
1. What is Chemoembolization?
Chemoembolization is a minimally invasive procedure used primarily to treat liver cancer and other localized tumors. It involves delivering high-dose chemotherapy directly to the tumor via blood vessels while simultaneously blocking its blood supply, which starves the tumor and increases the effectiveness of the treatment.
2. How does Chemoembolization work?
The procedure combines two mechanisms:
-
Targeted Chemotherapy: A catheter is inserted through a blood vessel to deliver chemotherapy directly into the tumor, increasing local drug concentration.
-
Embolization: Tiny particles or embolic agents block the arteries feeding the tumor, cutting off oxygen and nutrients, which enhances tumor shrinkage.
This dual approach helps maximize tumor damage while minimizing systemic side effects.
3. Who is a candidate for Chemoembolization?
Chemoembolization is often recommended for patients with:
-
Primary liver cancer (hepatocellular carcinoma) that cannot be removed surgically
-
Metastatic liver tumors from other cancers
-
Adequate liver function and overall health to tolerate the procedure
-
Patients who are not suitable for surgery or other systemic treatments
A detailed evaluation by an interventional radiologist or oncologist is essential to determine candidacy.
4. How is Chemoembolization performed?
The procedure is minimally invasive and generally involves:
-
Anesthesia: Local anesthesia with sedation.
-
Catheter Insertion: A small catheter is inserted into the femoral artery in the groin and guided to the tumor-supplying arteries under imaging guidance.
-
Drug Delivery: Chemotherapy drugs mixed with embolic particles are injected directly into the tumor.
-
Embolization: Particles block the tumor's blood supply.
-
Completion: Catheter is removed, and pressure is applied to prevent bleeding.
The procedure usually takes 1-2 hours, and patients often stay in the hospital overnight for observation.
5. What are the benefits of Chemoembolization?
Chemoembolization offers several advantages:
-
Targeted treatment with high drug concentration in the tumor
-
Minimal systemic side effects compared to intravenous chemotherapy
-
Tumor shrinkage and slowed progression
-
Potential to improve survival rates for unresectable liver cancer
-
Can be combined with other therapies like radiofrequency ablation or systemic therapy
6. What are the risks and complications?
While generally safe, possible risks include:
-
Post-embolization syndrome: Fever, nausea, abdominal pain, and fatigue (temporary)
-
Liver function changes: Usually mild and reversible
-
Infection or bleeding at the catheter insertion site
-
Rarely, damage to non-target tissues or arteries
-
Allergic reaction to contrast dye used in imaging
Most side effects are manageable with proper medical care.
7. What is the recovery like after Chemoembolization?
Recovery is generally straightforward:
-
Hospital stay: Often overnight for monitoring
-
Post-procedure symptoms: Mild pain, fever, or fatigue for a few days
-
Activity: Most patients can resume light activities within 1-2 days
-
Follow-up imaging: Needed to assess tumor response and plan further treatment
Pain medication and supportive care are provided as needed.
8. How effective is Chemoembolization?
Effectiveness depends on:
-
Tumor size, location, and vascular supply
-
Liver function and overall patient health
-
Response can include tumor shrinkage, slowed growth, or symptom relief
Chemoembolization is particularly effective in unresectable hepatocellular carcinoma, with studies showing improved survival and quality of life compared to supportive care alone.
9. Can Chemoembolization be repeated?
Yes, the procedure can be repeated multiple times if needed, depending on:
-
Tumor response
-
Liver function
-
Overall patient health
Repeat treatments can help control tumor growth and maintain quality of life.
10. Are there alternatives to Chemoembolization?
Alternatives include:
-
Surgical resection of the tumor (if operable)
-
Radiofrequency or microwave ablation
-
Systemic chemotherapy or targeted therapy
-
Radiation therapy, including stereotactic body radiotherapy (SBRT)
The best treatment option depends on tumor type, size, location, liver function, and overall health.


