Introduction to Cochlear Implant
A cochlear implant (CI) is a surgically implanted electronic device designed to provide a sense of sound to an individual with severe to profound sensorineural hearing loss, particularly when traditional hearing aids no longer provide sufficient benefit. Rather than simply amplifying sound like a conventional hearing aid, a cochlear implant bypasses damaged hair cells in the inner ear (cochlea) and directly stimulates the auditory nerve.
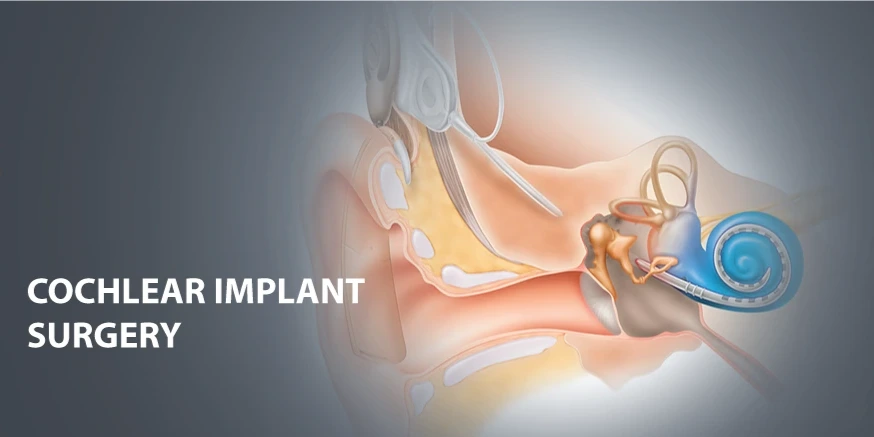
The implant typically consists of two main parts: an external sound processor (microphone, speech processor, transmitter) worn behind or on the ear, and an internal component (receiver/stimulator and electrode array) surgically placed beneath the skin behind the ear and inserted into the cochlea.
It is important to understand that while a cochlear implant does not restore "normal hearing", it can improve the ability to perceive sound and understand speech in many individuals who would otherwise have extremely limited hearing.
In recent years, eligibility criteria have expanded and outcomes have improved, making cochlear implants an increasingly important option for both children and adults. The remainder of this article will explore causes/risk factors, symptoms/signs, diagnosis, treatment options (including candidacy, surgery, rehabilitation), prevention/management of hearing loss and implant longevity, complications, and living with a cochlear implant over the long term.
Causes and Risk Factors of Hearing Loss Leading to Cochlear Implant
This section explores why people may require a cochlear implant-in other words, the underlying causes of profound hearing loss-and what factors increase those risks.
Common Causes of Severe Sensorineural Hearing Loss
-
Genetic causes: Many cases of profound hearing loss are due to inherited mutations affecting hair cells in the inner ear or auditory nerve pathways.
-
Congenital factors: Hearing loss present at birth may result from prenatal infections (e.g., cytomegalovirus, rubella), low birth weight, prematurity, or neonatal complications.
-
Progressive hearing loss: In some individuals, hearing gradually worsens over time due to degenerative changes in the cochlea or auditory nerve.
-
Acquired causes: Exposure to loud noise, ototoxic medications (e.g., certain antibiotics or chemotherapy agents), inner-ear trauma, viral infections (e.g., meningitis), or sudden sensorineural hearing loss can result in severe/immediate hearing loss.
-
Inner ear malformations: Structural anomalies of the cochlea or auditory nerve may lead to limited hearing and make hearing aids ineffective.
Risk Factors Associated with Cochlear Implant Candidacy
-
Lack of benefit from conventional hearing aids despite optimal use.
-
Age: Children identified early with profound hearing loss may benefit more from early implantation.
-
Delay in auditory stimulation: If hearing loss is longstanding without auditory input, the brain's auditory pathways may have reduced potential for rehabilitation.
-
Comorbidities: Medical conditions that affect general health or the inner ear/nerve (e.g., vestibular disorders, neurodegenerative disease) may impact prognosis.
-
Residual hearing: Individuals with some residual hearing may have different candidacy criteria and may benefit from hybrid or combined acoustic+electric stimulation.
Understanding these causes and risk factors helps in early identification of potential implant candidates, timely referral to audiology and ENT specialists, and setting expectations prior to implantation.
Symptoms and Signs Indicating Need for Cochlear Implant
This section discusses how hearing loss presents, when traditional hearing aids become insufficient, and what signs suggest a cochlear implant may be required.
Symptoms of Severe Hearing Loss
-
Inability to follow conversation, often even in quiet settings, despite using hearing aids.
-
Frequently asking for repetition, mishearing words, or inability to identify speech sounds.
-
Increasing isolation from social interactions due to difficulty in hearing.
-
In children: delayed speech and language development, lack of response to auditory stimuli, difficulty learning in noisy classroom environments.
-
In adults: sudden or rapid decline in hearing, diminishing ability to understand speech with hearing aids, or gradually worsening hearing despite amplification.
Signs Observed by Specialists
-
Pure-tone audiometry showing severe to profound sensorineural hearing loss (typically thresholds >70-90 dB HL) and poor speech discrimination scores despite hearing aid amplification.
-
Hearing aid benefit tests indicating minimal or no functional improvement with properly fitted aids.
-
Imaging (e.g., MRI/CT) showing cochlear/nerve abnormalities or confirming cochlear nerve integrity.
-
In children: delayed milestones for speech/language or non-response to auditory stimulation, visual cues, or lip-reading.
When these symptoms and signs are present, and hearing aids no longer provide adequate speech understanding, referral for cochlear implant evaluation is appropriate.
Diagnosis and Pre-Implant Evaluation
In this section we cover how specialists assess candidacy for a cochlear implant, the diagnostic work-up, and the decisions made prior to surgery.
Initial Audiologic and Medical Evaluation
-
Comprehensive audiometry (pure tone, speech discrimination) to quantify hearing loss and measure hearing aid benefit.
-
Hearing aid trials under optimal settings to determine if hearing aids suffice.
-
Medical evaluation by ENT surgeon to assess ear anatomy, cochlear/nerve status, and to rule out contraindications (such as active middle ear disease, ossified cochlea).
-
Imaging studies (CT or MRI) of the temporal bone/cochlea to assess structural anatomy, cochlear nerve presence, and evaluate for malformations.
-
General health evaluation: anesthesia fitness, comorbidities, ability to attend rehabilitation, family support (especially for children).
Candidacy and Timing Decisions
-
Eligibility criteria vary by region and manufacturer, but generally include severe-to-profound bilateral sensorineural hearing loss, limited benefit from hearing aids, and realistic expectations for rehabilitation.
-
Age considerations: Many centres now implant children as young as 9-12 months of age because early input yields better language outcomes.
-
Discussion of expected outcomes, risks, and commitment to post-implant rehabilitation is crucial.
-
Pre-implant counselling: families/patients must understand that hearing with a cochlear implant is different, requires training, and may not restore normal hearing.
Pre-operative Preparation
-
Vaccination coverage (e.g., against meningitis) may be reviewed, especially if inner ear surgery is planned.
-
Hearing preservation strategies may be discussed for those with residual hearing.
-
Logistics of device choice, implant side (unilateral vs bilateral), rehabilitation scheduling.
Through this structured diagnostic and pre-implant evaluation process, the implant team ensures that the patient is an appropriate candidate and that all factors (surgical, audiologic, rehabilitative) are in place for optimal outcome.
Treatment Options of Cochlear Implant
This key section describes the surgical procedure, device activation and post-operative rehabilitation, including variations (unilateral vs bilateral), and ongoing programming/therapy.
Surgical Procedure
-
Under general anesthesia, the surgeon makes a small incision behind the ear and drills a small opening in the mastoid bone. The internal receiver/stimulator is placed under the skin behind the ear, and an electrode array is inserted into the cochlea (inner ear).
-
The external sound processor is worn after healing, usually a few weeks later. The implant surgery typically takes 1.5-3 hours and most patients are discharged after a short hospital stay.
-
After healing, the external unit is connected, the system is "activated" or first "map" is done (programming of device settings). This marks the beginning of auditory rehabilitation.
Device Options and Strategies
-
Unilateral vs Bilateral implantation: Many children and increasingly adults receive bilateral implants for improved spatial hearing and speech understanding in background noise.
-
Hybrid systems/Electric-Acoustic Stimulation (EAS): For candidates with residual low-frequency hearing, a combined hearing aid + CI may be used.
-
Device upgrades and external processor replacements occur over time as technology advances.
Post-Surgery Activation and Rehabilitation
-
Initial activation involves programming thresholds, comfort levels and testing signal response.
-
Auditory therapy: Frequent visits with audiologists and speech/language therapists to learn to interpret the new auditory input. Many patients require months to years of therapy to maximize outcomes.
-
Monitoring and mapping: Regular follow-ups to adjust settings for optimal speech perception, music listening, and background noise management.
-
Special considerations for children: Early start of speech therapy, family engagement, auditory-verbal programmes, integration into mainstream or special schooling as appropriate.
Outcomes and Expectations
-
Many users achieve significant improvements in speech understanding, recognition of environmental sounds, and improved quality of life.
-
Outcomes depend on age at implantation, duration of deafness, residual hearing, device type, and rehabilitation intensity.
-
The hearing experience with a CI is distinct from natural hearing: sound quality differs, background noise remains a challenge, and musical perception may be limited initially.
Prevention, Management and Long-Term-Care of Cochlear Implant Users
This section addresses how to prevent further hearing damage, manage existing hearing loss, maintain device performance, and support long-term care of CI users.
Prevention and Early Intervention
-
Early identification of hearing loss via newborn screening allows earlier hearing aid trial and timely decision for cochlear implant if needed.
-
Protecting residual hearing: Avoiding loud noise exposure, ototoxic drugs, and managing middle ear conditions helps preserve any hearing the individual has.
-
For children: Early auditory-verbal therapy and family involvement support language development from the moment of device activation.
-
Routine audiologic monitoring ensures hearing loss progression is tracked and intervention is timely when hearing aids become inadequate.
Device and User Management
-
Regular maintenance of external processor (battery replacement, cleaning, updates).
-
Access to programming / mapping sessions ensures optimal device performance.
-
Monitoring for device malfunction, electrode failures or changes in auditory performance.
-
For bilateral users: Fine-tuning of both sides for binaural hearing benefits (localization, noise reduction).
-
Educational support: School accommodations, hearing assistive technology (FM/DM systems), training in listening strategies.
-
For adults: Career accommodations, communication strategies, and support in noisy environments.
Long-Term Care Considerations
-
Lifelong follow-up is required: hearing thresholds, speech outcomes, device performance, and quality of life.
-
Upgrades in technology: External processors are periodically improved, and internal parts may need replacement after many years.
-
Consideration of second implantation in the other ear if only one side was done initially and criteria met.
-
Management of expectations: Ongoing counselling about realistic outcomes (e.g., improved speech but possibly residual difficulties in noise or music).
-
In low-resource settings (e.g., India): Supporting families in access to follow-up care, device maintenance, and therapy is vital for long-term success.
Complications and Risks of Cochlear Implantation
This section highlights the potential complications of surgery, device use, and long-term risks for cochlear implant users.
Surgical and Immediate Post-operative Risks
-
Risks of anesthesia (general) and surgical complications such as infection, bleeding, wound healing issues.
-
Possible damage to facial nerve or inner ear structures (though rare with experienced surgeons).
-
Dizziness, tinnitus, or temporary balance disturbance in the early post-operative period.
-
Unintended change in residual hearing if present.
Device-Related and Long-Term Risks
-
Device failure or instability of electrode array requiring revision surgery.
-
Gradual decline in device performance or difficulty in speech intelligibility over time.
-
Risk of meningitis: Because the cochlea is opened during surgery, there may be a slightly increased risk of inner-ear infections; prophylactic vaccination and prompt care of infections are recommended.
-
Limited benefit: Some individuals may derive less hearing/speech improvement than expected due to auditory nerve damage, long duration of deafness, or other neurocognitive factors.
-
Psychological or social challenges: Adjusting to the new hearing experience, managing unrealistic expectations, communication frustrations in difficult listening environments.
How to Mitigate Risks
-
Careful candidate selection and pre-operative assessment.
-
Meticulous surgical technique and use of experienced implant centres.
-
Post-operative follow-up, device maintenance, and rehabilitation are crucial.
-
Ongoing audiologic monitoring and timely intervention if performance declines.
Living with a Cochlear Implant: Long-Term Outlook and Quality of Life
This section addresses what life is like for CI users-both children and adults-and how to optimize outcomes and lifestyle.
Children with Implants
-
Early implantation (ideally before or around age one in eligible children) is associated with better speech, language, and social outcomes.
-
With intensive therapy and hearing support, many children with cochlear implants attend mainstream schools, develop spoken language, and integrate socially.
-
Family involvement, consistent therapy, and educational support are key to success.
Adults with Implants
-
Many adults who have lost hearing later in life benefit and regain speech understanding, improved quality of life, and social interaction.
-
Success depends on duration of deafness, cognitive function, and motivation to engage in rehabilitation.
-
Adults may wear processor devices, engage with hearing assistive technology, and adjust to new listening strategies (especially in noisy environments).
Daily Life Considerations
-
Hearing performance: While many users understand speech and environmental sounds, noisy or reverberant settings remain challenging; continuous strategies (e.g., directional microphones, assistive devices) help.
-
Device maintenance: Wearing external components, managing batteries, keeping spare parts, and protecting from moisture or trauma.
-
Social and emotional: For children and families, developing communication strategies, managing expectations, and integrating into hearing or hearing-impaired communities.
-
Upgrades and technology: External processors evolve rapidly; users may benefit from periodic upgrades, firmware updates or new features (Bluetooth connectivity, streaming).
-
Access in low-resource contexts: Ensuring follow-up, device repairs, and therapy access are critical for long-term success.
Long-Term Prognosis
-
Overall outcomes are positive: many CI users report improved hearing, speech, participation in education/employment, and life satisfaction.
-
Lifelong care: Success requires ongoing audiologic and device care, monitoring for device performance, and auditory therapy when needed.
-
Realistic mindset: While implants provide a hearing benefit, they do not replicate normal hearing perfectly-users and families should understand this and plan accordingly.
Top 10 Frequently Asked Questions about Cochlear Implants
1. What is a Cochlear Implant?
A cochlear implant is a medical device that provides a sense of sound to individuals with severe to profound sensorineural hearing loss. Unlike hearing aids, which amplify sound, cochlear implants bypass damaged portions of the inner ear (cochlea) and directly stimulate the auditory nerve, enabling the brain to perceive sound.
2. Who is a candidate for a Cochlear Implant?
Candidates typically include:
-
Individuals with severe to profound hearing loss in one or both ears
-
Those who receive limited benefit from conventional hearing aids
-
Patients of any age, including children as young as 12 months
-
Individuals with healthy auditory nerves and no medical contraindications to surgery
A thorough evaluation by an audiologist and ENT surgeon is required to determine eligibility.
3. How does a Cochlear Implant work?
A cochlear implant consists of:
-
External Processor: Worn behind the ear; captures and processes sound
-
Internal Implant: Surgically placed under the skin; includes a receiver and electrode array inserted into the cochlea
-
Auditory Nerve Stimulation: Electrodes directly stimulate the auditory nerve, sending signals to the brain
-
Sound Perception: The brain interprets these signals as sound, enabling speech understanding and environmental awareness
4. How is Cochlear Implant Surgery performed?
The procedure involves:
-
Anesthesia: General anesthesia is used
-
Incision and Implant Placement: Surgeon makes a small incision behind the ear to place the internal implant and insert electrodes into the cochlea
-
Closure: Incision is sutured; surgical site heals in a few weeks
Surgery usually takes 2-3 hours, and most patients go home the same day or the next day.
5. What are the risks and complications of Cochlear Implant surgery?
Cochlear implantation is generally safe, but potential risks include:
-
Infection at the surgical site
-
Bleeding or swelling
-
Temporary dizziness or taste changes
-
Nerve injury (rare) affecting facial muscles
-
Device failure or need for replacement
-
Meningitis (rare; vaccination recommended before surgery)
6. What is the recovery process like?
Post-operative recovery includes:
-
Initial healing: Mild discomfort, swelling, or bruising for 1-2 weeks
-
Activation of the implant: Typically 3-6 weeks after surgery, once the incision is fully healed
-
Auditory training and mapping: Audiologists adjust the device and provide therapy for sound interpretation
-
Gradual improvement: Most recipients notice significant improvement in hearing over several months
7. How effective are Cochlear Implants?
Effectiveness varies, but studies show:
-
Significant improvement in speech perception and communication
-
Enhanced environmental awareness and safety
-
Children implanted early often develop near-normal speech and language skills
-
Adults benefit from improved conversation ability, even in noisy environments
8. Can both ears be implanted?
Yes, bilateral cochlear implantation is possible and may provide:
-
Improved sound localization
-
Better understanding of speech in noisy environments
-
Enhanced overall auditory experience
Your ENT surgeon can advise whether simultaneous or sequential implantation is appropriate.
9. Are there alternatives to Cochlear Implants?
Alternatives include:
-
Hearing aids for mild to severe hearing loss
-
Bone-anchored hearing systems (for conductive hearing loss)
-
Assistive listening devices and speech therapy
Cochlear implants are typically recommended when hearing aids provide limited benefit.
10. How should I prepare for Cochlear Implant surgery?
Preparation involves:
-
Comprehensive evaluation: Audiological tests, imaging, and ENT consultation
-
Vaccinations: Meningitis vaccination may be required
-
Medication review: Certain medications may need adjustment
-
Post-operative planning: Arrange support during initial recovery and rehabilitation
-
Expectations: Understanding that auditory rehabilitation is necessary for optimal outcomes


