Introduction to Colonic and Gastric Polypectomy
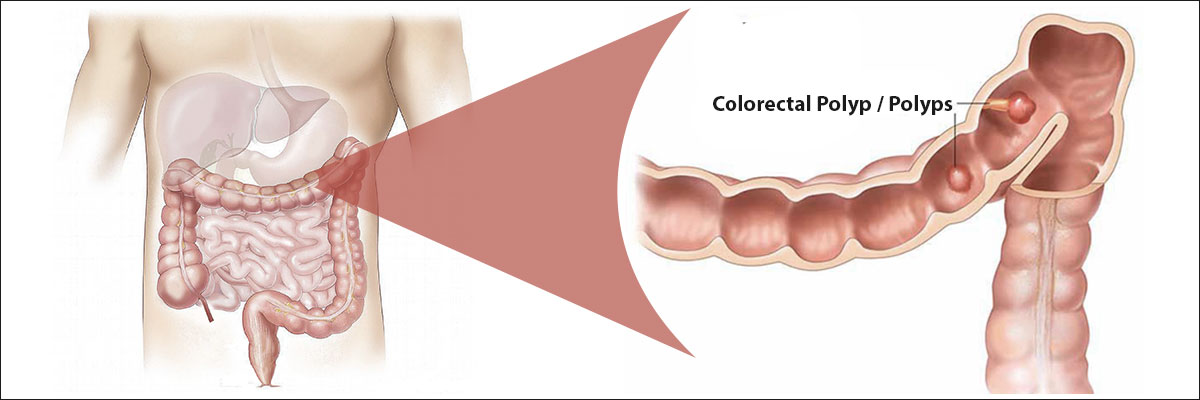
Colonic and gastric polypectomy refers to the medical procedure used to remove abnormal tissue growths called polyps from the lining of the colon (large intestine) or the stomach (gastric mucosa). Polyps are tissue overgrowths that protrude into the hollow of the digestive tract. Although many are benign (non-cancerous), certain types-particularly adenomatous or dysplastic polyps-can develop into cancer over time.
Polypectomy plays a dual role: it is both a diagnostic and preventive procedure. It allows doctors to analyze the removed tissue to determine whether it is cancerous or precancerous, and at the same time, it eliminates the risk of malignant transformation by physically removing the abnormal tissue.
Modern medicine has transformed polypectomy into a minimally invasive procedure, often performed through endoscopy. For colon polyps, this is done via colonoscopy; for stomach polyps, via gastroscopy (upper endoscopy). Both use flexible, camera-equipped tubes inserted into the digestive tract to locate and remove the growths safely, without large surgical incisions.
Polypectomy is one of the most common procedures performed in gastroenterology clinics worldwide. Its importance cannot be overstated - early removal of precancerous polyps has significantly reduced the incidence and mortality rate of colorectal cancer globally.
Causes and Risk Factors of Colonic and Gastric Polyps
Causes
Polyps in the colon and stomach form due to abnormal growth of the mucosal cells that line these organs. This abnormal growth may be triggered by genetic mutations, chronic inflammation, or environmental influences.
-
Genetic predisposition: Conditions such as Familial Adenomatous Polyposis (FAP), Peutz-Jeghers Syndrome, or Lynch Syndrome can lead to multiple polyps throughout the digestive tract.
-
Chronic irritation: Continuous inflammation of the stomach or colon mucosa - due to infection (Helicobacter pylori in the stomach) or inflammatory bowel diseases (like ulcerative colitis) - promotes abnormal cell regeneration.
-
Dietary habits: Diets low in fiber but high in processed foods, red meat, and saturated fats are linked with higher rates of colon polyps.
-
Medication effects: Long-term use of acid-suppressing drugs (PPIs) can lead to the development of gastric fundic gland polyps.
-
Aging: The risk of polyp formation increases with age as cellular renewal becomes less regulated.
Risk Factors
While anyone can develop gastrointestinal polyps, certain groups are at higher risk:
-
Age over 50 - especially for colonic polyps.
-
Family history of gastrointestinal cancers or polyposis syndromes.
-
Smoking and alcohol consumption, which accelerate mucosal damage.
-
Obesity and sedentary lifestyle, both associated with higher polyp rates.
-
Previous history of polyps: Once polyps have been removed, new ones may develop, requiring ongoing surveillance.
-
Chronic gastritis or acid reflux: Increase risk for gastric polyps.
Understanding these risk factors enables early screening and intervention, preventing future complications.
Symptoms and Signs of Colonic and Gastric Polyps
In many cases, polyps produce no noticeable symptoms and are discovered incidentally during routine screening, such as colonoscopy or endoscopy. However, when they grow large or become ulcerated, symptoms may appear.
Common Symptoms
Colonic Polyps
-
Rectal bleeding: Bright red or dark stools may indicate bleeding from a colon polyp.
-
Changes in bowel habits: Persistent constipation, diarrhea, or narrowing of stool shape.
-
Abdominal discomfort: Cramping, bloating, or mild pain in the lower abdomen.
-
Mucus in stools: Polyps may secrete mucus, which can appear in the feces.
-
Anemia: Chronic bleeding from polyps can lead to low hemoglobin and fatigue.
Gastric Polyps
-
Abdominal pain or discomfort: Especially in the upper abdomen (epigastric region).
-
Nausea and vomiting: If a polyp interferes with digestion or causes irritation.
-
Gastrointestinal bleeding: May present as black, tarry stools (melena) or vomiting blood.
-
Indigestion or early fullness: Larger gastric polyps may obstruct food passage.
Symptoms vary based on polyp location, size, and type. Importantly, even asymptomatic patients should undergo screening, as early removal is the best defense against cancer.
Diagnosis of Colonic and Gastric Polyps
Diagnosing polyps requires visual examination and histopathologic confirmation. Since small polyps are often symptomless, early detection relies on proactive screening and diagnostic testing.
Diagnostic Procedures
-
Endoscopy:
-
Colonoscopy for colon polyps and gastroscopy for stomach polyps.
-
A flexible tube with a camera visualizes the mucosa and allows real-time assessment.
-
Polyps can be identified, photographed, measured, and removed during the same session.
-
-
Imaging Studies:
-
CT colonography (virtual colonoscopy) may be used if traditional colonoscopy isn't possible.
-
Upper GI series with contrast can reveal larger gastric polyps, though less sensitive than endoscopy.
-
-
Biopsy and Histopathology:
-
Every removed polyp is sent for laboratory analysis to determine its type (hyperplastic, adenomatous, inflammatory, etc.) and malignancy potential.
-
-
Blood Tests:
-
Used to check for anemia (due to bleeding polyps) and sometimes tumor markers if malignancy is suspected.
-
Screening Recommendations
-
Colonic Polyps: Begin colonoscopy screening at age 45 (or earlier if family history exists).
-
Gastric Polyps: Individuals with chronic gastritis, H. pylori infection, or previous gastric surgery should undergo periodic endoscopic evaluation.
Early and accurate diagnosis ensures timely intervention and reduces the likelihood of cancer development.
Treatment Options: Colonic and Gastric Polypectomy
A polypectomy is the removal of a polyp using specialized endoscopic tools. It is usually performed during a colonoscopy or gastroscopy and takes 20-60 minutes depending on the number and size of polyps.
The main goal is complete removal with minimal risk to surrounding tissue, followed by pathological examination.
Techniques Used
-
Cold Snare Polypectomy:
-
Used for small polyps (<10 mm).
-
A wire loop “snare” is used to cut off the polyp without electrocautery.
-
-
Hot Snare Polypectomy:
-
Electrocautery is used to remove polyps 10-20 mm in size while sealing blood vessels to prevent bleeding.
-
-
Endoscopic Mucosal Resection (EMR):
-
Used for large or flat (sessile) polyps.
-
The polyp and surrounding mucosa are lifted by injecting fluid beneath them and then removed in one or more pieces.
-
-
Endoscopic Submucosal Dissection (ESD):
-
Advanced technique for very large or early cancerous lesions.
-
Allows precise removal of tissue en bloc (in one piece) for full pathological assessment.
-
-
Surgical Polypectomy:
-
Reserved for very large, inaccessible, or suspicious polyps not removable by endoscopy.
-
May involve laparoscopic or open surgery.
-
Aftercare
-
Patients are monitored for a few hours for bleeding or discomfort.
-
Most resume normal activities within 24-48 hours.
-
The doctor provides dietary and medication instructions to aid healing.
Polypectomy is a cornerstone of gastrointestinal cancer prevention, with minimal risk and high success rates.
Prevention and Management of Colonic and Gastric Polyps
Preventive Strategies
-
Healthy Diet:
-
Eat high-fiber foods (fruits, vegetables, whole grains).
-
Reduce intake of red meat and processed foods.
-
Avoid excessive salt and pickled foods to reduce gastric irritation.
-
-
Lifestyle Modifications:
-
Quit smoking and limit alcohol consumption.
-
Maintain healthy body weight and regular physical activity.
-
-
Medical Management:
-
Eradication of H. pylori infection lowers risk of gastric polyps.
-
Review long-term PPI (acid-suppressant) therapy with your doctor.
-
Use aspirin or NSAIDs only as prescribed, as chronic use may irritate the GI lining.
-
-
Regular Screening:
-
Colonoscopy every 5-10 years (or more frequently if prior polyps were found).
-
Upper endoscopy as advised for high-risk patients.
-
Post-Polypectomy Management
-
Monitor for post-procedure bleeding, pain, or fever.
-
Attend follow-up visits to discuss biopsy results.
-
Future surveillance intervals depend on pathology - typically 3 years for adenomatous polyps, 5 years for low-risk types.
Proactive management prevents recurrence and ensures long-term gastrointestinal health.
Complications of Colonic and Gastric Polypectomy
Polypectomy is generally safe, but as with any procedure, certain complications may occur.
Common (Minor) Complications
-
Mild bleeding: Small amounts of blood in stool are normal for 24-48 hours.
-
Abdominal discomfort or bloating: Due to air insufflation during endoscopy.
-
Temporary nausea: From sedation or anesthesia.
Serious (Rare) Complications
-
Perforation:
-
A small tear in the intestinal or gastric wall. It is rare (less than 1%) but may require surgical repair.
-
-
Post-Polypectomy Bleeding:
-
Can occur immediately or a few days after the procedure. Managed endoscopically or with medication.
-
-
Post-Polypectomy Syndrome:
-
Localized inflammation without perforation; causes pain and mild fever, treated conservatively.
-
-
Incomplete Resection:
-
If the entire polyp is not removed, residual tissue may regrow, necessitating repeat procedure.
-
-
Infection:
-
Very rare, prevented with sterile technique and antibiotics if required.
-
With modern techniques, the complication rate remains extremely low when the procedure is performed by trained specialists.
Living with the Condition: Life After Polypectomy
After undergoing colonic or gastric polypectomy, most patients recover quickly and experience significant relief knowing their cancer risk has been reduced.
Recovery and Lifestyle
-
Diet: Start with light foods (soups, soft fruits) and avoid spicy or fried dishes for a few days.
-
Activity: Normal routine can usually resume in 1-2 days, avoiding strenuous exercise for a week.
-
Medications: Avoid blood thinners (like aspirin or warfarin) unless approved by your doctor.
Emotional and Psychological Aspects
-
Knowing that polyps were removed before turning cancerous can provide peace of mind.
-
Some patients may experience anxiety about recurrence-routine follow-ups alleviate this concern.
Long-Term Outlook
-
Regular surveillance endoscopies ensure early detection of new polyps.
-
Maintaining a healthy diet and lifestyle significantly reduces recurrence risk.
-
For those with genetic syndromes, lifelong monitoring and family screening are vital.
Top 10 Frequently Asked Questions about Colonic and Gastric Polypectomy
1. What Is a Colonic and Gastric Polypectomy?
A colonic and gastric polypectomy is a medical procedure used to remove polyps from the colon (large intestine) or stomach (gastric area).
Polyps are abnormal tissue growths that form on the inner lining of these organs. Most are benign (non-cancerous), but some may develop into cancer if left untreated.
A polypectomy is typically performed during an endoscopic procedure - either a colonoscopy (for colonic polyps) or an upper endoscopy (gastroscopy) (for gastric polyps). It's a minimally invasive procedure, meaning it doesn't require open surgery and is done through a flexible scope inserted into the digestive tract.
2. Why Do Polyps Develop in the Colon or Stomach?
Polyps develop due to abnormal cell growth in the lining of the gastrointestinal (GI) tract. Several factors can increase the risk, including:
-
Age (over 50 years old)
-
Genetic predisposition (family history of polyps or colon cancer)
-
Diet high in red or processed meats
-
Smoking and alcohol consumption
-
Obesity and sedentary lifestyle
-
Chronic inflammation, such as gastritis or inflammatory bowel disease (IBD)
While most polyps are harmless, certain types - especially adenomatous or serrated polyps - have the potential to become cancerous over time.
3. How Are Colonic and Gastric Polyps Detected?
Polyps are often silent and symptomless, which is why screening tests are crucial.
They are usually detected through:
-
Colonoscopy: A camera-equipped flexible tube examines the colon and rectum.
-
Gastroscopy (Upper Endoscopy): A similar scope inspects the esophagus, stomach, and duodenum.
-
Imaging Tests: Such as CT colonography or barium X-rays (less commonly used today).
During these procedures, if a polyp is found, the doctor can often remove it immediately for biopsy and analysis.
4. What Are the Symptoms of Colonic or Gastric Polyps?
Most polyps don't cause symptoms until they grow larger or cause complications.
However, possible symptoms may include:
-
Rectal bleeding or blood in the stool
-
Unexplained anemia (low red blood cells)
-
Changes in bowel habits (diarrhea or constipation)
-
Abdominal pain or bloating
-
Unexplained weight loss
-
Nausea or vomiting (for gastric polyps)
If you experience any of these symptoms, a gastroenterologist should be consulted promptly for evaluation.
5. How Is a Polypectomy Performed?
A polypectomy is a non-surgical, endoscopic procedure performed under sedation or light anesthesia.
Procedure Steps:
-
The endoscope is gently inserted through the mouth (for gastric) or rectum (for colonic).
-
Once a polyp is located, it's removed using one of several techniques:
-
Cold Snare Polypectomy: For small polyps; uses a wire loop to cut the polyp without electrical current.
-
Hot Snare Polypectomy: For larger polyps; uses electric current to cut and cauterize tissue.
-
Endoscopic Mucosal Resection (EMR): Removes larger or flat polyps by lifting and cutting them.
-
-
The polyp is retrieved and sent to a pathology lab for microscopic examination.
The entire process usually takes 15 to 60 minutes, depending on the number and size of polyps.
6. Is Colonic or Gastric Polypectomy Painful?
No. Polypectomy is not painful because it's performed under sedation or light anesthesia.
Patients are typically asleep or deeply relaxed and feel no discomfort
during the procedure.
Afterward, mild side effects may occur, such as:
-
Bloating or gas (from air used to inflate the colon)
-
Cramping or mild soreness
-
Temporary fatigue
These usually resolve within a few hours. Most patients can go home the same day.
7. What Are the Risks or Complications of a Polypectomy?
While polypectomy is considered safe and routine, some rare risks include:
-
Bleeding (especially for larger polyps)
-
Perforation (tear) in the intestinal or stomach wall
-
Infection
-
Post-polypectomy syndrome (localized inflammation causing pain or fever)
-
Incomplete removal, requiring follow-up treatment
Your doctor will discuss your specific risks before the procedure. Serious complications occur in less than 1% of cases when performed by an experienced gastroenterologist.
8. How Should I Prepare for a Colonic or Gastric Polypectomy?
Preparation depends on whether the polyps are in the colon or stomach:
For Colonic Polypectomy:
-
You'll follow a clear liquid diet 1-2 days before the procedure.
-
A bowel preparation (laxative solution) will be prescribed to cleanse the colon.
-
Avoid iron supplements and certain blood thinners as advised.
For Gastric Polypectomy:
-
You'll need to fast for 6-8 hours before the procedure.
-
Inform your doctor about any medications, allergies, or health conditions.
Proper preparation ensures clear visualization and safe polyp removal.
9. What Is the Recovery Process After a Polypectomy?
Recovery is generally quick and uneventful:
-
You'll rest for a short time in recovery after the procedure (usually 1-2 hours).
-
Mild bloating or cramping is normal.
-
You can resume normal diet after a few hours unless otherwise instructed.
-
Avoid heavy lifting or strenuous activities for 24 hours.
If you experience severe pain, persistent bleeding, fever, or vomiting,
contact your doctor immediately.
Your doctor will discuss biopsy results and schedule a follow-up colonoscopy or
endoscopy if needed.
10. How Often Should I Get Checked for Polyps After a Polypectomy?
Follow-up frequency depends on the type, size, and number of polyps removed:
-
No or small hyperplastic polyps: Next screening in 5-10 years.
-
One or two small adenomas: Next screening in 3-5 years.
-
Multiple or large adenomas (>10mm): Follow-up in 1-3 years.
-
Cancerous or high-risk polyps: Follow-up as soon as 6-12 months.
Your gastroenterologist will customize a surveillance plan to monitor your digestive health and prevent polyp recurrence or cancer development.


