Introduction to Cone Biopsy of Cervix
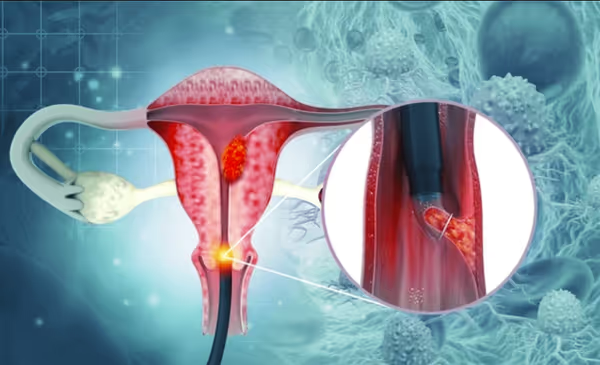
A Cone Biopsy of the Cervix, medically known as Cervical Conization, is a surgical procedure used to remove a cone-shaped section of tissue from the cervix - the lower, narrow portion of the uterus that opens into the vagina. The removed tissue includes both the outer part of the cervix (ectocervix) and part of the endocervical canal, where abnormal cells are often found. This section is sent for microscopic analysis to detect or treat precancerous conditions, carcinoma in situ, or early cervical cancer.
The cervix serves as the protective gateway between the uterus and the vagina, maintaining a sterile environment within the uterus while allowing menstrual flow out and sperm passage during conception. However, the cells of the cervix can undergo changes due to persistent infection by the Human Papillomavirus (HPV) - the most common cause of cervical abnormalities. Over time, these abnormal cells can develop into Cervical Intraepithelial Neoplasia (CIN) or even invasive cancer if left untreated.
A cone biopsy serves two main purposes:
-
Diagnostic: to determine the extent of abnormality or confirm cancer after abnormal Pap smear or biopsy results.
-
Therapeutic: to remove all abnormal tissue and prevent progression to invasive cancer.
This procedure can be performed using different techniques, such as cold knife conization (CKC), loop electrosurgical excision procedure (LEEP), or laser conization, depending on the nature of the lesion and the patient's fertility considerations.
Cone biopsy is typically done under regional or general anesthesia and can often be completed as an outpatient procedure. The recovery period is relatively short, and the results are extremely effective in preventing the development of cervical cancer. It is an essential step in modern cervical cancer prevention and management programs worldwide.
Causes and Risk Factors Necessitating Cone Biopsy of Cervix
The need for a cone biopsy arises when screening or diagnostic tests detect abnormal cervical cells that are potentially precancerous or suspicious for early cancer. These changes occur primarily because of persistent infection with high-risk HPV strains (especially HPV types 16 and 18).
A. Underlying Causes:
-
High-Grade Cervical Intraepithelial Neoplasia (CIN II/III):
These are precancerous changes confined to the top layers of cervical tissue. Cone biopsy removes this abnormal tissue before it progresses deeper. -
Microinvasive or Early-Stage Cervical Cancer:
If early cancer is suspected but not confirmed, a cone biopsy allows for diagnosis and staging. -
Unsatisfactory Colposcopy:
Sometimes, during a colposcopic exam (where the cervix is viewed under magnification), the entire transformation zone - where abnormal cells typically occur - cannot be visualized. In such cases, a cone biopsy provides a full sample. -
Glandular Abnormalities:
When Pap smear or biopsy shows atypical glandular cells or adenocarcinoma in situ, a cone biopsy ensures complete removal of suspicious tissue. -
Persistent Abnormal Pap or HPV Tests:
Repeated detection of high-risk HPV or high-grade cytology findings after other treatments may necessitate conization for a more accurate evaluation.
B. Risk Factors Leading to Cervical Abnormalities:
-
HPV Infection: The most significant risk factor.
-
Early Sexual Activity and Multiple Partners: Increases HPV exposure.
-
Smoking: Tobacco byproducts damage cervical cells and reduce immune response.
-
Weakened Immunity: Due to HIV infection, long-term steroid use, or organ transplantation.
-
Poor Genital Hygiene or Chronic Inflammation: Prolonged irritation of cervical tissue.
-
Long-term Oral Contraceptive Use: When not monitored medically.
-
Lack of Regular Screening: Skipping Pap smears delays detection of precancerous changes.
Recognizing these risk factors allows doctors and patients to prevent disease progression through vaccination, regular screening, and early treatment such as cone biopsy when necessary.
Symptoms and Signs That May Lead to Cone Biopsy
In many cases, cervical abnormalities are silent - women may feel perfectly healthy even as precancerous cells develop. This makes routine cervical screening (Pap smears and HPV tests) absolutely essential. However, some women may experience symptoms that indicate an underlying problem requiring further evaluation.
Common Symptoms Include:
-
Abnormal Vaginal Bleeding:
-
Bleeding between periods.
-
Post-coital bleeding (after intercourse).
-
Bleeding after menopause.
-
-
Unusual Vaginal Discharge:
Persistent discharge that is watery, pinkish, or foul-smelling may indicate infection or abnormal cell growth. -
Pelvic Pain or Discomfort:
Pain during sexual intercourse or persistent lower abdominal pain may occur in advanced stages. -
Abnormal Pap Smear or HPV Test Results:
Even without symptoms, repeated abnormal test results often lead to a cone biopsy for confirmation. -
Colposcopic Findings:
If colposcopy reveals abnormal patterns such as acetowhite changes, atypical vascularization, or mosaic patterns, further investigation with a cone biopsy may be warranted.
Silent Progression:
Most importantly, cervical dysplasia and early cancer often develop without any warning signs. That is why women are encouraged to undergo routine screening every 3-5 years, depending on their age and health status.
Diagnosis Leading to Cone Biopsy of Cervix
Cone biopsy is usually the result of a structured diagnostic process. It is the next step when less invasive tests have shown abnormalities that need confirmation or removal.
Step 1: Cervical Screening (Pap Smear and HPV Test)
-
The Pap test examines cervical cells under a microscope for abnormalities.
-
The HPV test checks for high-risk virus types that cause cervical cancer.
Step 2: Colposcopy
If screening tests are abnormal, colposcopy is performed to visually inspect the cervix using magnification. Special dyes (acetic acid or iodine) highlight suspicious areas.
Step 3: Biopsy or Endocervical Curettage
Small tissue samples are taken from suspicious spots. If results indicate high-grade lesions or invasion cannot be ruled out, a cone biopsy is the logical next diagnostic step.
Step 4: Pre-Procedural Evaluation
Before surgery, your doctor will review:
-
Medical history and medications (especially blood thinners).
-
Pregnancy status (procedure avoided during pregnancy unless necessary).
-
Blood tests and anesthesia planning.
Step 5: Histopathology Post-Biopsy
After the cone biopsy, the removed tissue is examined under a microscope to:
-
Confirm the exact diagnosis (CIN grade or invasive cancer).
-
Check if margins are free of abnormal cells.
-
Assess the need for additional treatment.
Accurate diagnosis through conization ensures early intervention, significantly improving survival and fertility outcomes.
Treatment Options and the Cone Biopsy Procedure
A cone biopsy (also called cervical conization) is both a diagnostic and therapeutic procedure used to remove a cone-shaped sample of tissue from the cervix. It is most often performed to evaluate and treat precancerous changes (dysplasia) or very early-stage cervical cancer, especially when less-invasive techniques are inadequate or the abnormal area is not fully seen.
A. Types of Cone Biopsy Procedures
-
Cold Knife Conization (CKC):
-
Performed under general or regional anesthesia in a hospital.
-
A scalpel is used to excise a cone-shaped portion of the cervix.
-
Provides the most accurate tissue margins for microscopic examination.
-
Preferred when cancer is suspected or when glandular abnormalities are involved.
-
-
Loop Electrosurgical Excision Procedure (LEEP/LETZ):
-
Uses a thin, electrified wire loop to remove the tissue.
-
Done under local anesthesia, usually in an outpatient setting.
-
Minimally invasive, less bleeding, and shorter recovery.
-
-
Laser Conization:
-
Uses a focused laser beam to vaporize or cut the affected tissue.
-
Provides precise control with minimal damage to surrounding areas.
-
B. Step-by-Step Process
-
The patient is placed in a lithotomy position.
-
Anesthesia is administered.
-
A speculum is inserted to visualize the cervix.
-
The abnormal area is removed in a cone-shaped segment that includes the transformation zone.
-
The tissue is immediately sent to pathology for examination.
-
Bleeding is controlled with sutures or cauterization.
C. Post-Surgery Care
-
Mild cramping or bleeding for a few days is normal.
-
Avoid intercourse, douching, and tampon use for about 4-6 weeks.
-
Pain relief medication and antibiotics may be prescribed.
-
Results are discussed in 7-10 days, and further treatment is planned if necessary.
Cone biopsy is often curative for precancerous lesions and early-stage cervical cancers, sparing women from more extensive surgeries.
Prevention and Management of Cone Biopsy Of Cervix
Cone biopsy of the cervix is a valuable procedure for diagnosing and treating cervical abnormalities, but it carries risks of complications that can be minimized by careful technique, patient preparation, and proper aftercare. Prevention centers on reducing recurrence of cervical disease and managing fertility or cervical function.
A. Preventive Strategies
-
HPV Vaccination:
Protects against the most common cancer-causing HPV types. Recommended for both males and females starting at 9-14 years of age. -
Regular Screening:
-
Women aged 21-29: Pap test every 3 years.
-
Women aged 30-65: Pap and HPV co-testing every 5 years or Pap test alone every 3 years.
-
-
Safe Sexual Practices:
Limiting partners and using protection reduces HPV transmission. -
Avoid Smoking:
Smoking doubles the risk of cervical dysplasia due to immune suppression. -
Prompt Treatment of Infections:
Timely management of vaginal or cervical infections helps prevent chronic inflammation.
B. Post-Cone Biopsy Management
-
Follow-up Testing: Pap smears and HPV testing at regular intervals to detect recurrence.
-
Lifestyle Modifications: A diet rich in fruits, vegetables, antioxidants, and vitamins A, C, and E supports cervical healing and immunity.
-
Pregnancy Monitoring: Women who wish to conceive should inform their obstetrician, as they may need cervical monitoring or cerclage.
Complications of Cone Biopsy Of Cervix
While generally safe, cone biopsy can carry some risks, particularly if large tissue sections are removed.
-
Bleeding: Most common but usually manageable.
-
Infection: Rare, can present as fever, pelvic pain, or foul discharge.
-
Cervical Stenosis: Scar tissue may narrow the cervical canal, affecting menstruation or fertility.
-
Cervical Insufficiency: Loss of cervical strength leading to miscarriage or preterm labor in later pregnancies.
-
Pain and Cramps: Mild to moderate discomfort for several days.
-
Recurrence: Rare, but possible if abnormal cells remain.
-
Emotional Distress: Anxiety about cancer or fertility may affect mental health - reassurance and support are key.
Modern techniques and skilled surgeons keep complication rates extremely low.
Living with the Condition After Cone Biopsy
Living with the condition after a cone biopsy of the cervix involves a brief initial recovery period, adherence to activity restrictions, awareness of potential complications, and some long-term considerations—especially for those concerned with fertility or pregnancy. Most patients recover fully and return to their usual activities, but individualized attention to healing and follow-up is essential.
Physical Recovery:
-
Avoid heavy lifting and strenuous exercise for 1-2 weeks.
-
Expect mild vaginal discharge and spotting for several days.
-
Use sanitary pads, not tampons.
Emotional Well-being:
It's natural to feel anxious awaiting results or about future fertility. Open communication with your healthcare team and support groups helps tremendously.
Fertility and Pregnancy:
Most women retain the ability to conceive and carry pregnancies successfully. However, doctors may monitor cervical length more closely during pregnancy to prevent premature dilation.
Long-Term Outlook:
After a successful cone biopsy with clear margins, the prognosis is excellent. The risk of recurrence is very low with proper follow-up and healthy lifestyle choices.
Top 10 Frequently Asked Questions about Cone Biopsy of the Cervix
1. What Is a Cone Biopsy of the Cervix?
A Cone Biopsy, also known as Cervical Conization, is a surgical procedure used to remove a cone-shaped section of abnormal tissue from the cervix - the lower, narrow part of the uterus that opens into the vagina.
The removed tissue includes precancerous or suspicious cells detected during abnormal Pap smears or colposcopy.
The main goals of a cone biopsy are to:
-
Diagnose cervical cancer or precancerous conditions (CIN - Cervical Intraepithelial Neoplasia).
-
Treat early-stage abnormalities by removing affected tissue before it turns cancerous.
This procedure helps both detect and prevent cervical cancer and is often done under local or general anesthesia.
2. Why Is a Cone Biopsy Needed?
Your doctor may recommend a cone biopsy if:
-
A Pap test or HPV test shows abnormal results.
-
A colposcopy reveals precancerous changes in the cervix.
-
There are signs of CIN 2 or CIN 3 (moderate to severe dysplasia).
-
Early-stage cervical cancer is suspected.
-
Other tests (e.g., punch biopsy) did not provide enough tissue for accurate diagnosis.
In many cases, a cone biopsy can serve both diagnostic and therapeutic purposes, as removing the abnormal area may cure the condition entirely.
3. How Is a Cone Biopsy Performed?
Cone biopsy is a short outpatient surgical procedure that usually takes 15 to 30 minutes. It can be done using one of several methods:
-
Cold Knife Conization (CKC): Uses a surgical scalpel to remove the tissue under general or spinal anesthesia.
-
LEEP (Loop Electrosurgical Excision Procedure): Uses a thin wire loop heated by an electrical current to remove tissue.
-
Laser Conization: Uses a focused laser beam to excise abnormal areas precisely.
During the procedure, the surgeon removes a cone-shaped section of the cervix containing the abnormal cells. The tissue is then sent to a pathology lab for microscopic examination.
4. What Happens Before and After the Procedure?
Before the Cone Biopsy:
-
You'll have a pelvic exam, Pap smear, or colposcopy for evaluation.
-
Avoid intercourse, douching, or vaginal medications 24 hours before the procedure.
-
If under anesthesia, you'll need to fast for several hours before surgery.
After the Procedure:
-
You may experience light bleeding, spotting, or mild cramping for a few days.
-
Avoid tampons, douching, and sexual activity for about 4-6 weeks to allow healing.
-
Your doctor will discuss results and follow-up appointments once the biopsy is analyzed.
5. Is a Cone Biopsy Painful?
Most women experience little or no pain during the procedure, as it's done under local, regional, or general anesthesia.
Afterward, mild cramping or pelvic discomfort may occur for a few days - similar to menstrual cramps. Over-the-counter pain relievers like ibuprofen or acetaminophen are usually sufficient to manage it.
Your doctor may recommend rest for 24-48 hours before resuming normal activities.
6. What Are the Risks or Possible Complications of a Cone Biopsy?
Cone biopsy is generally safe, but as with any surgical procedure, there are some potential risks, including:
-
Bleeding or infection at the surgical site
-
Cervical scarring (stenosis) - narrowing of the cervix
-
Weakening of the cervix (incompetent cervix), which can affect future pregnancies
-
Delayed healing or persistent discharge
-
Premature birth or miscarriage risk (very rare, especially in extensive biopsies)
Your doctor will take measures to minimize these risks and discuss them before the procedure.
7. How Long Does It Take to Recover from a Cone Biopsy?
Recovery time depends on the biopsy method used and your individual healing. Generally:
-
Light bleeding or discharge: May last up to 2-3 weeks.
-
Full healing: Takes about 4-6 weeks.
-
Work or routine activities: Most women return within 2-3 days, avoiding strenuous exercise or lifting.
Follow your doctor's post-procedure instructions carefully, and attend all follow-up appointments to ensure proper healing.
8. Will a Cone Biopsy Affect My Fertility or Future Pregnancy?
In most cases, a cone biopsy does not affect fertility or the ability to conceive.
However, if a large portion of cervical tissue is removed, it may slightly increase the risk of:
-
Preterm labor or premature birth
-
Cervical incompetence (weak cervix during pregnancy)
Your doctor may recommend extra monitoring or a cervical cerclage (a stitch to reinforce the cervix) in future pregnancies if needed.
Discuss your family planning goals with your gynecologist before the procedure to choose the most appropriate treatment method.
9. How Are the Biopsy Results Interpreted?
The biopsy sample is sent to a pathologist for detailed microscopic analysis. Results may show:
-
Normal tissue: No further treatment required.
-
Cervical intraepithelial neoplasia (CIN 1, 2, or 3): Indicates the degree of precancerous changes.
-
Carcinoma in situ: Very early, localized cancer (often treatable by the biopsy itself).
-
Invasive cancer: Further treatment or surgery may be needed.
Your doctor will review the results with you and recommend next steps, such as observation, repeat Pap tests, or additional treatment.
10. What Is the Long-Term Outlook After a Cone Biopsy?
The outlook after a cone biopsy is excellent, especially when performed early.
-
Most women recover fully and resume normal activities within a few weeks.
-
The procedure often removes all abnormal cells, preventing cervical cancer development.
-
Regular follow-up Pap tests and HPV screenings are essential to monitor recurrence.
Long-term complications are rare, and with proper care, most patients lead healthy, normal reproductive lives after the procedure.


