Introduction to Craniectomy Decompression
A Craniectomy Decompression, also known as Decompressive
Craniectomy (DC), is a critical neurosurgical procedure performed
to relieve elevated intracranial pressure (ICP) caused by brain swelling. When
the brain swells following trauma, stroke, or other neurological events, the
rigid skull restricts expansion, leading to compression of vital brain
structures.
To prevent brain herniation and potential death, part of the skull (a bone flap)
is surgically removed, allowing the swollen brain to expand safely. The bone
flap may be stored for later replacement (cranioplasty) once swelling subsides.
This surgery is often life-saving and performed in emergency or severe neurological cases such as traumatic brain injury (TBI), malignant cerebral infarction (stroke), subarachnoid hemorrhage, or refractory intracranial hypertension.
Craniectomy Decompression is part of advanced neurocritical care and has significantly improved survival rates in patients with life-threatening brain edema.
Causes and Risk Factors for Craniectomy Decompression
Decompressive Craniectomy is not performed for a disease itself but rather as a
treatment for conditions causing uncontrollable brain
swelling.
The underlying causes include:
A. Common Causes
-
Traumatic Brain Injury (TBI):
Severe head injuries resulting in brain swelling, bleeding, or hematomas are leading indications for DC. -
Ischemic Stroke (Malignant Middle Cerebral Artery Infarction):
Blockage of large brain arteries can cause massive brain swelling and infarction. -
Intracerebral Hemorrhage:
Bleeding within the brain tissue increases intracranial pressure. -
Subarachnoid Hemorrhage (SAH):
Bleeding into the space around the brain causes irritation, swelling, and vasospasm. -
Brain Tumors or Abscesses:
Space-occupying lesions can increase intracranial pressure and may require decompression. -
Infections such as Encephalitis or Meningitis:
Severe inflammation can lead to brain swelling and pressure rise.
B. Risk Factors
-
Severe head trauma (road accidents, sports injuries, falls)
-
Hypertension and vascular disorders
-
Blood clotting abnormalities
-
Previous brain surgeries or trauma
-
Age (younger patients may have more aggressive brain swelling)
-
Delay in treating the initial cause of swelling
Early identification and management of high-risk patients can help reduce the need for decompressive craniectomy.
Symptoms and Signs of Increased Intracranial Pressure
Before a craniectomy is performed, patients typically show clinical and radiological signs of raised intracranial pressure (ICP). Symptoms vary depending on the underlying cause and severity but may include:
A. Neurological Symptoms
-
Severe, persistent headache
-
Nausea and vomiting
-
Altered level of consciousness (confusion, drowsiness, or coma)
-
Seizures
-
Unequal pupils (anisocoria)
-
Weakness or paralysis on one side of the body
-
Visual disturbances or loss of vision
-
Speech difficulties or slurred speech
B. Systemic Signs
-
Cushing's Triad:
A combination of hypertension, bradycardia, and irregular respiration - a hallmark of dangerous ICP elevation. -
Vomiting without nausea
-
Posturing (abnormal flexion or extension movements)
Prompt recognition of these symptoms and rapid neuroimaging are essential to prevent irreversible brain injury.
Diagnosis of Conditions Requiring Craniectomy Decompression
The diagnosis involves clinical assessment, neurological evaluation, and imaging studies to confirm brain swelling and determine the cause.
A. Clinical Evaluation
-
Assessment of Glasgow Coma Scale (GCS) score
-
Neurological examination for pupil reactivity, limb movement, and reflexes
-
Monitoring of vital signs and ICP trends
B. Imaging Studies
-
CT Scan (Computed Tomography):
The primary tool to detect cerebral edema, midline shift, bleeding, or herniation. -
MRI (Magnetic Resonance Imaging):
Provides detailed visualization of brain tissue, infarction zones, and swelling extent. -
Cerebral Angiography:
Used when vascular occlusions, aneurysms, or strokes are suspected.
C. ICP Monitoring
-
In critical care, an intracranial pressure monitor may be inserted to measure ICP directly.
-
Persistent ICP >20-25 mmHg despite medical therapy often indicates the need for decompressive craniectomy.
Treatment Options for Craniectomy Decompression
A. Pre-Surgical (Medical) Management
Before surgery, doctors attempt to control ICP through:
-
Osmotic therapy (mannitol or hypertonic saline)
-
Controlled ventilation to manage carbon dioxide levels
-
Sedation to minimize brain activity
-
Head elevation (30°) to enhance venous drainage
-
Temperature control (preventing hyperthermia)
If these measures fail, Decompressive Craniectomy becomes the definitive treatment.
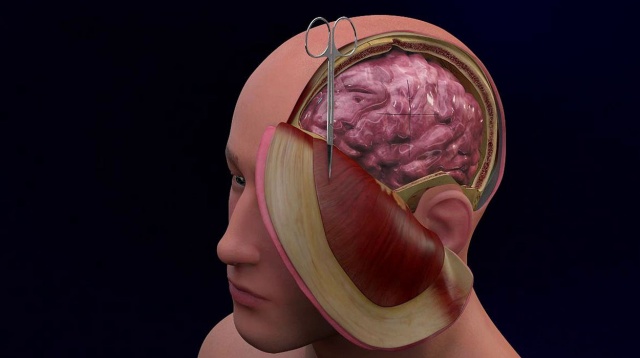
B. Surgical Procedure: Decompressive Craniectomy
-
Preparation and Anesthesia:
Performed under general anesthesia in a neurosurgical operating room. -
Surgical Steps:
-
A scalp incision is made at the affected area (often unilateral fronto-temporo-parietal region).
-
A large bone flap is removed to allow brain expansion.
-
Dura mater (outer brain membrane) is opened and sometimes expanded using a dural graft.
-
Any hematoma or blood clot is evacuated if present.
-
The bone flap is preserved (frozen or stored in the abdominal wall) for later cranioplasty.
-
The scalp is closed over the brain without replacing the bone.
-
-
Postoperative Care:
-
ICU monitoring for ICP, blood pressure, and oxygen levels.
-
Ventilator support may be needed.
-
Regular CT scans to monitor swelling reduction.
-
C. Cranioplasty (Bone Replacement)
-
Performed weeks or months later when brain swelling subsides.
-
Restores skull integrity and protection.
Prevention and Management After Craniectomy Decompression
While prevention of the underlying brain injury is ideal, management after surgery focuses on rehabilitation and neurological recovery.
A. Prevention of Initial Brain Injury
-
Use of helmets and seatbelts
-
Control of hypertension and diabetes
-
Immediate medical response to head trauma or stroke
-
Avoidance of smoking and excessive alcohol
B. Post-Surgical Management
-
Strict infection control at surgical site
-
Seizure prevention (antiepileptic drugs)
-
Nutritional and physical therapy
-
ICP and fluid balance monitoring
-
Psychological counseling and family support
C. Long-Term Management
-
Regular neurological follow-up
-
Physical and occupational therapy for mobility and coordination
-
Speech therapy if communication is affected
-
Scheduled cranioplasty to restore skull protection
Complications of Craniectomy Decompression
Although life-saving, Decompressive Craniectomy carries potential complications, including:
A. Early Complications
-
Bleeding or hematoma
-
Infection (meningitis, wound infection)
-
Brain herniation through the defect
-
Hydrocephalus (excess fluid buildup)
-
Seizures
B. Late Complications
-
Sinking Skin Flap Syndrome (Trephine Syndrome):
The scalp over the craniectomy site sinks, causing headaches or neurological decline. -
Cognitive or personality changes
-
Skull deformities if cranioplasty is delayed
-
CSF leaks or wound healing issues
Proper monitoring, infection prevention, and timely cranioplasty help minimize risks.
Living with the Condition after Craniectomy Decompression
Recovery from decompressive craniectomy can be a prolonged journey that involves multidisciplinary rehabilitation and psychosocial adaptation.
A. Rehabilitation and Recovery
-
Most patients require intensive physical therapy to regain strength and coordination.
-
Speech and occupational therapy help restore communication and daily functioning.
-
Neuropsychological support addresses memory, mood, and emotional challenges.
B. Lifestyle Adjustments
-
Wearing a protective helmet until cranioplasty is done.
-
Avoiding contact sports or activities that risk head injury.
-
Following a balanced diet and regular medical follow-ups.
-
Managing comorbidities such as hypertension, diabetes, and cholesterol.
C. Long-Term Outlook
-
Many patients regain functional independence, especially if treated early.
-
Recovery depends on the underlying cause, age, and severity of brain injury.
-
Emotional support and rehabilitation are vital for quality of life.
Top 10 Frequently Asked Questions about Craniectomy Decompression
1. What is Craniectomy Decompression?
Craniectomy decompression, also known as decompressive craniectomy, is a neurosurgical procedure in which a portion of the skull is temporarily removed to relieve pressure on the brain. It is typically performed in cases of severe brain swelling (cerebral edema) due to trauma, stroke, hemorrhage, or other conditions. The removed bone may be replaced later once the swelling subsides.
2. Why is Craniectomy Decompression performed?
This surgery is usually indicated when intracranial pressure (ICP) becomes dangerously high, threatening brain function. Key reasons include:
-
Severe traumatic brain injury with swelling
-
Large ischemic or hemorrhagic stroke
-
Intracranial hematoma causing pressure
-
Brain infections or tumors leading to mass effect
-
To prevent brain herniation, which can be life-threatening
The main goal is to protect the brain from permanent damage and improve survival.
3. Who is a candidate for Craniectomy Decompression?
Candidates generally include patients with:
-
Evidence of high intracranial pressure unresponsive to medical therapy
-
Significant neurological deterioration
-
Severe brain swelling or hematoma visible on imaging
-
Patients who are medically stable enough to undergo surgery
Decisions are based on CT/MRI scans, neurological assessment, and overall patient condition.
4. How is Craniectomy Decompression performed?
The procedure involves:
-
Anesthesia: General anesthesia ensures the patient is unconscious and pain-free
-
Incision: A section of the scalp is opened to expose the skull
-
Bone Removal: A portion of the skull is removed, creating space for the swollen brain
-
Dural Opening: The dura (brain covering) may be opened to further relieve pressure
-
Closure: Scalp is closed over the removed section; a protective helmet may be worn until bone replacement
The procedure duration depends on extent of swelling and complexity.
5. What are the risks and complications?
Craniectomy decompression is life-saving but carries risks:
-
Infection at the surgical site
-
Bleeding or hematoma formation
-
Seizures post-surgery
-
Brain injury or neurological deficits
-
CSF leakage (cerebrospinal fluid)
-
Bone flap complications such as resorption or delayed replacement
These risks are weighed against the potential life-saving benefits.
6. What is the recovery process like?
Recovery depends on the underlying cause and extent of brain injury:
-
ICU stay: Close monitoring of neurological function and intracranial pressure
-
Physical therapy: To regain motor skills, speech, and cognitive function
-
Rehabilitation: Occupational and speech therapy as needed
-
Bone flap replacement (cranioplasty): Performed weeks or months later once swelling decreases
Recovery can take weeks to months, and outcomes depend on severity of initial injury.
7. Will the removed bone be replaced?
Yes, the removed bone is usually stored and reattached later in a procedure called cranioplasty. In some cases, artificial materials such as titanium or PEEK implants are used if the original bone cannot be reused. Bone replacement restores normal skull contour and protection.
8. How does Craniectomy Decompression affect long-term brain function?
-
Outcomes vary depending on underlying brain injury and timeliness of intervention
-
Early decompression can reduce permanent brain damage and improve survival
-
Patients may still experience neurological deficits, including cognitive, speech, or motor impairments
-
Long-term rehabilitation can maximize functional recovery
9. Are there alternatives to Craniectomy Decompression?
For elevated intracranial pressure, alternatives include:
-
Medical management: Osmotic agents, hypertonic saline, and sedation
-
Controlled hypothermia to reduce brain swelling
-
Minimally invasive procedures: Such as ventriculostomy to drain cerebrospinal fluid
Craniectomy is typically reserved for severe, life-threatening swelling not responsive to medical therapy.
10. How should I prepare for Craniectomy Decompression?
Preparation is usually urgent due to the life-threatening nature of the condition:
-
Rapid medical assessment including imaging and neurological evaluation
-
Stabilization of blood pressure, oxygenation, and other vital parameters
-
Consent from family or guardians in emergency situations
-
Post-operative planning for ICU care, rehabilitation, and future cranioplasty
Early recognition and intervention are critical to prevent irreversible brain damage.


