Introduction to raniectomy of Aneurysms / AXM
Craniectomy of Aneurysms, also known as AXM, is a specialized neurosurgical procedure performed to treat life-threatening complications that arise due to a ruptured or complex brain aneurysm. An aneurysm is a weak or bulging area in the wall of a brain artery that can enlarge over time and eventually rupture, leading to subarachnoid hemorrhage (SAH) - a severe form of stroke. When bleeding occurs inside the brain, it often results in increased intracranial pressure (ICP) and brain swelling, which can quickly become fatal if not treated.
A craniectomy involves removing a section of the skull bone (called a bone flap) to allow the swollen brain to expand safely without being compressed against the skull. This helps to relieve dangerous pressure and prevents further brain injury. The removed bone flap may be replaced later once the swelling subsides, a procedure known as cranioplasty.
This surgical approach is typically used in patients with massive bleeding, large aneurysms, or refractory brain swelling after aneurysm rupture. The goal of this procedure is to save life, preserve brain function, and stabilize intracranial dynamics.
Causes and Risk Factors of Craniectomy of Aneurysms / AXM
The root cause leading to craniectomy is the formation and rupture of a cerebral aneurysm. A brain aneurysm develops when the arterial wall weakens due to genetic, structural, or lifestyle factors. Over time, blood pressure causes this weakened segment to balloon outward, forming a sac-like structure.
Primary Causes:
-
Congenital vessel wall defects - Some individuals are born with weaker blood vessel walls, making them more susceptible to aneurysm formation.
-
Chronic hypertension - High blood pressure increases stress on the arterial walls, accelerating aneurysm growth and rupture risk.
-
Atherosclerosis - Fatty deposits in arteries can lead to wall weakening.
-
Connective tissue disorders - Conditions such as Ehlers-Danlos syndrome or polycystic kidney disease are associated with aneurysms.
-
Infections or trauma - Rarely, infections (mycotic aneurysms) or head injuries can cause arterial damage leading to aneurysm formation.
Risk Factors for Rupture:
-
Persistent high blood pressure
-
Cigarette smoking or excessive alcohol consumption
-
Family history of brain aneurysm or subarachnoid hemorrhage
-
Age and gender - Middle-aged and elderly individuals, particularly women, are more prone
-
Large or irregular aneurysms located in critical arterial junctions
When an aneurysm ruptures, the subsequent brain bleeding and swelling can become uncontrollable, necessitating an emergency craniectomy to relieve intracranial pressure and save the patient's life.
Symptoms and Signs of Craniectomy of Aneurysms / AXM
The symptoms are primarily related to the underlying aneurysm and the increase in intracranial pressure following rupture. Recognizing these early can be lifesaving.
Before Rupture:
-
Persistent or localized headache
-
Visual disturbances such as double vision or blurred vision
-
Drooping eyelid or facial weakness
-
Pain above or behind the eye
-
Difficulty concentrating or dizziness
After Rupture:
-
A sudden, severe headache often described as “the worst headache of my life”
-
Loss of consciousness or fainting spells
-
Nausea and vomiting due to increased pressure inside the skull
-
Neck stiffness and light sensitivity
-
Seizures or convulsions
-
Weakness or numbness in limbs
-
Pupil dilation or unequal pupils
When Craniectomy Becomes Necessary:
As bleeding progresses, swelling and intracranial hypertension can cause:
-
Decreased level of consciousness or coma
-
Worsening headache unresponsive to medication
-
Abnormal breathing patterns
-
Seizures unresponsive to drugs
-
Brain herniation signs such as unequal pupils or decerebrate posturing
At this stage, emergency craniectomy is performed to prevent further brain damage and death.
Diagnosis of Craniectomy of Aneurysms / AXM
Accurate and rapid diagnosis is crucial for successful treatment. Modern neuroimaging and clinical assessments allow doctors to evaluate both the aneurysm and the need for decompressive surgery.
Initial Evaluation:
-
Neurological examination: To assess consciousness, reflexes, and motor responses.
-
Non-contrast CT scan: The first and most vital test; it detects bleeding, hematoma, and swelling.
-
CT Angiography (CTA): Helps visualize the aneurysm's size, shape, and exact location.
-
Magnetic Resonance Imaging (MRI): Provides detailed brain structure and tissue damage visualization.
-
Digital Subtraction Angiography (DSA): Considered the gold standard for aneurysm diagnosis and surgical planning.
Monitoring Intracranial Pressure:
If swelling is suspected, intracranial pressure monitoring helps determine whether surgical decompression is necessary.
Pre-Surgical Planning:
Based on imaging and patient status, neurosurgeons evaluate whether the aneurysm should be treated with clipping (open surgery), endovascular coiling (minimally invasive), or craniectomy in case of life-threatening swelling. The multidisciplinary team (neurosurgeon, neurologist, anesthesiologist, critical care expert) decides the safest and most effective route.
Treatment Options for Craniectomy of Aneurysms / AXM
The treatment involves two aspects: managing the aneurysm and controlling intracranial pressure through surgical means.
1. Aneurysm Repair
-
Endovascular Coiling: A catheter is inserted through the groin or wrist and advanced into the brain arteries. Platinum coils are placed inside the aneurysm to block blood flow, preventing rupture or re-bleeding.
-
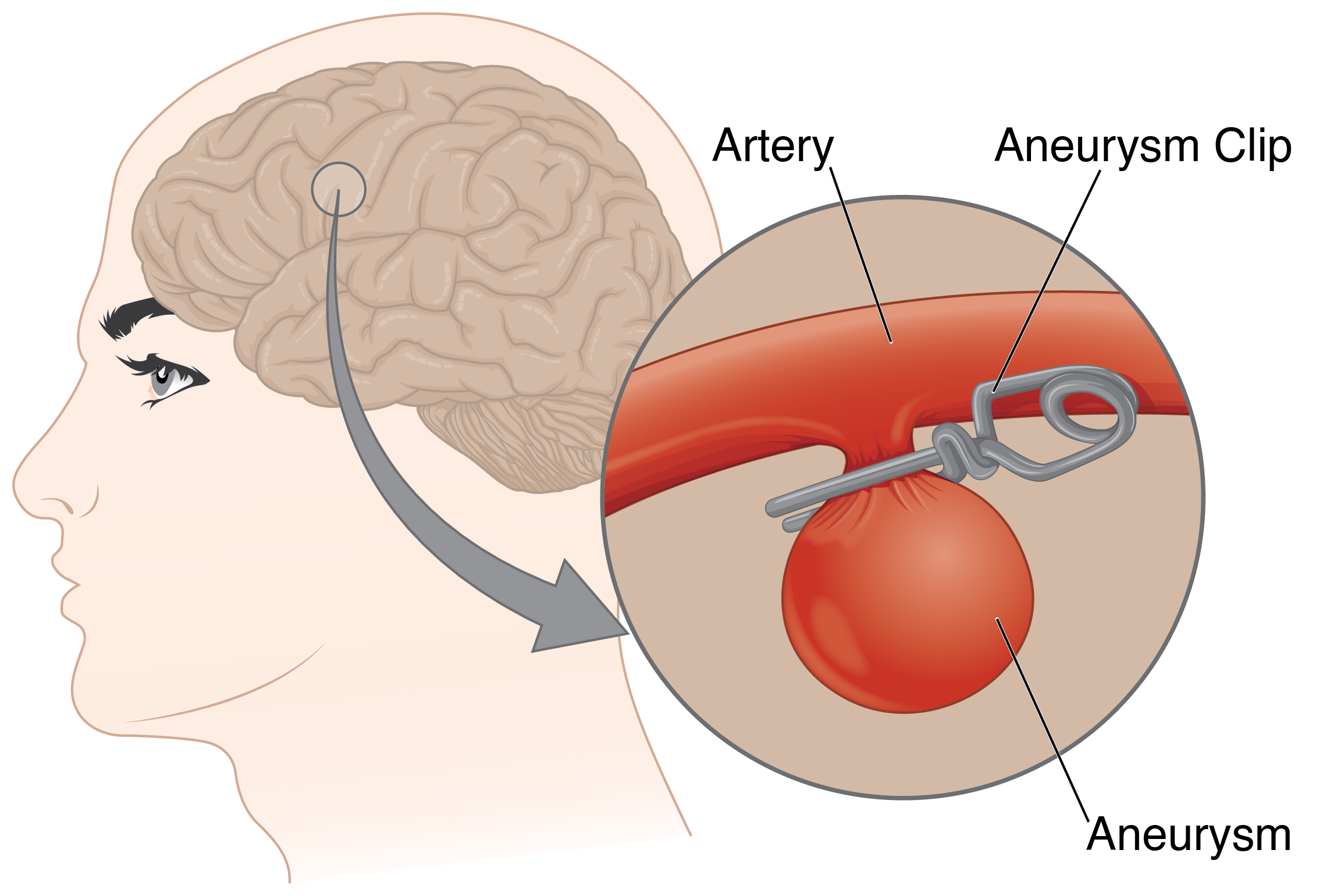
Microsurgical Clipping: The surgeon opens the skull (craniotomy) and applies a metal clip to the neck of the aneurysm, isolating it from circulation. This provides a permanent solution and prevents future rupture.
2. Decompressive Craniectomy
When bleeding causes massive brain swelling or refractory intracranial pressure, a portion of the skull bone is removed. This allows the brain to expand safely without being compressed, reducing the risk of herniation. The bone flap is preserved for later replacement (cranioplasty).
3. Postoperative Management
-
Intensive monitoring in a neuro-ICU
-
Control of intracranial pressure, blood pressure, and oxygenation
-
Administration of nimodipine, a calcium-channel blocker to prevent cerebral vasospasm
-
Management of seizures and hydrocephalus
-
Physical and cognitive rehabilitation to restore neurological functions
4. Cranioplasty
Weeks or months later, once brain swelling has subsided, the removed bone flap or an artificial implant is replaced to protect the brain and restore skull integrity.
Prevention and Management of Craniectomy of Aneurysms / AXM
Preventing aneurysm rupture is the best way to avoid needing such high-risk surgery. Early diagnosis and lifestyle modification play a crucial role.
Preventive Measures:
-
Maintain normal blood pressure through medication, diet, and exercise.
-
Quit smoking and limit alcohol consumption.
-
Regular health check-ups for those with family history of aneurysms.
-
Balanced diet rich in fruits, vegetables, and omega-3 fatty acids.
-
Manage cholesterol and diabetes effectively.
Post-Surgical Management:
-
Continuous neuro-rehabilitation for physical strength, balance, and coordination.
-
Cognitive therapy for memory, attention, and speech recovery.
-
Regular imaging scans to monitor for new or residual aneurysms.
-
Psychological support to help patients deal with anxiety, depression, or post-surgical stress.
Preventive efforts combined with early intervention dramatically improve long-term outcomes and reduce the risk of future brain injury.
Complications of Craniectomy of Aneurysms / AXM
Although craniectomy is often life-saving, it carries certain risks and complications.
Short-Term Complications:
-
Bleeding or hematoma formation at the surgical site
-
Infection of the wound or bone flap
-
Brain swelling or ischemia if pressure persists
-
Seizures after surgery
-
Cerebral vasospasm, a narrowing of brain arteries leading to delayed strokes
Long-Term Complications:
-
Hydrocephalus (fluid buildup in the brain)
-
Neurological deficits such as weakness, difficulty speaking, or memory loss
-
Syndrome of the Trephined, a condition where patients experience dizziness, headaches, or cognitive decline due to the skull defect before cranioplasty
-
Cosmetic deformity at the surgical site
-
Bone flap resorption or displacement after replacement
With skilled surgical care, infection control, and continuous rehabilitation, most complications can be minimized or successfully managed.
Living with the Condition of Craniectomy of Aneurysms / AXM
Life after aneurysm surgery and craniectomy involves a journey of recovery and adaptation. The patient's determination, rehabilitation, and medical follow-up play key roles in long-term recovery.
Rehabilitation and Recovery:
Patients often undergo multidisciplinary rehabilitation, including physical therapy to regain strength, occupational therapy for daily activities, and speech therapy for communication recovery. Cognitive rehabilitation helps with concentration, memory, and executive functions.
Lifestyle Adjustments:
-
Maintain a balanced, low-salt diet and stay hydrated.
-
Avoid smoking, stress, and heavy physical exertion until medically cleared.
-
Continue regular follow-up imaging to monitor brain healing.
-
Wear protective headgear if the bone flap hasn't yet been replaced.
-
Ensure good sleep and stress management for brain recovery.
Psychological and Emotional Support:
Depression and anxiety are common after brain surgery. Family counseling, patient education, and support groups can help patients and caregivers cope better.
Long-Term Outlook:
With modern surgical advances and rehabilitation, many patients lead productive, fulfilling lives after craniectomy for aneurysm. Recovery may take several months, but most individuals regain independence with proper care and follow-up.
Top 10 Frequently Asked Questions about Craniectomy for Aneurysms (AXM)
1. What is Craniectomy for Aneurysms (AXM)?
Craniectomy for aneurysms, also known as decompressive craniectomy in the context of aneurysmal subarachnoid hemorrhage (aSAH), is a neurosurgical procedure where a portion of the skull is removed to alleviate increased intracranial pressure (ICP) caused by a ruptured brain aneurysm. This procedure is typically performed when medical management fails to control ICP, and it aims to prevent brain herniation and further neurological damage.
2. Why is Craniectomy performed in Aneurysmal Subarachnoid Hemorrhage (aSAH)?
In aSAH, a ruptured aneurysm leads to bleeding in the subarachnoid space, increasing ICP. If ICP remains elevated despite medical interventions, decompressive craniectomy is considered as a last-resort measure to:
-
Reduce ICP and prevent herniation
-
Improve cerebral perfusion
-
Enhance the effectiveness of other treatments like aneurysm clipping or coiling
It's important to note that while craniectomy can improve survival rates, it may not always result in full neurological recovery.
3. How is the Craniectomy Procedure Performed?
The procedure involves:
-
Anesthesia: General anesthesia is administered.
-
Incision: A portion of the scalp is shaved and an incision is made.
-
Bone Removal: A section of the skull is removed to allow the brain to expand.
-
Brain Exposure: The dura mater (brain covering) may be opened to further relieve pressure.
-
Closure: The scalp is closed over the exposed brain; the bone flap may be preserved for later replacement.
In some cases, additional procedures like aneurysm clipping or coiling are performed during the same surgery.
4. What are the Risks and Complications?
While craniectomy can be life-saving, it carries potential risks, including:
-
Infection at the surgical site
-
Bleeding or hematoma formation
-
Seizures
-
Neurological deficits such as weakness, speech difficulties, or cognitive impairments
-
Hydrocephalus (fluid accumulation in the brain)
-
Delayed bone flap infection or resorption
The decision to perform craniectomy is carefully considered by the medical team based on the patient's condition and potential benefits.
5. What is the Recovery Process Like?
Post-surgery, patients are closely monitored in an intensive care unit (ICU). Recovery involves:
-
Monitoring for complications like infection or seizures
-
Gradual reintroduction of physical activity
-
Rehabilitation therapies (physical, occupational, speech) to address any deficits
-
Regular follow-up imaging to assess brain healing
The timeline for recovery varies; some patients may require several months to a year for full recovery, depending on the severity of the initial condition and the success of rehabilitation efforts.
6. Will the Bone Removed During Surgery Be Replaced?
Yes, the bone flap removed during craniectomy is typically preserved and reimplanted in a separate surgery called cranioplasty. This procedure is usually performed once the brain has healed sufficiently and swelling has reduced. In some cases, if the original bone is not viable, synthetic materials or titanium plates may be used to reconstruct the skull.
7. How Does Craniectomy Affect Long-Term Brain Function?
The impact on long-term brain function depends on several factors:
-
The extent of brain injury prior to surgery
-
The presence of other complications like infections or seizures
-
The effectiveness of rehabilitation
Some patients experience significant recovery, while others may have lasting neurological impairments. Early and intensive rehabilitation can improve outcomes.
8. Are There Alternatives to Craniectomy in Aneurysmal Subarachnoid Hemorrhage?
Alternative treatments focus on controlling ICP and preventing further brain injury:
-
Medical management with hyperosmolar therapy (e.g., mannitol)
-
Sedation and analgesia to reduce metabolic demand
-
Aneurysm repair through clipping or coiling
-
External ventricular drainage for hydrocephalus
Craniectomy is considered when these measures fail to control ICP and the patient's condition is deteriorating.
9. How Should I Prepare for Craniectomy Surgery?
Preparation involves:
-
Preoperative imaging (CT/MRI) to assess brain condition
-
Blood tests and other assessments to evaluate overall health
-
Discussion of medication adjustments, especially anticoagulants
-
Arrangements for post-surgery care and rehabilitation
As craniectomy is often performed in emergency situations, preparation is typically rapid and coordinated by the surgical team.
10. What is the Prognosis After Craniectomy for Aneurysms?
The prognosis varies widely:
-
Some patients experience full recovery, especially if the aneurysm was treated promptly and effectively
-
Others may have permanent neurological deficits, depending on the extent of brain injury
-
Factors influencing prognosis include age, overall health, the severity of the initial hemorrhage, and the timeliness of surgical intervention
Ongoing medical care, rehabilitation, and lifestyle adjustments play crucial roles in recovery and quality of life post-surgery.


