Introduction to Debridement of Wound, Burn, or Infection
Debridement is a critical medical procedure that involves the removal of dead, damaged, or infected tissue to improve the healing potential of the remaining healthy tissue. It is an essential step in the management of chronic wounds, burns, and infections where necrotic (dead) tissue impedes the natural healing process or promotes bacterial growth.
When a wound becomes contaminated or develops dead tissue, the body's ability to heal is significantly compromised. This dead tissue not only delays healing but also acts as a medium for bacteria, increasing the risk of severe infection such as cellulitis, sepsis, or gangrene. Through debridement, the wound bed is cleansed and prepared for new tissue formation, reducing infection risk and enhancing the effectiveness of subsequent therapies such as skin grafting, antibiotics, or dressings.
Debridement can be performed surgically, mechanically, chemically (enzymatic), or biologically (maggot therapy), depending on the nature and severity of the wound. Modern wound-care practices rely on a multidisciplinary approach, combining surgical precision, infection control, and advanced dressing technology to promote optimal outcomes.
This procedure plays a vital role not only in trauma and burn management but also in chronic conditions such as diabetic ulcers, pressure sores, and vascular wounds-conditions that often affect millions worldwide.
Causes and Risk Factors Leading to Debridement
Debridement is not a standalone disease but a treatment approach for wounds that fail to heal properly. Understanding the causes of wounds requiring debridement helps in prevention and management.
Common Causes
-
Traumatic Injuries: Road accidents, cuts, or crush injuries may lead to tissue necrosis and contamination.
-
Burns: Thermal, electrical, or chemical burns cause varying depths of tissue death requiring removal to prevent infection.
-
Infected Surgical Wounds: Postoperative infections may produce necrotic tissue or pus that must be cleared for healing.
-
Chronic Ulcers:
-
Diabetic Foot Ulcers: Poor circulation and neuropathy in diabetics lead to deep infected wounds.
-
Pressure Ulcers: Caused by prolonged pressure on skin (bedridden or wheelchair-bound patients).
-
Venous or Arterial Ulcers: Poor blood flow impairs healing and leads to tissue death.
-
-
Ischemic Tissue Necrosis: From poor oxygenation due to vascular diseases.
-
Radiation or Chemical Injuries: Exposure may destroy soft tissue, requiring removal of damaged areas.
Risk Factors
-
Uncontrolled diabetes mellitus
-
Peripheral artery disease or venous insufficiency
-
Immune suppression (HIV, chemotherapy, corticosteroids)
-
Malnutrition, which delays wound healing
-
Poor hygiene and wound care practices
-
Advanced age, where tissue regeneration slows
-
Smoking and alcohol abuse, both of which impair circulation and oxygenation
Symptoms and Signs Indicating the Need for Debridement
The signs that a wound, burn, or infection requires debridement are primarily related to the presence of necrotic or infected tissue and poor wound healing.
Visible Signs
-
Black, brown, yellow, or green patches in the wound (necrotic slough or eschar)
-
Foul-smelling discharge or pus from the wound site
-
Swelling, redness, and warmth around the wound (local infection)
-
Visible blisters or dried scabs preventing healing
-
Wound edges that are not closing or healing over time
-
Deep tissue exposure (muscle, tendon, or bone) with dead tissue
-
Excessive exudate (fluid discharge) or bleeding after minimal touch
Systemic Symptoms
-
Fever, chills, and fatigue (signs of systemic infection or sepsis)
-
Increased pain and tenderness around the wound
-
Elevated blood glucose levels in diabetic patients with infected ulcers
-
Delay in wound granulation (formation of new tissue)
Recognizing these signs early is crucial because delays can allow infection to spread to deeper structures, leading to osteomyelitis (bone infection) or amputation in severe cases.
Diagnosis and Assessment Before Debridement
Before proceeding with debridement, a comprehensive wound assessment is performed by a wound-care specialist or surgeon to determine the appropriate method and urgency of treatment.
Clinical Evaluation
-
Detailed medical history: including diabetes, vascular disease, or prior infections.
-
Physical examination: to assess wound type, location, depth, and color.
-
Identification of necrotic tissue and infection level.
Diagnostic Tests
-
Wound Culture and Sensitivity: Identifies bacterial or fungal pathogens to guide antibiotic therapy.
-
Blood Tests: White blood cell count, blood sugar levels, and inflammatory markers (CRP, ESR).
-
Imaging Studies:
-
X-ray: To rule out foreign bodies or bone involvement.
-
MRI/CT Scan: For deep or chronic wounds, to detect abscesses or osteomyelitis.
-
Doppler Ultrasound: To assess blood flow in patients with vascular disease.
-
-
Tissue Biopsy: Confirms infection, malignancy, or necrosis in suspicious wounds.
Assessment Parameters
-
Depth of necrosis (superficial vs. deep tissue involvement)
-
Type of exudate (serous, purulent, hemorrhagic)
-
Perfusion level (blood flow)
-
Pain intensity and infection signs
-
Overall patient health and immune status
This diagnostic process determines whether conservative debridement (gradual removal) or surgical debridement (immediate removal) is indicated.
Treatment Options: Methods of Debridement
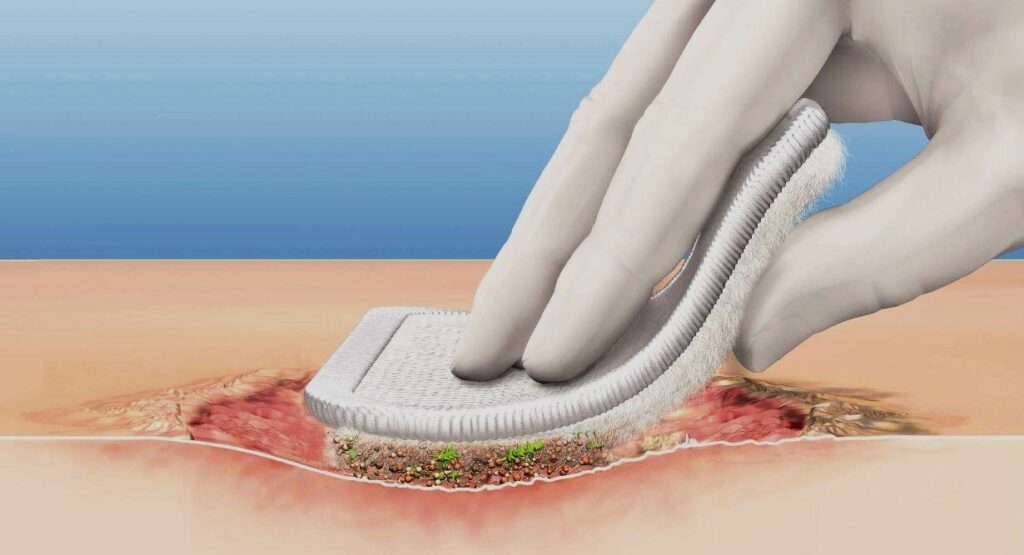
Debridement methods vary according to the wound type, depth, infection status, and patient health. The main goal is to remove all necrotic tissue while preserving viable cells.
1. Surgical (Sharp) Debridement
-
Performed by surgeons using scalpels, scissors, or curettes under sterile conditions.
-
Best suited for extensive necrosis, infected burns, or deep ulcers.
-
Provides immediate results and allows for rapid tissue healing.
-
Often combined with reconstructive procedures such as skin grafts or flaps.
2. Mechanical Debridement
-
Involves physical removal using wet-to-dry dressings, hydrotherapy, or wound irrigation.
-
Effective for moderate necrosis but may be painful and non-selective (can damage healthy tissue).
-
Modern techniques like ultrasonic debridement are more precise and less traumatic.
3. Autolytic Debridement
-
Uses the body's own enzymes and moisture to liquefy dead tissue.
-
Involves use of moisture-retentive dressings such as hydrogels or hydrocolloids.
-
Painless and selective, ideal for non-infected wounds or patients who cannot tolerate surgery.
4. Enzymatic (Chemical) Debridement
-
Utilizes topical enzymes (e.g., collagenase) to break down necrotic tissue.
-
Effective for chronic wounds or burns with slough; can be used alongside other methods.
-
Requires daily dressing changes and monitoring.
5. Biological (Maggot Therapy)
-
Sterile larvae (Lucilia sericata) are introduced into the wound to digest necrotic tissue and secrete antibacterial enzymes.
-
Highly selective and effective in chronic, non-healing wounds resistant to other methods.
-
Used under strict medical supervision.
6. Adjunctive Therapies
-
Negative Pressure Wound Therapy (NPWT): Uses suction to promote drainage and stimulate tissue growth.
-
Hyperbaric Oxygen Therapy (HBOT): Enhances oxygen delivery to healing tissues.
-
Topical antimicrobials: To control bacterial load post-debridement.
Prevention and Management of Wound, Burn, and Infection
Effective prevention and management of wounds, burns, and infections depend on prompt care, proper hygiene, and risk reduction strategies. A multidisciplinary approach ensures healing and minimizes complications for all types of skin injuries.
Preventive Strategies
-
Prompt Wound Care: Clean and dress wounds immediately after injury to prevent infection.
-
Blood Sugar Control: Diabetic patients must maintain stable glucose levels to improve healing.
-
Good Nutrition: Adequate protein, vitamins (A, C, E), and zinc intake supports tissue regeneration.
-
Hygiene and Skin Care: Regular cleaning and moisture management of skin to avoid breakdown.
-
Pressure Relief: For bedridden patients, frequent repositioning prevents pressure ulcers.
-
Smoking Cessation: Improves circulation and oxygen delivery to tissues.
-
Early Intervention: At first sign of delayed healing or infection, seek medical attention.
Wound Management After Debridement
-
Keep wound moist but not overly wet.
-
Use sterile dressings, changed regularly as per medical advice.
-
Apply prescribed antibiotics or topical agents.
-
Monitor for signs of reinfection or delayed healing.
-
Attend follow-up appointments for wound evaluation and dressing review.
Complications of Debridement Of Wound Burn Or Infection
Despite being essential for healing, debridement can occasionally lead to complications, especially in high-risk patients.
Immediate Complications
-
Bleeding from exposed capillaries or vessels.
-
Pain during and after procedure.
-
Allergic reactions to anesthetics or enzymatic agents.
Delayed Complications
-
Infection: If sterile technique is not maintained.
-
Tissue Damage: From aggressive debridement or poor wound care.
-
Scarring or Contracture: Especially in burns or deep wounds.
-
Delayed Healing: In patients with poor vascular supply or immune compromise.
-
Psychological Impact: Long-term wounds and repeated debridement can affect mental health.
Systemic Complications
-
Sepsis: Spread of infection into bloodstream if wound is untreated.
-
Amputation: In severe diabetic or gangrenous cases when tissue death extends too far.
Close monitoring, aseptic technique, and proper wound care minimize these risks significantly.
Living with a Healing Wound After Debridement
Living with a wound that has undergone debridement involves consistent care, patience, and lifestyle modification.
Post-Debridement Recovery
-
Healing time varies depending on wound size, cause, and general health.
-
Follow-up visits are crucial for dressing changes, progress monitoring, and secondary treatments (grafting, reconstruction).
-
Maintain adequate hydration and balanced diet to promote healing.
Pain and Comfort
-
Mild discomfort is normal; pain management may include analgesics or topical anesthetics.
-
Avoid tight clothing or pressure on wound area.
Lifestyle Adjustments
-
Avoid smoking and alcohol consumption.
-
Engage in light physical activity to improve blood flow, unless restricted.
-
Manage chronic diseases like diabetes and hypertension carefully.
Emotional Well-Being
-
Chronic wounds can be psychologically taxing. Support groups, counseling, and education on wound care can improve outlook and confidence.
-
Positive attitude and adherence to medical advice significantly improve outcomes.
Long-Term Outlook
Most patients experience complete recovery if proper wound care and medical follow-up are maintained. However, those with underlying vascular disease or diabetes may need periodic evaluation to prevent recurrence.
Top 10 Frequently Asked Questions about Debridement of Wound, Burn, or Infection
1. What Is Debridement?
Debridement is a medical procedure that involves the removal of dead, damaged, or infected tissue from a wound, burn, or infected area.
The purpose is to:
-
Promote healing
-
Prevent infection spread
-
Reduce tissue necrosis
-
Prepare the wound for further treatments, such as skin grafts
It is an essential step in wound management, especially for chronic, severe, or infected wounds.
2. Why Is Debridement Necessary?
Debridement is crucial because dead tissue prevents proper healing and can become a breeding ground for bacteria, leading to serious infections.
It is commonly indicated for:
-
Burn wounds with dead skin
-
Chronic ulcers (diabetic, pressure, or venous ulcers)
-
Traumatic wounds with necrotic tissue
-
Surgical site infections
-
Gangrene or tissue necrosis
Prompt debridement reduces the risk of severe complications and systemic infections.
3. What Are the Types of Debridement?
Debridement can be performed using several methods:
-
Surgical Debridement: Cutting away dead tissue using scalpels or scissors (most effective for severe wounds)
-
Mechanical Debridement: Physical removal of debris using wet-to-dry dressings or irrigation
-
Autolytic Debridement: Using the body's own enzymes and moisture to dissolve dead tissue (slow but non-invasive)
-
Enzymatic Debridement: Applying topical enzymes to break down necrotic tissue
-
Biological Debridement: Using sterile larvae (maggots) to consume dead tissue
The choice depends on wound type, severity, and patient condition.
4. How Is Surgical Debridement Performed?
Surgical debridement is typically performed under local or general anesthesia, depending on wound size and depth.
Procedure Steps:
-
The wound is cleaned and disinfected.
-
Dead, infected, or damaged tissue is carefully removed with scalpels, scissors, or curettes.
-
The wound is irrigated to remove debris and bacteria.
-
Sometimes wound dressings, negative pressure therapy, or skin grafts are applied to support healing.
Surgical debridement is usually quick, precise, and effective, especially for infected or necrotic wounds.
5. Is Debridement Painful?
Pain management depends on the type and extent of debridement:
-
Surgical or mechanical debridement: Usually performed under anesthesia or sedation to minimize discomfort.
-
Autolytic or enzymatic debridement: Generally painless, though mild irritation may occur.
-
Post-procedure, mild pain or tenderness is normal and can be managed with analgesics.
6. What Are the Risks or Complications?
Debridement is generally safe, but potential risks include:
-
Bleeding
-
Infection if sterility is compromised
-
Damage to healthy tissue
-
Delayed wound healing in patients with diabetes or poor circulation
-
Pain or discomfort during or after the procedure
These risks are minimized with proper surgical technique, sterile environment, and post-procedure wound care.
7. How Long Does It Take to Heal After Debridement?
Healing depends on the wound type, size, depth, and patient health:
-
Small, superficial wounds: May heal within 1–2 weeks
-
Large or chronic wounds: May require several weeks to months, sometimes needing additional treatments like skin grafts or negative pressure therapy
-
Proper nutrition, blood sugar control, and infection management are critical for faster healing
8. Can Debridement Prevent Infection?
Yes. By removing dead tissue, debridement eliminates the medium where bacteria thrive, significantly reducing the risk of:
-
Wound infection
-
Sepsis in severe cases
-
Spread of necrosis to surrounding tissues
Early intervention is particularly important for diabetic ulcers, burn wounds, and surgical site infections.
9. Are There Non-Surgical Alternatives to Debridement?
Yes, for certain wounds:
-
Autolytic debridement using dressings that maintain a moist environment
-
Enzymatic topical agents that digest necrotic tissue
-
Biological debridement with sterile larvae (maggot therapy)
-
Hydrotherapy or saline irrigation for mild or superficial necrotic tissue
Non-surgical methods are slower but less invasive, suitable for patients who cannot undergo surgery.
10. How Can I Care for My Wound After Debridement?
Proper post-debridement care is essential for optimal healing:
-
Keep the wound clean and dry as instructed
-
Change dressings regularly and follow medical guidance
-
Take prescribed antibiotics or analgesics
-
Avoid trauma or pressure on the wound area
-
Maintain good nutrition and hydration
-
Attend follow-up appointments for monitoring and additional treatments if needed
Adhering to post-procedure instructions reduces infection risk and promotes faster recovery.


