Introduction to Diagnostic Laparoscopy with Biopsy
Diagnostic Laparoscopy with Biopsy is a minimally invasive surgical technique used by surgeons to look directly inside the abdomen and pelvis and obtain tissue samples for microscopic examination. It serves as a bridge between non-invasive imaging tests and traditional open surgery, providing both visual confirmation and tissue diagnosis in one safe, precise procedure.
In this technique, a laparoscope-a slender, tube-like instrument with a high-resolution camera and light source-is inserted through a small incision near the navel. The abdominal cavity is gently inflated with carbon dioxide gas, which lifts the abdominal wall away from the organs, creating space for safe inspection. The surgeon can then observe the internal organs in real-time on a video monitor and use fine instruments inserted through additional small incisions to remove tiny samples of tissue (biopsies) from suspicious areas such as the liver, peritoneum, lymph nodes, ovaries, or intestines.
The biopsy specimens are later analyzed under a microscope by a pathologist to confirm or rule out diseases like cancer, tuberculosis, infection, cirrhosis, or endometriosis. Because the incisions are small and recovery is rapid, patients experience minimal pain, reduced scarring, and faster return to daily activities compared to traditional open exploratory surgery.
Diagnostic laparoscopy with biopsy has become an essential tool in modern medicine. It not only enhances diagnostic accuracy but also allows early intervention-sometimes in the same sitting-when the surgeon identifies treatable conditions.
Causes and Risk of Diagnostic Laparoscopy with Biopsy
Diagnostic laparoscopy with biopsy is performed when non-invasive methods fail to identify the cause of a patient's symptoms, or when visual confirmation and tissue diagnosis are necessary.
A. Common Indications (Causes for Performing the Procedure)
There are several medical situations in which diagnostic laparoscopy with biopsy is recommended. It is primarily performed when the cause of abdominal or pelvic symptoms remains uncertain after standard imaging and laboratory investigations. Key indications include:
-
Unexplained Abdominal Pain:
When imaging tests fail to reveal the reason for persistent abdominal discomfort, laparoscopy allows the surgeon to directly view the abdominal cavity for possible causes such as adhesions, inflammation, or hidden pathology. -
Detection and Staging of Cancer:
In suspected malignancies of the liver, stomach, pancreas, ovary, or peritoneum, laparoscopy with biopsy confirms the diagnosis and determines the extent of cancer spread. It is often used to guide treatment decisions before chemotherapy or major surgery. -
Evaluation of Abdominal or Pelvic Masses:
When a mass is found on imaging, a biopsy through laparoscopy helps distinguish between benign (non-cancerous) and malignant (cancerous) growths. -
Unexplained Fluid in the Abdomen (Ascites):
The cause of ascites-whether infection, liver disease, or cancer-can be determined through laparoscopy and biopsy of the peritoneum. -
Infertility and Gynecological Disorders:
In women, laparoscopy identifies conditions like endometriosis, pelvic inflammatory disease, adhesions, and tubal blockages, and biopsies confirm the presence of disease. -
Chronic Infections and Tuberculosis:
When abdominal tuberculosis or other chronic infections are suspected, a peritoneal biopsy provides the most reliable diagnostic confirmation. -
Unexplained Weight Loss or Fever:
Laparoscopy may be indicated to rule out hidden infections, inflammatory diseases, or cancers. -
Trauma Assessment:
In cases of abdominal trauma where internal bleeding or organ damage is suspected but not clear on scans, laparoscopy helps evaluate the injury and control bleeding if necessary.
B. Risks and Considerations
While diagnostic laparoscopy with biopsy is generally safe, as with any surgical procedure, there are some potential risks:
-
Bleeding: Small blood vessels can be damaged during port insertion or biopsy, especially in vascular organs like the liver.
-
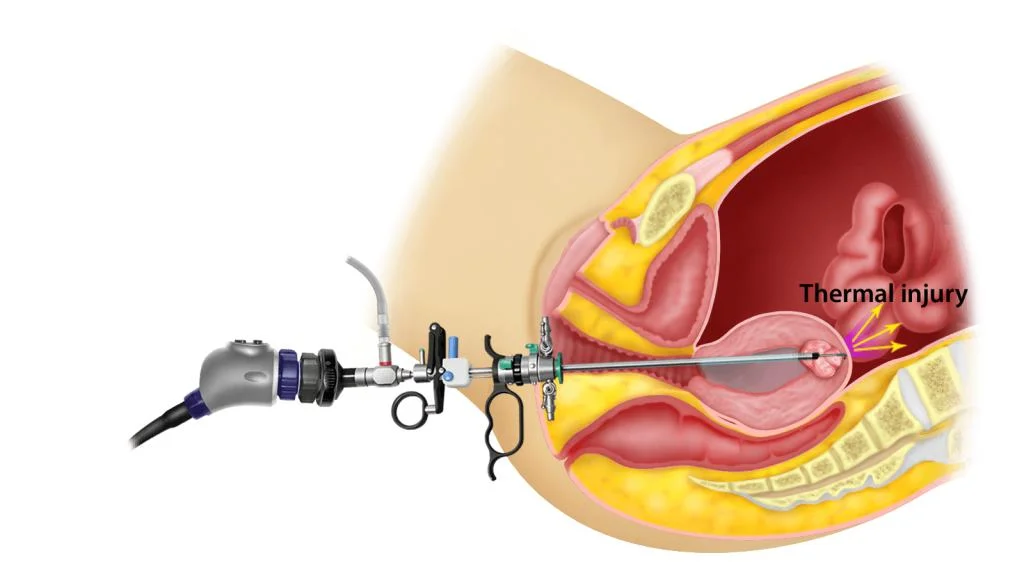
Injury to Internal Organs: Accidental injury to the intestines, bladder, or blood vessels can occur but is rare with skilled surgeons.
-
Infection: Risk of wound infection or, rarely, intra-abdominal infection exists.
-
Adverse Reactions to Anesthesia: Such as nausea, dizziness, or allergic responses.
-
Gas-related Discomfort: Shoulder or abdominal pain due to the gas used for insufflation.
-
Conversion to Open Surgery: If visualization is poor or complications arise, the surgeon may need to switch to a traditional open approach.
Despite these risks, diagnostic laparoscopy with biopsy remains safer, quicker, and less traumatic than open surgical exploration.
Symptoms and Signs Leading to Diagnostic Laparoscopy with Biopsy
Patients undergoing diagnostic laparoscopy with biopsy typically present with persistent or unexplained abdominal or pelvic symptoms that require a deeper look beyond imaging. Common clinical presentations include:
A. Symptoms Before the Procedure
-
Chronic or recurrent abdominal pain without a clear cause.
-
Unexplained bloating, distension, or pressure in the abdomen.
-
Weight loss, loss of appetite, or fatigue.
-
Unexplained fever or malaise.
-
Presence of lumps or swelling felt on examination.
-
Jaundice or liver enlargement suggesting liver pathology.
-
Abnormal menstrual cycles or infertility in women.
-
Ascites (fluid buildup) not explained by routine investigations.
-
Abnormal findings on ultrasound, CT, or MRI scans requiring tissue diagnosis.
B. Post-Procedure Signs
After the procedure, mild and temporary effects may include:
-
Slight abdominal pain or cramping.
-
Shoulder discomfort due to residual gas.
-
Minimal bleeding or bruising at incision sites.
-
Temporary tiredness or mild nausea.
-
Full recovery usually occurs within a few days.
These are normal postoperative experiences and resolve as the body heals.
Diagnosis and Preoperative Evaluation
Diagnosis and preoperative evaluation for diagnostic laparoscopy ensure patient safety, proper surgical planning, and accurate diagnosis. The process combines clinical assessment, targeted laboratory tests, imaging, and careful preparation for the procedure.
A. Preoperative Assessment
Before performing diagnostic laparoscopy with biopsy, a thorough evaluation ensures patient safety and success of the procedure. This includes:
-
Medical History:
Reviewing any previous abdominal surgeries, bleeding disorders, allergies, and chronic illnesses such as hypertension or diabetes. -
Physical Examination:
Assessing abdominal tenderness, organ enlargement, and ascitic fluid. -
Laboratory Investigations:
-
Blood counts and coagulation profile.
-
Liver and kidney function tests.
-
Viral markers (Hepatitis B, C, HIV) if liver biopsy is planned.
-
Tumor markers (CA-125, AFP, CEA) if cancer is suspected.
-
Pregnancy test for women of reproductive age.
-
-
Imaging Studies:
-
Ultrasound: First-line for assessing liver, gallbladder, ovaries, or free fluid.
-
CT or MRI scans: For detailed visualization of deeper structures.
-
PET scan: For cancer staging if needed.
-
-
Anesthesia Clearance:
Ensures fitness for general anesthesia and assesses cardiac and respiratory health.
B. Diagnostic Advantage
Diagnostic laparoscopy with biopsy provides a direct visual confirmation that no imaging test can match. The surgeon can see abnormalities in color, texture, and structure of internal organs and immediately obtain tissue samples for histological study. This combination of visual and microscopic analysis provides the highest accuracy in diagnosing abdominal and pelvic diseases.
Treatment Options and Surgical Procedure
Diagnostic laparoscopy is a minimally invasive procedure that enables direct visualization and, if necessary, surgical intervention in the abdomen or pelvis. It provides both diagnosis and the ability for ancillary treatments, with a focus on minimal trauma and rapid recovery.
A. Step-by-Step Description of the Procedure
-
Anesthesia:
The patient is placed under general anesthesia to ensure complete comfort and immobility. -
Positioning and Sterilization:
The patient lies on their back; the abdominal area is cleaned with antiseptic solution and covered with sterile drapes. -
Creating Pneumoperitoneum:
A small incision (about 1 cm) is made near the navel. Carbon dioxide gas is introduced into the abdomen to create space for visibility. -
Insertion of the Laparoscope:
The laparoscope is gently inserted through the incision, allowing the surgeon to inspect internal organs on a video monitor. -
Inspection of the Abdomen and Pelvis:
The surgeon systematically examines organs such as the liver, gallbladder, stomach, intestines, uterus, ovaries, and peritoneum, identifying any abnormality like inflammation, nodules, or fluid collections. -
Taking the Biopsy:
Using fine laparoscopic instruments, small samples of tissue are taken from the suspected area.-
Liver biopsies for cirrhosis or cancer.
-
Peritoneal biopsies for tuberculosis or carcinomatosis.
-
Ovarian or uterine biopsies in gynecologic cases.
-
Lymph node biopsies for lymphoma or metastasis.
-
-
Specimen Handling:
Biopsy specimens are labeled and sent to a pathology laboratory for analysis under a microscope. -
Completion and Closure:
After inspection, the gas is released, instruments are withdrawn, and small incisions are closed with dissolvable sutures.
The entire procedure usually lasts 30 to 90 minutes, depending on complexity.
B. Postoperative Care
After surgery:
-
Patients are observed until fully awake from anesthesia.
-
Oral intake resumes a few hours after recovery.
-
Mild painkillers and antibiotics are prescribed.
-
Most patients are discharged the same or next day.
-
The surgeon reviews the biopsy report in 5-7 days to plan further treatment.
Prevention and Management of Diagnostic Laparoscopy with Biopsy
Prevention and management of complications after double outlet right ventricle (DORV) repair focus on optimizing surgical outcomes, preventing postoperative complications, and providing comprehensive long-term follow-up. While DORV itself cannot currently be prevented, proactive strategies can reduce risks and improve post-surgical quality of life.
A. Preventing Complications
Although diagnostic laparoscopy with biopsy is safe, optimal outcomes depend on:
-
Preoperative optimization - treating anemia, controlling diabetes, and ensuring sterile technique.
-
Experienced surgical team - minimizes organ injury and bleeding risk.
-
Careful selection of biopsy site - choosing accessible and safe areas under direct vision.
-
Prophylactic antibiotics to prevent infection.
-
Adequate patient education regarding post-procedure care.
B. Postoperative Management
Effective postoperative care accelerates recovery and prevents complications:
-
Rest for 24 hours and resume light activity after 2-3 days.
-
Maintain hygiene of incision sites.
-
Avoid heavy lifting or strenuous activity for one week.
-
Report fever, redness, or discharge immediately.
-
Eat light meals initially and stay hydrated.
-
Use prescribed medication as directed.
-
Attend follow-up for biopsy results and further care planning.
With proper management, most patients recover fully within a week.
Complications of Diagnostic Laparoscopy with Biopsy
While complications are rare, it's important to recognize possible outcomes early for prompt management:
-
Bleeding: From biopsy sites or trocar insertion areas.
-
Infection: Local wound infection or intra-abdominal abscess formation.
-
Injury to Organs: Accidental puncture or tear in bowel, bladder, or blood vessels.
-
Gas-related Symptoms: Shoulder or chest pain due to CO₂ insufflation.
-
Anesthesia-Related Issues: Nausea, vomiting, or allergic reactions.
-
Conversion to Open Surgery: Required if severe bleeding or dense adhesions are found.
-
Postoperative Adhesions: Rare scar tissue formation that may cause discomfort later.
All these are uncommon when the procedure is performed by experienced laparoscopic surgeons in a well-equipped setting.
Living with the Condition After Diagnostic Laparoscopy with Biopsy
Living after a diagnostic laparoscopy with biopsy is typically smooth and allows for rapid recovery, but requires attention to incision care, gradual return to activities, and awareness of your body's healing signals. Most people recover rapidly and can expect to return to light normal life within a week, with some variations depending on what was found and biopsied.
A. Recovery Experience
Most patients recover rapidly with minimal discomfort. Mild bloating or shoulder pain may persist briefly as the body absorbs the CO₂ gas. Proper wound care and adherence to follow-up schedules ensure uneventful healing.
B. Impact of Biopsy Results
The results of the biopsy determine the next phase of management:
-
Benign findings may require medical management or observation only.
-
Infectious causes (like tuberculosis) are treated with specific drug regimens.
-
Cancerous findings guide oncologists in staging and therapy planning.
C. Lifestyle and Long-Term Management
-
Eat a balanced diet rich in protein, vitamins, and fluids to aid healing.
-
Avoid smoking and alcohol, which delay recovery.
-
Maintain a healthy weight to prevent complications from abdominal pressure.
-
Regular medical follow-ups are crucial if chronic or malignant diseases are detected.
D. Emotional and Psychological Well-being
Undergoing a diagnostic procedure can be stressful. Patients benefit from clear communication about results and reassurance about treatment plans. Support groups and counseling are encouraged, especially for those diagnosed with chronic illness or cancer.
Top 10 Frequently Asked Questions about Diagnostic Laparoscopy with Biopsy
1. What is Diagnostic Laparoscopy with Biopsy?
Diagnostic laparoscopy with biopsy is a minimally invasive surgical procedure used to examine the organs inside the abdomen and pelvis. It combines the diagnostic capabilities of laparoscopy with the ability to take tissue samples (biopsies) for laboratory analysis. This helps in identifying the cause of unexplained abdominal or pelvic conditions such as infections, tumors, or inflammatory diseases.
2. Why is Diagnostic Laparoscopy with Biopsy performed?
This procedure is recommended when:
-
Imaging tests (like ultrasound, MRI, or CT scans) are inconclusive
-
There is unexplained abdominal or pelvic pain
-
Suspicious masses, cysts, or tumors are detected
-
Infertility evaluation is needed to assess pelvic organs
-
Endometriosis or adhesions are suspected
-
To confirm the diagnosis of infections, cancer, or inflammatory conditions
The biopsy provides definitive histological information, guiding treatment decisions.
3. How is the Procedure Performed?
-
Anesthesia: General anesthesia is administered to ensure comfort.
-
Incision and Insufflation: A small incision is made near the navel, and carbon dioxide gas inflates the abdomen for better visualization.
-
Laparoscope Insertion: A laparoscope (camera) is inserted to examine the organs.
-
Tissue Sampling: If abnormal areas are identified, a small piece of tissue is taken for laboratory biopsy.
-
Closure: Incisions are closed with sutures or surgical glue, and dressings are applied.
The procedure typically takes 30 minutes to 1 hour, depending on complexity.
4. Is Diagnostic Laparoscopy with Biopsy Painful?
-
During the procedure: No pain, as the patient is under anesthesia.
-
Post-procedure: Patients may experience mild abdominal discomfort, bloating, or shoulder pain (due to gas used for inflation).
-
Pain is usually manageable with prescribed or over-the-counter medications.
5. How Should Patients Prepare for the Procedure?
-
Fasting: Avoid food or drink for 6-8 hours prior.
-
Medication Review: Some medications, especially blood thinners, may need to be paused.
-
Medical History: Inform the surgeon about previous surgeries, allergies, or medical conditions.
-
Arrange Transportation: Anesthesia requires someone to drive you home.
-
Consent: Understand the procedure, risks, recovery, and the purpose of the biopsy.
6. What Are the Risks and Complications?
While generally safe, potential risks include:
-
Infection at the incision site
-
Bleeding or hematoma formation
-
Organ or blood vessel injury (rare)
-
Reactions to anesthesia
-
Postoperative hernias
-
Pain or discomfort at the biopsy site
Careful surgical technique minimizes these risks.
7. What Can I Expect After the Procedure?
-
Recovery: Most patients go home the same day or the next day.
-
Postoperative Care: Keep the incision clean, monitor for infection, and follow prescribed medications.
-
Activity Restrictions: Avoid heavy lifting or strenuous activity for 1-2 weeks.
-
Follow-Up: A check-up to review biopsy results and ensure proper healing.
Full recovery typically occurs within 1-2 weeks.
8. How Long Does It Take to Get Biopsy Results?
-
Biopsy samples are sent to a laboratory for histopathological analysis.
-
Results usually take 3-10 days, depending on the complexity of the analysis.
-
These results help determine further treatment, such as medication, surgery, or other interventions.
9. Can Conditions Be Treated During Diagnostic Laparoscopy with Biopsy?
Yes. If abnormalities are found, the surgeon may:
-
Remove adhesions or scar tissue
-
Excise ovarian cysts or small tumors
-
Perform minor surgical repairs
This combination of diagnosis and immediate treatment reduces the need for additional surgeries.
10. How Accurate is Diagnostic Laparoscopy with Biopsy?
-
Diagnostic laparoscopy provides direct visualization of abdominal and pelvic organs, making it highly accurate.
-
When combined with biopsy, it offers definitive diagnosis of conditions like cancer, endometriosis, infections, or inflammatory diseases.
-
Accuracy depends on surgeon expertise, thorough examination, and proper biopsy technique.


