Introduction to Diagnostic Laparoscopy
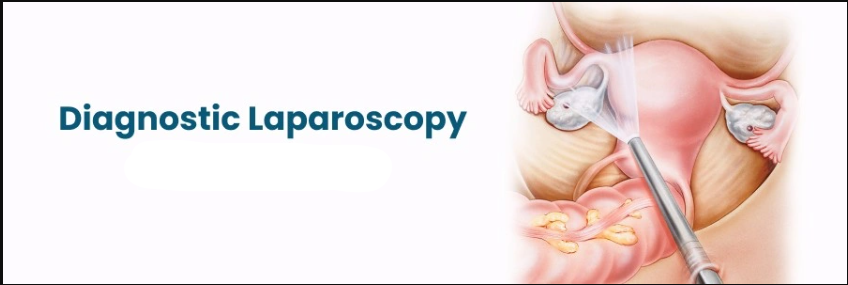
Diagnostic laparoscopy is a minimally invasive surgical procedure in which a surgeon uses a thin, lighted tube (a laparoscope) inserted through a small incision in the abdomen to directly view the organs of the abdomen and pelvis. The goal is to investigate unexplained abdominal or pelvic symptoms, assess the extent of disease (such as cancer), evaluate injury (after trauma), or take targeted biopsies of tissue that cannot be fully assessed via imaging. The technique provides direct visualization of organs such as the liver, gallbladder, appendix, pancreas, small- and large-bowel, ovaries, fallopian tubes, uterus, spleen and peritoneal surfaces. Compared to traditional open surgery (laparotomy), diagnostic laparoscopy offers reduced postoperative pain, shorter hospital stay, faster recovery and fewer complications, making it an invaluable tool in modern surgical diagnostics.
The procedure is indicated when non-invasive tests (imaging, labs, ultrasound) fail to yield a clear diagnosis and when visual inspection plus potential biopsy may govern further management. With advances in instrumentation and imaging, surgeons are increasingly able to combine diagnostic laparoscopy with therapeutic interventions in the same session, blurring the line between "diagnostic" and "operative" laparoscopy.
Causes and Risks of Diagnostic Laparoscopy
Diagnostic laparoscopy is a minimally invasive surgical procedure used to look inside the abdomen and pelvis for diagnosis, but it carries specific risks and complications related to access, visualization, and the underlying condition being assessed.
Causes (Indications)
Diagnostic laparoscopy is performed for a variety of clinical situations where direct visual inspection and/or tissue sampling may influence diagnosis or treatment. Common indications include:
-
Persistent or unexplained abdominal pain despite imaging and labs.
-
Suspected intra-abdominal or pelvic pathology (e.g., endometriosis, adhesions) when non-invasive methods are inconclusive.
-
Suspected malignancy (abdominal or pelvic) where staging (extent of spread) matters.
-
Evaluation of ascites or intra-abdominal fluid of unknown origin.
-
Trauma cases (hemodynamically stable) where internal organ injury is suspected but imaging is deficient.
-
Infertility investigations (in gynecologic situations) where fallopian tube patency, adhesions or endometriosis may be evaluated.
Risks Associated with the Procedure
While diagnostic laparoscopy is generally safe when performed by experienced teams, it is still a surgical procedure and carries risks. Some of the key risks include:
-
Injury to intra-abdominal organs (bowel, bladder, blood vessels) especially during insertion of the trocar or due to adhesions from prior surgery.
-
Bleeding into the abdominal cavity.
-
Infection of the incisions or intra-abdominal infection.
-
Complications from anesthesia (general or sedation).
-
Gas-related complications: pneumoperitoneum (carbon dioxide insufflation) may lead to shoulder pain, elevated intra-abdominal pressure, or cardiovascular/respiratory effects in vulnerable patients.
-
Conversion to open surgery if visualization is inadequate or complications arise.
-
In patients with prior surgeries or dense adhesions, the risk of complication is higher and laparoscopy may be contraindicated or less effective.
Thus, patient selection, preoperative planning and informed consent are critical.
Symptoms and Signs of Diagnostic Laparoscopy
Since diagnostic laparoscopy is a procedure, it is helpful to view this section in two parts: (a) the clinical signs/symptoms that lead to the decision to perform the procedure, and (b) postoperative signs and symptoms to monitor after the procedure.
A. Preoperative Signs & Symptoms
Patients who are candidates for diagnostic laparoscopy often present with:
-
Abdominal or pelvic pain that is persistent, unexplained by imaging or labs.
-
Distension or accumulation of fluid in the abdomen (ascites) without clear cause.
-
Unexplained infertility or pelvic pain in gynecologic settings.
-
Suspected intra-abdominal malignancy (e.g., mass on imaging) with need to assess spread or stage.
-
History of trauma (blunt or penetrating) where internal organ injury is suspected but imaging is unclear.
-
Symptoms of bowel obstruction or internal bleeding when non-invasive imaging is insufficient.
B. Postoperative Signs & Monitoring
After diagnostic laparoscopy, the following signs and symptoms are generally expected or should be monitored:
-
Mild discomfort or pain at the incision sites for a few days.
-
Some bloating or shoulder pain (referred pain) due to the gas (CO₂) used to inflate the abdomen.
-
Slight urge to urinate more frequently or minor bladder pressure (due to pneumoperitoneum).
-
Small amount of abdominal bloating, mild gas pain or belching as the body clears residual gas.
-
The incisions must be monitored for redness, swelling or discharge (signs of infection).
-
Any new onset of severe pain, fever, bleeding, dizziness or signs of bowel/bladder injury should prompt urgent evaluation.
Understanding both sets of symptoms helps patients and clinicians anticipate the procedure and enhance postoperative monitoring.
Diagnosis of Diagnostic Laparoscopy
Here again the term "diagnosis" refers to the pre-procedural workup (how we decide the procedure is needed) plus the intra-operative findings and how they lead to diagnosis.
A. Pre-Procedural Evaluation
Before embarking on diagnostic laparoscopy, thorough evaluation is conducted including:
-
Detailed medical history and physical examination, reviewing prior surgeries, comorbidities, signs of infection, trauma history, fertility issues, cancer history.
-
Laboratory tests: Complete blood count, coagulation profile, electrolytes, liver & renal function, tumor markers (if indicated), pregnancy test for women of childbearing age.
-
Imaging studies: This typically includes ultrasound, CT scan, MRI or PET/CT depending on the suspected pathology. These help define whether a laparoscopy is indicated and guide surgical planning.
-
Assessment of anesthesia risk and pre-operative optimization (cardiac, respiratory, diabetic control).
-
Patient counselling: Discussion of risks/benefits, alternatives (observation, more imaging, open surgery), possibility of therapeutic intervention during the same procedure, possibility of conversion to laparotomy.
B. Intra-Operative Diagnostic Process
During the laparoscopic procedure itself:
-
The abdomen is insufflated with CO₂ to create working space ("pneumoperitoneum"), a laparoscope is inserted (typically via an incision near the umbilicus), and additional small ports may be created. The surgeon systematically inspects all quadrants of the abdomen and pelvis, including surfaces of major organs, peritoneum, and potential pathology areas (adhesions, masses, fluid, inflammation).
-
The surgeon may obtain biopsies or cytologic washings, may take peritoneal fluid samples, may inspect organ surfaces, may evaluate adhesions, may detect small lesions not visible on imaging.
-
Based on findings, the surgeon forms a diagnosis and may even convert to operative intervention (i.e., if appendicitis, cholecystitis or other treatable process is found).
The direct visual inspection plus ability to biopsy makes diagnostic laparoscopy highly valuable when imaging is inconclusive.
Treatment Options of Diagnostic Laparoscopy
While the primary role of diagnostic laparoscopy is diagnosis, it increasingly serves dual purposes: diagnosis plus treatment (hybrid diagnostic-therapeutic laparoscopy). This section describes the procedural options and what follows.
A. Procedural Options
-
Pure Diagnostic Laparoscopy: The surgeon enters the abdomen with the sole goal of visual inspection and biopsy. No therapeutic step is planned initially, though the surgeon is prepared for possible intervention.
-
Combined Diagnostic & Therapeutic Laparoscopy: Many surgeons plan for treatment if pathology is found: for example, if a suspicious mass is found, the surgeon may proceed to removal; if adhesions causing pain are discovered, lysis may be done; if endometriosis is found, ablation may be done; in fertility evaluation, tubal repair may be considered.
-
Staging Laparoscopy: In oncology, diagnostic laparoscopy is used to determine the extent of cancer spread (e.g., peritoneal metastases) so the treatment plan (surgery vs chemotherapy) can be made appropriately.
-
Bedside or ICU Laparoscopy: In critically ill patients, laparoscopy may be performed at bedside to detect intra-abdominal sepsis, ischemic bowel or other hidden pathology.
B. Post-Procedure Follow-Up and Management
-
Based on operative findings, the patient's management plan may change: e.g., initiation of chemotherapy for cancer, initiation of fertility treatment, surgical therapy for identified disease.
-
The postoperative period typically involves monitoring for complications (see next section), plus scheduled follow-up visits where results of biopsy or washings are reviewed and further treatment options are decided.
-
Rehabilitation or supportive care may be required depending on findings (e.g., if therapeutic intervention was done).
-
Patient education about wound care, activity restrictions (often minimal due to small incisions), signs to watch for.
Prevention and Management of Diagnostic Laparoscopy
Prevention and management of complications in diagnostic laparoscopy rely on preoperative preparation, meticulous surgical technique, strict infection control, and postoperative care. Most serious risks are rare but can be minimized with experienced teams and careful attention at every stage.
A. Prevention (Of Complications and Need for More Invasive Surgery)
While you cannot always "prevent" the need for diagnostic laparoscopy when pathology is suspected, you can optimize the conditions by:
-
Early diagnosis of abdominal/pelvic symptoms via non-invasive imaging and labs to avoid delays.
-
Use of high-quality imaging, ultrasound and cross-sectional scans to guide whether laparoscopy is needed.
-
Preoperative optimization of the patient: managing comorbidities, nutrition, cessation of smoking, controlling infections.
-
Proper patient selection: patients with massive prior surgeries, dense adhesions or unstable hemodynamics may not be ideal candidates for laparoscopy; open approach or alternative imaging may be better.
B. Management After the Procedure
-
Postoperative wound and incisions: keeping them clean, dry, monitoring for infection.
-
Monitoring for signs of internal complications: bleeding, organ injury, infection, gas complications.
-
Pain management: although laparoscopy is less painful than open surgery, some discomfort, gas-related shoulder pain or bladder urge may occur.
-
Early ambulation: helps recovery, reduces risks of deep vein thrombosis, gas retention.
-
Communication of pathology results to patient and planning next steps (therapeutic interventions, surveillance).
-
Lifestyle recommendations: depending on underlying diagnosis, patient may need to modify diet (if GI pathology found), follow up with oncology/gynecology, avoid certain activities temporarily, cease smoking/alcohol.
Complications of Diagnostic Laparoscopy
While diagnostic laparoscopy is considered safe, the possibility of complications remains. Some of the important complications include:
-
Trocar or port-site injury: When inserting the trocar or laparoscope, there is risk of injuring bowel, bladder, blood vessels or other organs.
-
Bleeding or hemorrhage: If an intra-abdominal vessel is injured or a lesion is biopsied and bleeds.
-
Infection: At the incision site, deeper intra-abdominal infection, peritonitis if bowel injury occurs.
-
Gas-related complications: The carbon dioxide used to inflate the abdomen can cause shoulder pain (irritation of diaphragm), subcutaneous emphysema, or cardiac/respiratory changes in vulnerable patients.
-
Conversion to open surgery: Sometimes the visualization is inadequate, adhesions too dense or findings too complex requiring full laparotomy.
-
Anesthesia-related risks: Especially in patients with cardiopulmonary disease.
-
Delayed diagnosis or missed pathology: Some retroperitoneal or deeply embedded lesions may be missed by laparoscopy, which may give false reassurance.
-
Adhesion formation: Although smaller than open surgery, laparoscopy can still lead to adhesions which have long-term implications (especially for fertility or bowel obstruction).
Adequate surgical team expertise, patient selection and postoperative monitoring help minimise these risks.
Living with the Condition of Diagnostic Laparoscopy
Although diagnostic laparoscopy is a procedure rather than a chronic "condition", patients and their caregivers benefit from understanding life before, during and after the procedure — and what to expect in longer-term follow-up.
A. Pre-Procedure Considerations
-
Patients should be informed about what the procedure will involve, including small incisions, possible gas discomfort, requirement of general or regional anesthesia, potential therapeutic intervention.
-
Patient should prepare their body: fasting before surgery, stopping certain medications (anticoagulants), informing physician of prior surgeries, allergies, comorbidities.
-
Psychological preparation: anxiety around surgical diagnosis, possibility of discovering serious pathology, need for biopsy results, further treatment.
B. Recovery and Short-Term Life
-
After laparoscopy, most patients recover relatively quickly compared to open surgery: small incisions heal faster, hospital stay is shorter, return to normal activities is faster.
-
Some discomfort, bloating or shoulder pain from the pneumoperitoneum is common and usually temporary.
-
The incision sites must be cared for: keeping them clean, dry, avoiding heavy lifting as per surgeon's instructions.
-
Patients must attend post-operative follow-up, review of biopsy/pathology results and planning of next steps (therapeutic surgery, oncology treatments, fertility etc).
C. Long-Term Outlook
-
The long-term outlook depends entirely on what was found during the laparoscopy and what subsequent treatment is required. For example:
-
If benign disease (endometriosis, adhesions) is found and treated, the patient may resume normal life with improved symptoms.
-
If malignancy is discovered, the patient enters a different phase of care (treatment, follow-up).
-
If no abnormality is found, the laparoscopy still offers value by ruling out serious pathology and preventing more invasive open surgery.
-
-
Patients should maintain a healthy lifestyle (balanced diet, exercise, avoiding smoking/alcohol), especially if abdominal or pelvic pathology is present.
-
If repeat laparoscopy or further surgery is indicated, prior patient experience helps adapt and set expectations for recovery.
D. Patient Education and Support
-
Inform patients that even though laparoscopy is less invasive, it is still surgery — some downtime is required, and they must observe surgeon's instructions.
-
Provide support for dealing with anxiety around findings, biopsies, results, follow-up treatments.
-
Encourage patients to monitor for and report any new symptoms promptly: increased pain, fever, bleeding, change in bowel/bladder habits, persistent bloating.
-
For patients with fertility concerns, gynecologic findings, or cancer staging, appropriate counselling and referral to support groups or fertility/oncology specialists may be needed.
Top 10 Frequently Asked Questions about Diagnostic Laparoscopy
1. What is Diagnostic Laparoscopy and How Does it Work?
Diagnostic laparoscopy is a minimally invasive surgical procedure that allows doctors to directly examine the organs inside the abdomen and pelvis. It uses a laparoscope, a thin tube equipped with a camera and light, inserted through small incisions in the abdominal wall. The camera transmits live images to a monitor, enabling the surgeon to identify abnormalities that might not be visible on imaging tests like CT scans or ultrasounds.
This procedure provides a more accurate assessment of conditions such as adhesions, endometriosis, pelvic inflammatory disease, ovarian cysts, and unexplained abdominal pain. Unlike traditional open surgery, laparoscopy requires smaller incisions, resulting in less pain, quicker recovery, and reduced risk of infection.
2. Why Is Diagnostic Laparoscopy Performed?
Diagnostic laparoscopy is indicated when patients have persistent or unexplained abdominal or pelvic symptoms. Common reasons include:
-
Unexplained abdominal or pelvic pain
-
Infertility evaluation: To detect blockages in the fallopian tubes or other reproductive organ abnormalities
-
Suspected endometriosis or pelvic adhesions
-
Evaluation of ovarian cysts, tumors, or masses
-
Appendicitis or gastrointestinal disorders
-
Chronic pelvic inflammatory disease (PID)
-
Internal bleeding or trauma
The primary goal is to diagnose the cause of symptoms accurately and, in many cases, treat minor abnormalities immediately.
3. How Is the Procedure Performed? Step by Step
-
Preoperative Preparation: Patients typically fast for 6–8 hours. Blood tests and imaging may be done prior.
-
Anesthesia: General anesthesia ensures the patient is asleep and pain-free.
-
Incision and Gas Insufflation: A small incision is made near the navel, and carbon dioxide gas is introduced to inflate the abdomen. This creates space for better visualization and maneuvering of instruments.
-
Insertion of Laparoscope: The laparoscope is inserted through the incision, and additional small incisions may be made for surgical instruments.
-
Examination and Possible Treatment: The surgeon examines organs such as the uterus, ovaries, fallopian tubes, appendix, and intestines. Biopsies or minor procedures like cyst removal can be performed simultaneously.
-
Closure: Incisions are closed with sutures or surgical glue, and dressings are applied.
The procedure generally takes 30 minutes to 1 hour, but may be longer if therapeutic interventions are required.
4. Is Diagnostic Laparoscopy Painful?
During the procedure, patients are under anesthesia and feel no pain. Postoperatively, mild discomfort is common, including:
-
Abdominal cramping or bloating due to gas used during the procedure
-
Shoulder pain from diaphragmatic irritation
-
Mild soreness at the incision sites
Pain is usually manageable with over-the-counter or prescribed analgesics, and discomfort typically resolves within a few days.
5. How Should Patients Prepare for the Procedure?
Proper preparation ensures a safe and successful procedure:
-
Fasting: No food or drink for 6–8 hours before surgery
-
Medication Review: Some medications, particularly blood thinners, may need to be paused
-
Medical History: Inform the surgeon about previous surgeries, allergies, or medical conditions
-
Consent and Education: Understand the procedure, risks, recovery timeline, and potential outcomes
-
Transportation: Arrange for someone to drive you home post-procedure, as anesthesia may cause temporary grogginess
6. What Are the Risks and Complications?
Although diagnostic laparoscopy is minimally invasive, potential risks include:
-
Infection at the incision site
-
Bleeding or hematoma formation
-
Organ or blood vessel injury, particularly to the intestines, bladder, or blood vessels
-
Adverse reactions to anesthesia
-
Blood clots or deep vein thrombosis (DVT)
-
Post-operative hernias at the incision site
Choosing an experienced surgeon and accredited facility minimizes these risks.
7. What Is the Recovery Process Like?
Recovery is generally faster than traditional surgery:
-
Hospital Stay: Usually outpatient; some patients stay overnight for observation
-
Initial Recovery: Mild pain, soreness, and bloating are common
-
Activity: Light activities can resume within 1–2 days; avoid heavy lifting for 1–2 weeks
-
Follow-Up: Check-ups ensure proper healing and review any biopsy results
Full recovery and normalization of activities usually occur within 1–2 weeks, depending on the complexity of the procedure.
8. Will Tissue Samples Be Taken?
Yes, diagnostic laparoscopy often allows for biopsies of abnormal tissue, such as:
-
Endometrial or ovarian tissue for infertility evaluation
-
Suspicious masses or cysts
-
Areas affected by infection or inflammation
These samples are sent to a lab for pathological examination, helping guide further treatment.
9. Can Diagnostic Laparoscopy Be Used to Treat Conditions?
Yes, in many cases, laparoscopy is both diagnostic and therapeutic:
-
Adhesion removal to relieve pain or improve fertility
-
Ovarian cyst removal
-
Appendectomy if appendicitis is confirmed
-
Endometriosis excision
-
Minor repairs to organs or tissues
Combining diagnosis and treatment reduces the need for additional invasive surgeries.
10. How Accurate and Reliable Is Diagnostic Laparoscopy?
Diagnostic laparoscopy is highly accurate because it allows direct visualization of the internal organs. It is particularly superior for detecting:
-
Small adhesions or scar tissue
-
Early-stage endometriosis
-
Subtle ovarian or pelvic abnormalities
Its accuracy depends on the surgeon's experience, thorough examination, and proper use of laparoscopic tools. Studies show laparoscopy can diagnose conditions missed by imaging in a significant number of cases.


