Introduction to Double Outlet Right Ventricle Repair
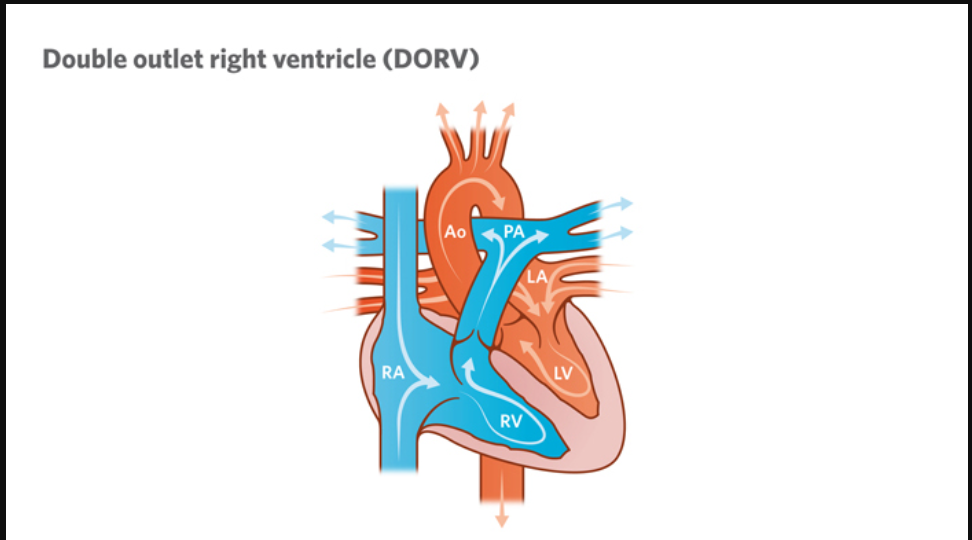
Double Outlet Right Ventricle (DORV) is a rare but serious congenital heart defect in which both of the heart's major arteries - the aorta and the pulmonary artery - arise predominantly or entirely from the right ventricle, instead of one from each ventricle as in a normal heart. In a healthy heart, the aorta carries oxygen-rich blood from the left ventricle to the body, while the pulmonary artery carries oxygen-poor blood from the right ventricle to the lungs. In DORV, this normal separation is disrupted, resulting in mixing of oxygenated and deoxygenated blood, which causes the body to receive insufficient oxygen.
DORV is a complex congenital cardiac anomaly, often associated with other structural heart defects such as ventricular septal defect (VSD), pulmonary stenosis, transposition of the great arteries (TGA), and coarctation of the aorta. The severity of symptoms and type of surgical repair required depend on how these abnormalities are arranged within the heart.
Double Outlet Right Ventricle Repair is a life-saving surgical procedure designed to restore normal blood flow by redirecting oxygen-rich blood from the left ventricle into the aorta, ensuring adequate oxygen delivery to the body. The surgery can vary greatly depending on the specific type of DORV, ranging from intraventricular tunnel repair (baffle repair) to arterial switch operations or single-ventricle palliation in complex cases.
With advancements in pediatric cardiac surgery, neonatal intensive care, and imaging technologies, survival rates for DORV have improved significantly. Early diagnosis, timely surgical intervention, and lifelong follow-up care allow many children born with DORV to lead active, fulfilling lives into adulthood.
Causes and Risk Factors of Double Outlet Right Ventricle Repair
DORV is a congenital condition, meaning it develops during early fetal growth - typically between the 4th and 8th week of pregnancy when the baby's heart is forming. The exact cause is not always known, but a combination of genetic, environmental, and developmental factors is believed to contribute.
A. Causes of Double Outlet Right Ventricle
-
Genetic Factors:
Mutations or chromosomal abnormalities may disrupt normal heart development. Conditions such as 22q11 deletion syndrome, trisomy 13 or 18, or other genetic syndromes are sometimes linked to DORV. -
Abnormal Heart Tube Development:
During fetal growth, improper alignment or rotation of the conotruncal outflow tract results in both arteries connecting to the right ventricle instead of each ventricle having its own artery. -
Environmental and Maternal Factors:
Maternal illnesses like diabetes, viral infections (e.g., rubella), exposure to alcohol, tobacco, or certain medications during pregnancy may increase risk. -
Unknown or Multifactorial Causes:
In most cases, the defect occurs spontaneously without identifiable cause, resulting from complex interactions between genes and environmental factors.
B. Risk Factors Affecting DORV and Its Repair
-
Family history of congenital heart defects.
-
Maternal diabetes or poor prenatal nutrition.
-
Exposure to teratogenic substances (certain medications, alcohol, or toxins).
-
Presence of other heart anomalies, such as pulmonary stenosis or transposition of the great arteries, which make surgical repair more complex.
-
Delayed diagnosis or inadequate management, leading to development of pulmonary hypertension.
-
Low birth weight or premature birth, which complicates surgery and recovery.
These risk factors not only influence the likelihood of developing DORV, but also play a significant role in determining the timing, type, and risk of surgical repair.
Symptoms and Signs of Double Outlet Right Ventricle
Because DORV causes the mixing of oxygen-rich and oxygen-poor blood, the most prominent symptom is cyanosis-a bluish discoloration of the skin, lips, and nails due to low oxygen levels. The severity of symptoms depends on the anatomy of the defect and how well the blood is circulating between the lungs and the body.
Common Symptoms
-
Cyanosis (bluish skin or lips) appearing soon after birth.
-
Rapid or labored breathing (tachypnea).
-
Difficulty feeding or poor weight gain in infants.
-
Excessive sweating during feeding or crying.
-
Fatigue, lethargy, or fainting spells.
-
Clubbing of fingers and toes in older children.
-
Heart murmur, often heard during routine check-ups.
-
Recurrent respiratory infections due to poor oxygenation.
Signs on Clinical Examination
-
Enlarged heart (cardiomegaly).
-
Abnormal heart sounds or murmurs due to turbulent blood flow.
-
Low oxygen saturation levels (hypoxemia).
-
Signs of heart failure such as swelling in the legs or abdomen in severe cases.
Without surgical intervention, most infants with DORV develop severe complications such as pulmonary hypertension, congestive heart failure, or even death in early childhood.
Diagnosis of Double Outlet Right Ventricle
Accurate diagnosis and detailed anatomical assessment are vital to determine the appropriate surgical approach.
A. Prenatal Diagnosis
DORV can often be detected during pregnancy through fetal echocardiography, typically performed around 18-22 weeks gestation. Early diagnosis allows parents and medical teams to plan specialized care and immediate intervention after birth.
B. Postnatal Diagnostic Tests
-
Echocardiography:
The gold-standard diagnostic tool that provides detailed imaging of cardiac chambers, great arteries, and associated defects like VSD or pulmonary stenosis. -
Chest X-Ray:
Shows heart size and pulmonary blood flow patterns. -
Electrocardiogram (ECG):
Helps detect heart enlargement or rhythm abnormalities. -
Cardiac MRI and CT Scan:
Offer 3D visualization of heart anatomy, allowing surgeons to map out repair strategies. -
Cardiac Catheterization:
Measures pressure gradients, oxygen saturation, and confirms findings before surgery.
A multidisciplinary team-including pediatric cardiologists, cardiothoracic surgeons, and radiologists-works together to determine the best surgical plan based on diagnostic results.
Treatment Options for Double Outlet Right Ventricle Repair
Treatment options for double outlet right ventricle (DORV) repair focus on individualized, anatomy-driven surgical correction, with the aim of optimizing oxygen delivery, minimizing shunting, and restoring as normal a heart function as possible. The mainstay of treatment is surgery, but the exact operation depends on each patient's unique heart structure.
A. Medical Stabilization
Before surgery, newborns may require medications to stabilize heart function and improve oxygen delivery:
-
Prostaglandin E1 infusion to keep the ductus arteriosus open and maintain circulation.
-
Diuretics and inotropes to manage heart failure symptoms.
-
Oxygen therapy or mechanical ventilation in critically ill infants.
However, medical therapy only serves as a bridge to surgery - definitive repair is always surgical.
B. Surgical Approaches
The type of Double Outlet Right Ventricle Repair depends on the anatomical relationship of the great arteries, presence of VSD, and pulmonary blood flow.
-
Intraventricular Tunnel (Baffle) Repair:
A patch (baffle) is placed inside the heart to connect the left ventricle to the aorta via the VSD, ensuring oxygen-rich blood is directed correctly. -
Arterial Switch Operation:
Used in cases resembling Taussig-Bing anomaly, where the aorta lies anterior and to the right of the pulmonary artery. The great arteries are repositioned to their correct ventricles. -
Right Ventricular Outflow Tract Reconstruction:
If pulmonary stenosis exists, the narrowed outflow tract is widened using patches or conduits. -
Single-Ventricle or Fontan Repair:
In complex cases where the left ventricle is too small or poorly aligned, a Fontan pathway may be created to redirect blood flow from the body to the lungs without passing through the heart. -
Hybrid or Staged Repairs:
Some children require multiple operations over several years to achieve complete correction.
Surgery is usually performed in infancy, ideally within the first year of life, to prevent irreversible lung damage and ensure normal growth and oxygen delivery.
Prevention and Management of Double Outlet Right Ventricle
While DORV cannot always be prevented, certain steps can reduce risk and improve management outcomes.
A. Prevention
-
Regular prenatal care with fetal ultrasounds and genetic testing when indicated.
-
Avoiding alcohol, tobacco, and harmful drugs during pregnancy.
-
Managing maternal health conditions such as diabetes and infections.
-
Genetic counseling for families with a history of congenital heart defects.
B. Postoperative Management
-
Close monitoring in pediatric intensive care after surgery for cardiac rhythm, oxygen levels, and bleeding.
-
Long-term cardiology follow-up to detect arrhythmias, baffle leaks, or valve problems early.
-
Medications such as anticoagulants, beta-blockers, or ACE inhibitors may be prescribed as needed.
-
Nutritional support and physical therapy to ensure proper growth and development.
-
Endocarditis prophylaxis before dental or surgical procedures to prevent infection.
Complications of Double Outlet Right Ventricle Repair
Although survival rates have improved, DORV repair remains a major cardiac surgery with potential complications.
A. Short-Term (Postoperative) Complications
-
Bleeding and infection at surgical sites.
-
Arrhythmias (irregular heartbeat) requiring temporary pacing.
-
Residual shunts or leaks around the VSD patch.
-
Pulmonary artery stenosis or obstruction after repair.
-
Low cardiac output requiring inotropic support.
-
Neurological complications such as seizures due to low oxygen.
B. Long-Term Complications
-
Right ventricular dysfunction or dilation.
-
Conduit or baffle obstruction, requiring reoperation.
-
Valve regurgitation or stenosis.
-
Exercise intolerance or chronic fatigue.
-
Risk of endocarditis (heart infection).
-
Need for re-intervention during adolescence or adulthood due to growth changes.
With consistent follow-up and lifestyle management, most complications can be prevented or treated early.
Living After Double Outlet Right Ventricle Repair
People living after double outlet right ventricle (DORV) repair can often expect a good quality of life and near-normal potential lifespan, especially after biventricular or more complete repairs. Ongoing follow-up and careful management remain critical due to the possibility of late complications and the need for re-interventions in some cases.
A. Recovery and Growth
After surgery, children typically spend a few days to weeks in the hospital. Full recovery may take several months, during which parents should watch for signs of infection, poor appetite, or difficulty breathing. Nutrition, medication adherence, and gentle activity play key roles in recovery.
B. Long-Term Care
Patients require lifelong cardiology follow-up to monitor heart function. Regular echocardiograms, ECGs, and MRI scans help detect issues early. Children can attend school, play, and grow normally, although some may have mild exercise restrictions.
C. Lifestyle Adjustments
-
Balanced diet rich in protein and vitamins to support cardiac recovery.
-
Regular but moderate exercise, approved by the cardiologist.
-
Avoiding smoking and alcohol in adulthood.
-
Vaccinations and good dental hygiene to prevent infections.
D. Emotional and Social Well-Being
Children and adults with repaired DORV may experience anxiety about their health. Counseling, support groups, and awareness about congenital heart disease help them cope emotionally and socially. With proper care, most individuals lead long, productive lives and can even safely bear children under medical supervision.
Top 10 Frequently Asked Questions about Double Outlet Right Ventricle (DORV) Repair
1. What is Double Outlet Right Ventricle (DORV)?
Double Outlet Right Ventricle (DORV) is a congenital heart defect where both the aorta and pulmonary artery arise from the right ventricle instead of their normal positions. This abnormality causes mixing of oxygen-rich and oxygen-poor blood, leading to reduced oxygen delivery to the body.
2. What are the symptoms of DORV in children?
Symptoms can vary depending on the type and severity of the defect, but commonly include:
-
Cyanosis (bluish skin or lips)
-
Rapid breathing or shortness of breath
-
Fatigue or difficulty feeding
-
Heart murmur detected by a doctor
-
Failure to thrive in infants
Early detection is crucial for timely management and repair.
3. How is DORV diagnosed?
Diagnosis typically involves a combination of:
-
Physical examination and heart auscultation
-
Echocardiogram (ultrasound of the heart)
-
Electrocardiogram (ECG) to assess heart rhythm
-
Chest X-ray to evaluate heart size and blood flow
-
Cardiac MRI or CT scan for detailed anatomical assessment
-
Cardiac catheterization in some cases to measure pressures and oxygen levels
4. What is DORV repair surgery?
DORV repair is open-heart surgery performed to correct the abnormal blood flow. The goal is to direct oxygen-rich blood from the left ventricle to the aorta and oxygen-poor blood to the pulmonary artery.
Techniques may include:
-
Ventricular septal defect (VSD) patching to route blood properly
-
Arterial switch or conduit placement depending on anatomy
-
Valve repair or reconstruction if needed
The surgery is usually performed in infancy or early childhood, though some cases are repaired later depending on severity.
5. How is the surgery performed?
-
General anesthesia is administered.
-
The chest is opened through a median sternotomy.
-
The patient is placed on a heart-lung bypass machine to maintain circulation while the heart is repaired.
-
The surgeon reroutes blood flow and repairs the heart using patches or conduits.
-
The heart is restarted, and the chest is closed.
The procedure typically lasts 4-6 hours, depending on complexity.
6. What are the risks and complications of DORV repair?
Like all heart surgeries, DORV repair carries risks:
-
Bleeding or infection
-
Arrhythmias (abnormal heart rhythms)
-
Residual or recurrent heart defects
-
Heart failure or low cardiac output
-
Stroke or neurological complications (rare)
-
Death (rare, especially in complex cases)
Risk is minimized by experienced pediatric cardiac surgeons and specialized centers.
7. What is the recovery process after DORV repair?
-
Hospital stay: Usually 7-14 days, depending on recovery
-
ICU care: First few days for monitoring heart function, breathing, and blood pressure
-
Medications: To support heart function, prevent blood clots, or control rhythm
-
Activity: Gradual increase; children may resume normal activities over weeks to months
-
Follow-up: Regular cardiology visits with echocardiograms and ECGs to monitor heart function
Full recovery may take 1-3 months, with long-term monitoring essential.
8. Will my child need additional surgeries later?
Some children may require additional interventions if:
-
There is residual obstruction or leakage
-
Conduits or patches need replacement as the child grows
-
Heart rhythm abnormalities develop
Most patients, however, achieve significant improvement in heart function and quality of life after the initial repair.
9. What is the long-term outlook after DORV repair?
-
Most children lead active, healthy lives with proper follow-up care.
-
Long-term outcomes depend on the type of DORV, associated defects, and timing of surgery.
-
Lifelong cardiology follow-up is recommended to monitor heart function, valves, and rhythm.
-
Exercise and activity are encouraged, with guidance from the cardiologist.
10. How can parents prepare for DORV repair surgery?
-
Understand the procedure: Discuss surgical plan, risks, and expected outcomes with the cardiac team
-
Preoperative evaluation: Ensure all blood tests, imaging, and pre-surgical assessments are complete
-
Arrange support at home: Recovery requires rest and gradual activity progression
-
Emotional preparation: Counseling and support groups can help parents and siblings cope with surgery stress
Parents play a critical role in post-operative care, monitoring symptoms, and ensuring follow-up visits.


