Introduction to Double Switch Operation
The Double Switch Operation (DSO) is an advanced and intricate corrective heart surgery performed primarily for congenital heart defects where the normal connections of the heart's chambers and great arteries are reversed. The most common indication is Congenitally Corrected Transposition of the Great Arteries (CCTGA), a rare condition in which the heart's electrical and mechanical systems are abnormally aligned - the ventricles and the arteries are "switched" in their positions.
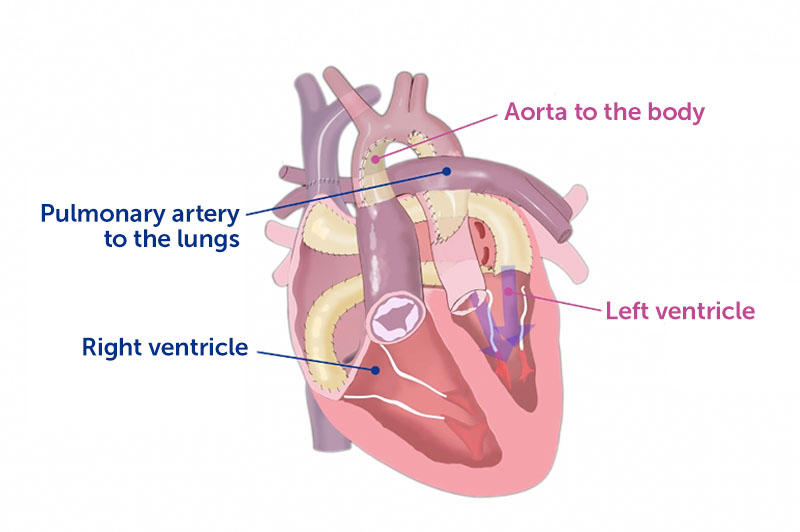
In a healthy heart, the right ventricle pumps deoxygenated blood into the pulmonary artery (to the lungs), and the left ventricle pumps oxygenated blood into the aorta (to the body). In CCTGA, this relationship is reversed - the right ventricle ends up pumping to the body while the left ventricle pumps to the lungs. Although blood flow may initially seem normal because the circuits are "double switched," the right ventricle is not built to handle high systemic pressure long-term, leading to heart failure, valve leakage, and rhythm disturbances as the patient grows older.
The Double Switch Operation aims to restore the heart's anatomy and physiology as close to normal as possible. It involves two simultaneous "switches":
-
Atrial switch (Senning or Mustard procedure): Redirects the blood flow at the atrial level so that oxygen-rich and oxygen-poor blood go to the correct ventricles.
-
Arterial switch (Jatene procedure): Reconnects the great arteries to their correct ventricles, ensuring the left ventricle pumps blood to the aorta and the right ventricle to the pulmonary artery.
By performing both switches, surgeons effectively "correct" the heart's structure and function, giving the patient a physiologically normal circulation. Modern advancements in pediatric cardiac surgery, anesthesia, imaging, and postoperative care have made the Double Switch Operation a life-saving and long-term restorative surgery, improving both survival and quality of life.
Causes and Risk Factors of Double Switch Operation
The Double Switch Operation is a treatment, not a cause of disease itself, but understanding why the surgery is needed begins with understanding the underlying congenital heart defects.
A. Causes Leading to the Need for a Double Switch Operation
-
Congenitally Corrected Transposition of the Great Arteries (CCTGA):
The most common reason for this surgery. In CCTGA, the heart's ventricles and arteries are inverted - the right ventricle pumps to the body, and the left ventricle pumps to the lungs. Over time, this abnormal setup strains the right ventricle, causing failure. -
Dextro-Transposition of the Great Arteries (d-TGA) with Ventricular Septal Defect or Pulmonary Stenosis:
In certain complex cases, a double switch is required to restore both ventricular and arterial alignment. -
Other Complex Congenital Heart Defects:
Rarely, patients with multiple misalignments of the great vessels or ventricles require this dual correction to re-establish normal physiology.
B. Risk Factors
-
Genetic and Chromosomal Abnormalities: Some cases are linked to defects like 22q11 deletion syndrome, heterotaxy, or situs inversus (abnormal organ positioning).
-
Maternal Health Conditions: Poorly controlled diabetes, viral infections during pregnancy (rubella, cytomegalovirus), or exposure to teratogenic drugs increase the risk of congenital heart malformations.
-
Family History: Congenital heart defects can be hereditary, particularly in families with cardiac abnormalities.
-
Environmental Factors: Smoking, alcohol, radiation exposure, and poor prenatal care can contribute to fetal heart development issues.
Because this defect forms during fetal life, prevention centers on maternal health, early prenatal detection, and genetic counseling, rather than avoidance after birth.
Symptoms and Signs of Double Switch Operation (Underlying Conditions)
Children who require a Double Switch Operation usually show symptoms of CCTGA or TGA, which may vary depending on the severity of associated structural problems.
A. Common Symptoms
-
Cyanosis: Bluish discoloration of lips, skin, or nails due to low oxygen levels.
-
Shortness of Breath: Difficulty breathing during feeding or exertion.
-
Fatigue and Poor Growth: Infants may tire easily and struggle to gain weight.
-
Palpitations or Irregular Heartbeats: Resulting from conduction abnormalities in the inverted ventricles.
-
Swelling (Edema): In the legs or abdomen due to heart failure.
-
Exercise Intolerance: Older children may struggle to play or keep up with peers.
B. Physical Signs
-
Heart murmur due to turbulent blood flow.
-
Enlarged liver and neck vein distension in advanced heart failure.
-
Clubbing of fingers in chronic cyanosis cases.
-
Signs of right ventricular hypertrophy (RV thickening) and tricuspid valve regurgitation.
Symptoms often worsen with age, as the right ventricle deteriorates under systemic workload. The timing of surgical correction is therefore critical to prevent irreversible heart damage.
Diagnosis of Double Switch Operation Candidates
A. Prenatal Diagnosis
Modern fetal echocardiography can detect CCTGA or TGA as early as 18-22 weeks of gestation, allowing parents and doctors to plan early management and delivery at specialized cardiac centers.
B. Postnatal and Pediatric Diagnostic Procedures
-
Echocardiography (2D/3D):
The primary tool for assessing chamber orientation, valve connections, and great artery relationships. -
Electrocardiogram (ECG):
Reveals conduction abnormalities such as complete heart block or arrhythmias common in CCTGA. -
Chest X-Ray:
Shows cardiac enlargement and abnormal positioning of great arteries. -
Cardiac MRI/CT Angiography:
Provides a three-dimensional map of cardiac structures, arteries, and veins - essential for surgical planning. -
Cardiac Catheterization:
Measures pressure gradients and oxygen levels in different heart chambers and confirms suitability for double switch repair.
Precise anatomical mapping is vital, as each patient's heart has unique variations requiring individualized surgical planning.
Treatment Options for Double Switch Operation
A. Pre-Surgical Medical Management
Before surgery, stabilization is critical.
-
Diuretics, ACE inhibitors, or digoxin may be prescribed to control heart failure.
-
Pacemaker implantation may be required if significant conduction blocks exist.
-
Oxygen therapy and nutritional support ensure optimal condition before surgery.
B. The Double Switch Operation - Step-by-Step Overview
The surgery combines two major procedures: the atrial switch and the arterial switch.
-
Atrial Switch (Senning or Mustard procedure):
The surgeon constructs a baffle (internal tunnel) within the atria to redirect venous blood flow:-
Deoxygenated blood from the body is directed to the left ventricle.
-
Oxygenated blood from the lungs is redirected to the right ventricle.
-
-
Arterial Switch (Jatene procedure):
The great arteries are detached and reconnected to their appropriate ventricles:-
The aorta is connected to the left ventricle.
-
The pulmonary artery is connected to the right ventricle.
-
The coronary arteries are re-implanted into the new aorta.
-
-
Additional Repairs (if required):
-
Closure of VSD or repair of pulmonary stenosis.
-
Tricuspid valve repair if regurgitation exists.
-
Pacemaker placement for conduction abnormalities.
-
C. Duration and Recovery
The operation typically takes 6-10 hours under cardiopulmonary
bypass.
Patients usually spend 5-10 days in the intensive care unit
(ICU) for monitoring, followed by several weeks of recovery in the
hospital.
Prevention and Postoperative Management
A. Prevention
Because DSO addresses a congenital anomaly, prevention focuses on maternal and fetal health:
-
Proper prenatal care and genetic screening.
-
Avoidance of harmful substances (alcohol, tobacco, drugs).
-
Control of chronic maternal diseases.
-
Early fetal echocardiographic evaluation for high-risk pregnancies.
B. Postoperative Management
-
Continuous cardiac monitoring for arrhythmias or conduction issues.
-
Medications to support cardiac function and prevent clot formation.
-
Regular echocardiograms to assess ventricular performance.
-
Gradual physiotherapy and nutrition optimization for recovery.
-
Endocarditis prophylaxis for dental or invasive procedures.
-
Ongoing pacemaker follow-up if implanted.
Patients often require lifelong cardiology supervision by adult congenital heart disease specialists.
Complications of Double Switch Operation
A. Early (Post-Surgical) Complications
-
Bleeding and infection.
-
Arrhythmias, particularly atrial flutter or heart block.
-
Coronary artery kinking or obstruction after reimplantation.
-
Low cardiac output syndrome requiring temporary mechanical support.
-
Pulmonary or systemic venous obstruction from atrial baffles.
B. Long-Term Complications
-
Baffle obstruction or leaks requiring reoperation.
-
Valve regurgitation (especially tricuspid or aortic).
-
Coronary artery narrowing leading to ischemia.
-
Right or left ventricular dysfunction over years.
-
Arrhythmias needing permanent pacemaker implantation.
-
Endocarditis (heart infection) risk.
Regular lifelong follow-up, imaging, and prompt treatment of complications have greatly improved survival rates - currently over 85-90% long-term survival at specialized centers.
Living with the Condition After Double Switch Operation
A. Postoperative Life and Recovery
After initial recovery, children often resume near-normal growth and physical activity. Early months may require close monitoring of feeding, oxygen levels, and wound healing. With time, most patients can attend school and live active lives, though some may have restrictions on high-intensity exercise.
B. Long-Term Outlook
With successful repair, the heart functions physiologically normal. Lifelong cardiology follow-up ensures detection of:
-
Valve abnormalities.
-
Baffle or arterial complications.
-
Rhythm disturbances.
-
Ventricular performance issues.
C. Lifestyle and Emotional Health
-
Maintain a balanced diet and healthy weight.
-
Avoid smoking or alcohol in adulthood.
-
Exercise under guidance of a cardiologist.
-
Ensure emotional support and connect with congenital heart support groups.
-
Women with repaired DSO can often have safe pregnancies under specialized care.
Today, thanks to surgical precision and medical progress, most children who undergo a Double Switch Operation grow into healthy, independent adults capable of pursuing careers, relationships, and normal life expectancy.
Top 10 Frequently Asked Questions about Double Switch Operation
1. What is a Double Switch Operation?
A Double Switch Operation is a complex open-heart surgery performed to correct certain congenital heart defects, particularly Congenitally Corrected Transposition of the Great Arteries (CCTGA). In this condition, the positions of the heart's main pumping chambers and great arteries are reversed, leading to improper blood flow. The operation “switches” both the blood flow within the heart (atrial switch) and the arterial connections (arterial switch), restoring normal circulation of oxygen-rich and oxygen-poor blood.
2. Why is a Double Switch Operation needed?
This surgery is necessary when a child has CCTGA or related defects causing the right ventricle (which is weaker) to perform the work of the left ventricle (which pumps blood to the whole body). Over time, this strain can lead to heart failure or valve leakage. The double switch operation corrects this by re-routing blood flow so the left ventricle functions as the main pumping chamber, improving long-term heart function.
3. At what age is the Double Switch Operation performed?
The ideal timing varies depending on the child's condition and ventricular function.
-
In infants or young children, the surgery is often performed between 6 months to 2 years of age.
-
In some cases, doctors may perform preparatory surgeries (such as pulmonary artery banding) before the full double switch to strengthen the left ventricle.
The exact timing is determined after thorough evaluation by a pediatric cardiologist and cardiac surgeon.
4. What conditions can the Double Switch Operation correct?
The procedure is primarily used to correct:
-
Congenitally Corrected Transposition of the Great Arteries (CCTGA)
-
Ventricular Septal Defect (VSD) associated with CCTGA
-
Pulmonary stenosis or atresia
-
Certain forms of complex congenital heart disease involving abnormal blood flow between ventricles and arteries.
5. How is the Double Switch Operation performed?
The surgery combines two major procedures:
-
Atrial Switch (Senning or Mustard procedure) - Redirects blood returning to the heart so that oxygen-poor blood enters the right ventricle and oxygen-rich blood enters the left ventricle.
-
Arterial Switch - Repositions the aorta and pulmonary artery to their correct ventricles.
These combined steps restore the heart's natural pumping direction, ensuring proper oxygen delivery to the body.
6. How long does the surgery take and what happens afterward?
The operation is performed under general anesthesia and typically lasts 6 to 8 hours. After surgery:
-
The child is kept in the Cardiac Intensive Care Unit (CICU) for close monitoring.
-
Breathing tubes, IV lines, and monitors are gradually removed over a few days.
-
Most children remain in the hospital for 10-14 days, depending on recovery.
7. What are the possible risks of a Double Switch Operation?
While modern surgical techniques have made the procedure highly successful, potential risks include:
-
Bleeding or infection
-
Heart rhythm disturbances (arrhythmias)
-
Coronary artery complications
-
Residual leaks or narrowing at surgical connections
-
Heart failure (rare in modern outcomes)
The overall survival and success rates are excellent in experienced cardiac centers.
8. What is the recovery process like after surgery?
Recovery usually takes several weeks. Parents can expect:
-
Gradual improvement in breathing and energy levels
-
Temporary fatigue or poor appetite
-
Regular follow-up visits for echocardiograms and ECGs
-
Restrictions on heavy activity for 6-8 weeks
Full recovery depends on the child's age, heart condition, and overall health.
9. What is the long-term outlook after a Double Switch Operation?
The long-term outlook is very positive. Most children grow up with normal or near-normal heart function and can lead active, healthy lives. Lifelong cardiac follow-up is essential to monitor heart rhythm, valve function, and ventricular performance. Some patients may require minor procedures or medications later in life to support heart health.
10. How can parents care for their child after a Double Switch Operation?
After discharge, parents should:
-
Follow the prescribed medication schedule strictly.
-
Ensure the child eats a nutritious, heart-healthy diet.
-
Attend all follow-up appointments for heart check-ups.
-
Watch for signs such as breathing difficulty, bluish skin, or extreme fatigue, and contact the doctor immediately if they occur.
Regular care and medical monitoring can ensure the best long-term results for your child.


