Introduction to Elbow Replacement
Elbow Replacement Surgery, medically known as Total Elbow Arthroplasty (TEA), is a highly specialized surgical procedure designed to relieve pain, restore motion, and improve function in individuals suffering from severe elbow joint damage. This operation involves replacing the diseased or damaged parts of the elbow joint with artificial components (prostheses) made of metal and medical-grade plastic, mimicking the smooth movement of a healthy elbow.
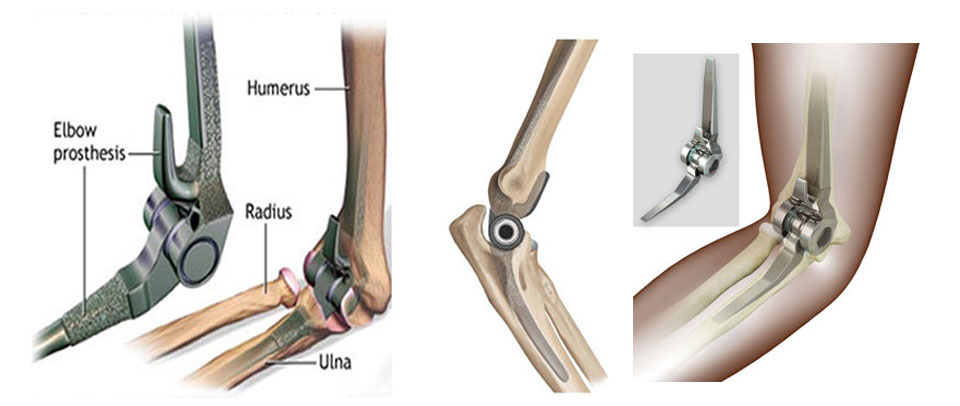
The elbow joint is a complex hinge-type joint connecting the humerus (upper arm bone) with the radius and ulna (forearm bones). It allows bending (flexion-extension) and rotation (pronation-supination) — movements essential for daily tasks such as eating, dressing, or lifting. However, trauma, arthritis, and overuse can lead to irreversible damage, resulting in pain, deformity, and loss of motion.
Elbow replacement surgery aims to recreate normal joint mechanics when conservative treatments like medication, injections, or physiotherapy fail to control symptoms. During the procedure, the surgeon removes the damaged bone and cartilage surfaces and replaces them with metal stems (fitted into the humerus and ulna) connected by a hinged or semi-hinged plastic joint that allows smooth and stable movement.
Although less common than hip or knee replacements, elbow replacement has evolved dramatically over the last two decades. Thanks to advances in implant design, surgical technique, and rehabilitation protocols, it is now considered one of the most effective solutions for restoring pain-free motion and functional strength in patients with advanced joint disease or severe fractures.
By 2025, elbow replacement surgery has become a standard of care for specific cases of osteoarthritis, rheumatoid arthritis, complex fractures, and post-traumatic arthritis — offering not just mobility but a renewed quality of life.
Causes and Risks Leading to Elbow Replacement
Elbow replacement surgery is typically recommended when the joint is irreversibly damaged and other treatments no longer provide relief. The damage can stem from degenerative diseases, autoimmune conditions, or trauma.
A. Major Causes
-
Rheumatoid Arthritis (RA):
The most common indication for elbow replacement. This autoimmune disease causes chronic inflammation of the joint lining (synovium), leading to cartilage destruction, bone erosion, and severe deformity. Arthroplasty restores function and relieves pain in advanced RA. -
Osteoarthritis (Degenerative Arthritis):
With age or overuse, the protective cartilage wears away, leading to stiffness, grinding, and pain. When degeneration becomes advanced, joint replacement offers long-term relief. -
Post-Traumatic Arthritis:
After a serious fracture or dislocation, even with proper healing, the joint may develop abnormal wear patterns, leading to chronic pain and stiffness. Replacement restores alignment and function. -
Severe Fractures (Especially in the Elderly):
Complex fractures involving multiple bone fragments — particularly of the distal humerus — may not be reconstructible with plates and screws. In such cases, immediate replacement provides better outcomes. -
Failed Previous Surgeries:
Patients who have undergone prior fixation, partial replacement, or arthrodesis (joint fusion) and continue to experience pain or stiffness may need total elbow replacement. -
Tumor Resection or Bone Loss:
In cases where cancer or infection has destroyed parts of the elbow joint, replacement reconstructs both function and structure.
B. Risk Factors for Elbow Degeneration
-
Advancing age (especially over 60 years).
-
History of repetitive heavy lifting or occupational strain.
-
Chronic inflammatory conditions like lupus or gout.
-
Poorly healed fractures or repeated dislocations.
-
Smoking and diabetes, which delay tissue healing.
-
Genetic predisposition to arthritis.
Recognizing these risks early and maintaining joint health through physiotherapy and medical management can delay the need for surgical intervention.
Symptoms and Signs Indicating the Need for Elbow Replacement
Elbow degeneration or trauma leads to progressive pain, stiffness, and loss of function. The symptoms often worsen over time and may become unresponsive to non-surgical measures.
A. Common Symptoms
-
Chronic Pain:
Persistent aching or throbbing pain, even at rest, especially during daily activities such as lifting or turning objects. -
Joint Stiffness:
Difficulty bending or straightening the elbow, with restricted motion range. -
Swelling and Warmth:
Inflammatory response leading to tenderness and visible swelling. -
Grinding or Clicking Sensation:
Rough joint surfaces produce noise during movement. -
Loss of Strength:
Weakness when lifting objects or performing tasks requiring grip or rotation. -
Deformity:
Visible joint misalignment or “crooked” elbow appearance. -
Functional Limitation:
Difficulty performing daily activities like eating, grooming, or writing.
B. Clinical Signs
-
Pain on palpation over joint margins.
-
Limited flexion-extension and rotation.
-
Joint crepitus (grating sound).
-
Visible swelling or bony enlargement.
-
Muscle wasting around the arm from disuse.
When these symptoms persist despite medical therapy, elbow replacement surgery may be the only viable solution to restore comfort and function.
Diagnosis and Evaluation Before Elbow Replacement
Accurate diagnosis ensures that elbow replacement is appropriate and safe. The evaluation involves both clinical examination and imaging to assess joint integrity and surrounding soft tissue health.
A. Diagnostic Steps
-
Medical History and Physical Examination:
Assessment of pain duration, movement restrictions, and impact on daily life. The surgeon evaluates deformity, swelling, and muscle strength. -
Imaging Studies:
-
X-rays: Show bone alignment, joint space narrowing, and deformities.
-
CT Scan: Provides a 3D view of bone structure, essential for surgical planning in complex deformities.
-
MRI: Evaluates soft tissues, ligaments, and cartilage health.
-
Bone Scan: May be ordered to rule out infection or necrosis.
-
-
Blood Tests:
Screen for infection (CBC, ESR, CRP) and autoimmune markers (rheumatoid factor, anti-CCP). -
Joint Aspiration:
If infection is suspected, synovial fluid may be analyzed for bacteria or crystals.
B. Preoperative Evaluation
-
General health assessment (cardiac, renal, and pulmonary evaluation).
-
Anesthesia clearance.
-
Review of medications, especially anticoagulants.
-
Counseling on postoperative expectations and rehabilitation.
Treatment Options and the Elbow Replacement Procedure
A. Non-Surgical Options
Before recommending replacement, doctors attempt conservative management:
-
Physical Therapy: Stretching and strengthening exercises.
-
Pain Management: NSAIDs, corticosteroids, or PRP injections.
-
Activity Modification: Avoiding repetitive stress and heavy lifting.
-
Bracing: Supports and stabilizes the joint during motion.
-
Assistive Devices: To reduce joint strain during daily tasks.
If these measures fail to provide relief, surgical intervention becomes necessary.
B. The Elbow Replacement Procedure
Elbow replacement can be total, partial, or linked/unlinked, depending on the extent of damage.
1. Preoperative Preparation
-
The patient is placed under general or regional anesthesia.
-
The arm is sterilized and positioned for optimal surgical access.
2. Surgical Steps
-
Incision and Exposure:
A curved incision is made at the back of the elbow to access the joint. Surrounding muscles and ligaments are carefully retracted. -
Removal of Damaged Bone and Cartilage:
The surgeon removes worn-out bone surfaces from the humerus and ulna. -
Implant Placement:
Metal stems are inserted into both bones and connected by a hinged or semi-hinged joint made of polyethylene and titanium. -
Alignment and Testing:
The new joint is tested for smooth, stable motion before closure. -
Closure:
The incision is sutured, and a sterile dressing is applied.
3. Duration and Hospital Stay
-
Surgery Time: 2-3 hours.
-
Hospital Stay: 2-4 days post-surgery for observation and early physiotherapy.
Prevention and Postoperative Management
A. Preventive Care
Although not all elbow disorders are preventable, these habits maintain joint health:
-
Regular exercise to strengthen arm and shoulder muscles.
-
Avoid repetitive heavy lifting or high-impact activity.
-
Prompt treatment of fractures and dislocations.
-
Control inflammatory diseases like rheumatoid arthritis.
-
Balanced diet rich in calcium and vitamin D.
B. Postoperative Rehabilitation
-
Pain Control:
Managed with medications and cold compresses. -
Immobilization:
A splint is used for the first few days to support healing. -
Physiotherapy:
Gentle motion exercises begin within a week to prevent stiffness. -
Activity Restrictions:
Avoid heavy lifting (more than 5 kg) for life to prevent implant wear. -
Follow-Up:
Regular checkups and X-rays to ensure implant stability.
With strict adherence to rehabilitation, most patients regain 70-90% of normal elbow movement within 3-6 months.
Complications of Elbow Replacement
While modern implants are safe, complications can occasionally occur.
A. Early Complications
-
Infection: Requires antibiotics or revision surgery in severe cases.
-
Nerve Injury: The ulnar nerve is at risk; usually temporary numbness.
-
Bleeding or Hematoma Formation.
-
Wound Healing Issues due to diabetes or smoking.
B. Late Complications
-
Implant Loosening or Wear: Occurs after years of use; may need revision.
-
Joint Instability or Dislocation: Rare but possible if ligaments weaken.
-
Bone Fracture around the Prosthesis: Especially from trauma.
-
Chronic Pain or Stiffness.
-
Allergic Reaction to implant materials (rare).
Overall success rates exceed 90%, with implants lasting 10-15 years or longer in most patients.
Living with the Condition After Elbow Replacement
A. Recovery and Rehabilitation
Patients experience immediate pain relief after surgery, though full recovery takes months. A structured rehabilitation program focuses on:
-
Restoring range of motion.
-
Strengthening surrounding muscles.
-
Gradual return to light activities.
-
Avoiding jerky or high-impact movements.
B. Lifestyle Adjustments
-
Avoid lifting weights heavier than 5 kg.
-
Maintain a healthy weight.
-
Avoid contact sports or manual labor.
-
Continue lifelong physiotherapy to preserve flexibility.
C. Long-Term Outlook
With modern implants and surgical precision, elbow replacement patients enjoy:
-
Substantial pain relief.
-
Improved strength and function.
-
Ability to perform self-care and light work independently.
Most patients resume normal routines — driving, cooking, writing, and even light gardening — within 8-12 weeks.
D. Emotional and Psychological Well-Being
Living pain-free after years of disability often brings renewed confidence and emotional recovery. Counseling and physiotherapy together enhance overall quality of life.
Top 10 Frequently Asked Questions about Elbow Replacement Surgery
1. What is Elbow Replacement Surgery?
Elbow replacement surgery, also known as Total Elbow Arthroplasty, is a procedure in which the damaged parts of the elbow joint are replaced with artificial components (prosthesis). These prosthetic parts mimic the function of a natural joint, helping restore movement, reduce pain, and improve overall arm function.
2. Why is Elbow Replacement Surgery needed?
Doctors recommend elbow replacement surgery when the joint is severely damaged or painful due to:
-
Rheumatoid arthritis or other inflammatory joint diseases
-
Severe fractures that can’t be repaired
-
Post-traumatic arthritis after an old injury
-
Osteoarthritis causing chronic pain and stiffness
-
Failed previous elbow surgeries
It’s usually performed when conservative treatments like medication or physiotherapy no longer provide relief.
3. What are the types of Elbow Replacement?
There are two main types of elbow replacement procedures:
-
Total Elbow Replacement (Linked prosthesis):
Both sides of the joint are replaced and linked together with a hinge mechanism for stability. -
Partial or Unlinked Elbow Replacement:
Only one side of the joint is replaced; relies on surrounding ligaments and muscles for stability.
Your surgeon will choose the type based on the extent of damage, bone quality, and your overall health.
4. How is Elbow Replacement Surgery performed?
The procedure is performed under general or regional anesthesia and
typically takes 1.5-2 hours.
Steps include:
-
Making an incision at the back of the elbow
-
Removing the damaged bone and cartilage
-
Inserting the metal and plastic prosthetic components into the humerus and ulna
-
Attaching and securing them with bone cement or screws
-
Closing the incision and applying a soft dressing or splint
5. What are the benefits of Elbow Replacement Surgery?
The surgery offers multiple benefits, including:
-
Significant pain relief
-
Improved joint movement and flexibility
-
Restored arm strength for daily activities
-
Better quality of life and independence
Most patients report a dramatic improvement in pain and function after recovery.
6. What are the potential risks or complications?
While elbow replacement is generally safe, possible risks include:
-
Infection at the surgical site
-
Implant loosening or wear over time
-
Nerve or blood vessel injury
-
Joint stiffness or instability
-
Allergic reaction to implant materials (rare)
Your orthopedic team takes every precaution to reduce these risks and ensure a smooth recovery.
7. What is the recovery period after Elbow Replacement Surgery?
Recovery varies from person to person, but generally:
-
Hospital stay: 1-3 days
-
Arm immobilization: in a sling or splint for about 2 weeks
-
Physical therapy: starts gradually after stitches are removed
-
Light activities: in 4-6 weeks
-
Full recovery: 3-6 months
Patients must follow their surgeon’s instructions carefully to achieve the best outcomes.
8. What restrictions should I follow after Elbow Replacement?
To protect the artificial joint, patients should:
-
Avoid lifting objects heavier than 2-3 kilograms
-
Refrain from high-impact activities (e.g., contact sports)
-
Use caution when pushing, pulling, or twisting movements
-
Maintain good joint hygiene and report any signs of infection immediately
Following these precautions can extend the life of the prosthesis.
9. How long does an Elbow Replacement last?
Modern elbow prostheses typically last 10 to 15 years or longer, depending on activity level and joint care. Advances in materials and surgical techniques have improved implant longevity and patient satisfaction over the years.
10. What results can I expect after Elbow Replacement Surgery?
Most patients experience excellent pain relief and restored elbow motion after recovery. While the new joint may not be as strong as a natural elbow, it allows for normal daily activities like eating, dressing, writing, and light lifting without pain.


