Introduction to Enucleation of the Prostate
Enucleation of the prostate is a highly advanced and minimally invasive surgical technique used to treat Benign Prostatic Hyperplasia (BPH) - a non-cancerous enlargement of the prostate gland that affects millions of men worldwide, particularly as they age. This procedure has transformed the landscape of urological surgery, offering a safer, more effective, and longer-lasting alternative to traditional methods like Transurethral Resection of the Prostate (TURP) and open prostatectomy.
The prostate gland is a walnut-sized organ located just below the bladder, surrounding the urethra - the tube that carries urine from the bladder to the outside of the body. As men get older, hormonal and cellular changes cause the prostate to grow larger. While this is a natural aging process, in many men the growth becomes excessive, squeezing the urethra and restricting urine flow. This leads to symptoms such as frequent urination, weak stream, incomplete bladder emptying, and nighttime urination (nocturia).
Enucleation of the prostate works by removing the overgrown prostate tissue (called adenoma) that compresses the urethra, while leaving the outer capsule intact. By completely “shelling out” the obstructive tissue, the surgery restores normal urine flow and relieves symptoms permanently.
This can be achieved through different modern techniques:
-
Holmium Laser Enucleation of the Prostate (HoLEP): Uses a Holmium laser for precise cutting and sealing.
-
Thulium Laser Enucleation (ThuLEP): Employs continuous-wave laser energy for smooth tissue removal.
-
Bipolar Enucleation (BipoLEP): Uses electric energy instead of a laser for cost-effective alternatives.
Enucleation has become the gold standard for prostates of all sizes - even very large glands (>100 grams) - due to its precision, low complication rate, and minimal recurrence. It is a one-time, definitive solution that combines the benefits of laser precision, endoscopic access, and rapid patient recovery.
By 2025, it is one of the most frequently performed advanced urological procedures, delivering excellent long-term results, minimal hospital stays, and superior safety compared to conventional surgeries.
Causes and Risk Factors Leading to Enucleation of the Prostate
The most common underlying cause leading to this surgery is Benign Prostatic Hyperplasia (BPH) - a condition that causes the prostate to enlarge and obstruct urinary flow. While the enlargement is non-cancerous, it can severely impact a man's quality of life if left untreated.
A. Main Causes of Prostate Enlargement
-
Hormonal Imbalance:
Testosterone is naturally converted into a more potent hormone called Dihydrotestosterone (DHT). As men age, DHT accumulates in the prostate, stimulating excessive cell growth and tissue thickening. -
Aging:
BPH is primarily age-related. Studies show that by the age of 60, nearly half of all men have some degree of prostate enlargement; by 80, this number exceeds 90%. -
Genetic Predisposition:
A family history of BPH significantly increases the risk of developing the condition earlier in life. -
Chronic Inflammation:
Recurrent prostatitis (inflammation of the prostate) triggers structural changes and tissue overgrowth. -
Metabolic Factors:
Conditions like obesity, diabetes, hypertension, and high cholesterol are closely linked to increased prostate size due to hormonal and vascular changes. -
Lifestyle Factors:
Sedentary behavior, excessive alcohol, smoking, and high-fat diets contribute to hormonal imbalance and poor pelvic circulation, worsening BPH symptoms.
B. Risk Factors for Severe BPH
-
Age over 50 years
-
Family history of prostate enlargement or prostate cancer
-
Obesity or metabolic syndrome
-
Lack of physical activity
-
Chronic stress (increases cortisol, which disrupts testosterone balance)
-
Long-term use of certain medications (e.g., antihistamines, decongestants)
-
Uncontrolled diabetes or hypertension
When these risk factors combine, prostate enlargement often progresses to a stage where medications are no longer effective, and surgical removal through enucleation becomes necessary to prevent bladder or kidney damage.
Symptoms and Signs of Prostate Enlargement
Prostate enlargement leads to Lower Urinary Tract Symptoms (LUTS), which can range from mild discomfort to severe obstruction. These symptoms develop gradually and worsen over time.
A. Common Urinary Symptoms
-
Increased Frequency of Urination:
Especially at night (nocturia), leading to disturbed sleep. -
Weak Urine Stream:
Reduced force and intermittent flow due to urethral narrowing. -
Difficulty Starting Urination:
Straining or hesitation before urine begins to flow. -
Incomplete Emptying:
Feeling that the bladder is never fully emptied. -
Urgency:
A sudden, intense urge to urinate. -
Dribbling or Leakage:
Especially after finishing urination.
B. Complications and Advanced Signs
-
Acute Urinary Retention: Complete inability to urinate.
-
Recurrent Urinary Tract Infections (UTIs): Due to stagnant urine.
-
Bladder Stones: From long-term urine retention.
-
Hematuria (Blood in Urine): Due to stretched bladder vessels.
-
Kidney Damage: Resulting from backflow pressure on the kidneys.
When symptoms severely interfere with daily life and conservative treatment fails, Enucleation of the Prostate becomes the preferred surgical option to permanently remove the obstructing tissue.
Diagnosis Before Enucleation of the Prostate
A thorough diagnostic work-up ensures that the enlargement is benign and that enucleation is the most appropriate treatment.
A. Diagnostic Methods
-
Medical History and Physical Examination:
Assessment of urinary symptoms using the International Prostate Symptom Score (IPSS) questionnaire. -
Digital Rectal Examination (DRE):
The doctor palpates the prostate through the rectum to estimate size and consistency. -
Prostate-Specific Antigen (PSA) Blood Test:
Elevated PSA can indicate BPH, infection, or cancer - further testing differentiates between them. -
Urinalysis:
Detects infections, blood, or abnormalities. -
Uroflowmetry:
Measures the rate and strength of urine flow. -
Post-Void Residual (PVR) Test:
Determines if urine remains in the bladder after voiding. -
Ultrasound or MRI:
Provides detailed imaging of prostate size, bladder wall thickness, and any upper urinary tract damage. -
Cystoscopy:
A small camera is inserted through the urethra to directly view the prostate and urinary tract. -
Biopsy (if required):
If PSA is high or irregularities are found, a biopsy rules out malignancy.
A precise diagnosis ensures that the chosen surgical approach - usually HoLEP or BipoLEP - is both safe and effective.
Treatment Options and the Enucleation Procedure
A. Medical Management (Initial Approach)
In early or mild BPH, doctors often prescribe:
-
Alpha-Blockers (e.g., tamsulosin, alfuzosin): Relax the bladder neck and prostate muscles.
-
5-Alpha Reductase Inhibitors (e.g., finasteride, dutasteride): Shrink the prostate by reducing DHT levels.
-
Phytotherapy: Plant-based supplements like saw palmetto (less evidence-based).
-
Lifestyle Adjustments: Fluid timing, diet changes, bladder training.
However, for large prostates or advanced symptoms, surgery becomes the best long-term option.
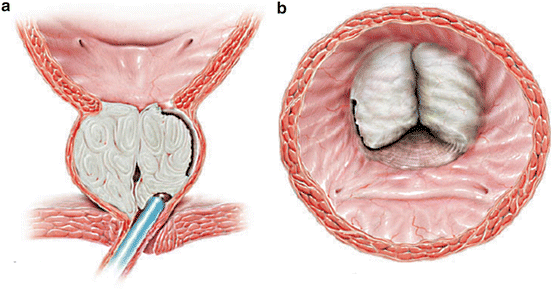
B. Enucleation of the Prostate - Step-by-Step Surgical Overview
-
Anesthesia:
The procedure is performed under spinal or general anesthesia. -
Insertion of Endoscope:
A thin instrument (resectoscope) is inserted through the urethra. -
Laser or Bipolar Dissection:
The surgeon uses laser energy or bipolar current to separate the inner adenoma from the prostate capsule, following natural tissue planes. -
Enucleation of Tissue:
The obstructive prostate tissue is gently pushed into the bladder. -
Morcellation:
The detached tissue is fragmented and removed using a morcellator - a device that grinds and extracts the tissue. -
Hemostasis (Control of Bleeding):
The laser simultaneously seals blood vessels, minimizing blood loss. -
Catheter Placement:
A urinary catheter is inserted for 1-2 days to ensure proper urine drainage and healing.
Duration and Recovery
-
Surgery time: 60-120 minutes
-
Hospital stay: Usually 1-2 days
-
Full recovery: 2-4 weeks
C. Benefits of Enucleation Over Traditional Surgery
-
Minimal bleeding and no open incisions
-
Short hospital stay and quick recovery
-
Effective for very large prostates
-
Lower recurrence rate compared to TURP
-
Preservation of erectile function
-
Improved urinary flow and long-term satisfaction
Enucleation has now largely replaced older surgical methods, becoming the gold standard for BPH management.
Prevention and Management of Prostate Health
A. Preventive Measures
While prostate enlargement can't be fully prevented, adopting a healthy lifestyle significantly reduces risk:
-
Maintain a healthy weight and regular exercise routine.
-
Consume a balanced diet - rich in vegetables, fruits, and omega-3 fatty acids.
-
Reduce caffeine and alcohol intake.
-
Avoid smoking to improve circulation.
-
Stay hydrated, but reduce fluid intake before bedtime.
-
Regular prostate checkups after the age of 40.
B. Post-Surgical Management and Recovery
-
Immediate Care:
The catheter is removed within 1-2 days after surgery. Mild burning during urination is normal initially. -
Hydration:
Drinking plenty of water helps flush the urinary tract and prevent infection. -
Activity Restrictions:
Avoid heavy lifting, cycling, and sexual activity for 4-6 weeks. -
Dietary Advice:
Light, high-fiber meals prevent constipation and strain. -
Medication:
Antibiotics and anti-inflammatory drugs aid recovery. -
Follow-Up:
Regular visits at 2 weeks, 1 month, and 3 months post-surgery to monitor healing and urine flow.
Patients typically notice dramatic improvement in urinary symptoms within days and return to normal life quickly.
Complications of Enucleation of the Prostate
While rare, like any surgery, enucleation has potential side effects - though these are far fewer and milder compared to older procedures.
A. Common Temporary Effects
-
Mild bleeding or pink urine for a few days.
-
Frequent urination or urgency during healing.
-
Burning sensation while urinating.
-
Retrograde ejaculation: Semen flows backward into the bladder during orgasm (harmless).
B. Rare Complications
-
Urinary Tract Infection (UTI) - treated with antibiotics.
-
Urethral stricture - narrowing due to scar tissue (rare).
-
Bladder injury or temporary incontinence (very rare).
-
Reoperation (less than 1%) for residual tissue or regrowth.
With advanced laser precision and skilled surgeons, complication rates are under 2-3%, and most are temporary.
Living After Enucleation of the Prostate
A. Recovery and Long-Term Well-Being
After enucleation, most patients experience immediate relief
from symptoms such as urgency, weak stream, and nocturia.
They regain normal bladder control and significantly improve quality of life.
Long-term care involves:
-
Maintaining hydration.
-
Continuing pelvic floor (Kegel) exercises to strengthen bladder control.
-
Resuming sexual activity after medical clearance (usually 4-6 weeks).
-
Attending annual prostate checkups.
B. Emotional and Psychological Recovery
Many men report feeling younger, more energetic, and confident after surgery. The constant anxiety over urinary issues and interrupted sleep is replaced by comfort and peace of mind.
C. Long-Term Outcomes
Clinical studies show that enucleation provides lasting relief for over 10-15 years with success rates above 95%. Most patients never need repeat surgery. It has proven superior to TURP and open prostatectomy in durability and safety.
Top 10 Frequently Asked Questions about Enucleation of Prostate
1. What is Enucleation of the Prostate?
Enucleation of the prostate is a minimally invasive surgical
procedure used to treat Benign Prostatic Hyperplasia (BPH)
- a non-cancerous enlargement of the prostate gland that can block urine flow. The
procedure involves removing the entire obstructive portion of the prostate
tissue that is pressing on the urethra, thereby restoring normal urine
flow.
Common techniques include Holmium Laser Enucleation of the Prostate
(HoLEP) and Bipolar Enucleation of the Prostate (BEP).
2. Why is Enucleation of the Prostate performed?
This surgery is recommended for men who experience moderate to severe urinary symptoms due to BPH, such as:
-
Weak or slow urine stream
-
Frequent urination, especially at night (nocturia)
-
Difficulty starting urination
-
Incomplete bladder emptying
-
Urinary retention or infections
When medications fail to relieve symptoms, enucleation offers long-term, effective relief.
3. How is Enucleation of the Prostate different from TURP (Transurethral Resection of the Prostate)?
While both surgeries treat prostate enlargement:
-
TURP removes only small portions of prostate tissue layer by layer.
-
Enucleation removes the entire obstructive adenoma (core tissue), similar to open prostate surgery but without large incisions.
This makes enucleation more complete and long-lasting, with a lower risk of needing reoperation compared to TURP.
4. How is the procedure performed?
The surgery is performed under spinal or general anesthesia using an
endoscope inserted through the urethra (no external cuts).
Steps include:
-
Using a laser or bipolar energy to separate the enlarged prostate tissue from the capsule.
-
Removing the tissue in one piece and cutting it into smaller fragments.
-
Suctioning the fragments out using a special instrument called a morcellator.
The entire procedure usually takes 60-120 minutes, depending on prostate size.
5. What are the benefits of Prostate Enucleation?
Key advantages include:
-
Minimally invasive - no external incision
-
Complete removal of enlarged tissue for long-term results
-
Shorter hospital stay (1-2 days)
-
Less bleeding and safer for patients on blood thinners
-
Faster recovery compared to open surgery
-
Low reoperation rate
It provides excellent relief from urinary symptoms and improves overall quality of life.
6. What are the possible risks or side effects?
While generally safe, potential risks include:
-
Temporary urinary incontinence (usually improves in a few weeks)
-
Mild burning or discomfort during urination
-
Blood in urine for a few days
-
Retrograde ejaculation (semen flows backward into the bladder)
-
Urinary tract infection (UTI)
Serious complications are rare when performed by experienced urologists.
7. How long does it take to recover after Enucleation of the Prostate?
Recovery is typically fast:
-
Hospital stay: 24-48 hours
-
Catheter removal: within 1-2 days
-
Return to light work: in 5-7 days
-
Full recovery: within 3-4 weeks
Patients are advised to avoid heavy lifting, strenuous exercise, and sexual activity for at least 4-6 weeks post-surgery.
8. Will Enucleation of the Prostate affect sexual function?
In most cases, sexual function (erection ability) is preserved after surgery. However, retrograde ejaculation (semen flowing backward into the bladder instead of out through the penis) is a common side effect. This is harmless but may affect fertility. It does not impact sexual pleasure or orgasm.
9. How successful is Prostate Enucleation?
The procedure has a success rate of over 90% for relieving urinary symptoms and improving flow. Studies show that patients experience significant improvement in quality of life, minimal recurrence, and lower reoperation rates compared to other surgical methods like TURP.
10. Who is an ideal candidate for Enucleation of the Prostate?
You may be a good candidate if you:
-
Have moderate to severe urinary symptoms from BPH
-
Have a large prostate gland (usually over 60-80 grams)
-
Do not respond well to medications
-
Want a long-term solution with minimal invasiveness
-
Are at higher bleeding risk (since laser enucleation minimizes bleeding)
A urologist will evaluate your prostate size, health condition, and preferences before recommending the procedure.


