Introduction to Fontan's Operation
Fontan's Operation is a complex and lifesaving cardiac surgical procedure designed for children born with single-ventricle congenital heart defects, in which only one ventricle is capable of effectively pumping blood to the body. This group of defects includes conditions such as tricuspid atresia, hypoplastic left heart syndrome, double-inlet left ventricle, and pulmonary atresia.
The Fontan procedure is typically the final stage in a series of staged heart surgeries that help reroute blood flow in a way that allows oxygen-poor (blue) blood to reach the lungs without passing through a defective or missing ventricle. It essentially creates a new circulatory pathway that directs venous (deoxygenated) blood from the body directly to the pulmonary arteries - bypassing the heart chambers.
The main goal of the Fontan operation is to improve oxygenation, reduce cyanosis (bluish discoloration of the skin), and enable the patient to live a more active, symptom-free life. Since its introduction by Dr. Francis Fontan and Dr. Eugene Baudet in 1971, the procedure has undergone many refinements, including extracardiac conduit techniques and lateral tunnel modifications, which have improved survival, reduced complications, and enhanced long-term outcomes.
Fontan's Operation is typically performed between 2 to 5 years of age, depending on the child's condition and previous surgical stages (such as the Norwood and Glenn procedures). With current surgical advancements and long-term postoperative care, many patients now live well into adulthood with good quality of life, turning what was once a fatal diagnosis into a manageable, chronic condition.
Causes and Risk Factors Leading to Fontan's Operation
The Fontan operation is performed for children and adults who have congenital heart defects that result in a functionally single ventricle-meaning only one pumping chamber is able to support the circulation for both the lungs and the body. The Fontan procedure provides a pathway to improve oxygen delivery and reduce the workload on the single functioning ventricle.
A. Causes: Underlying Heart Conditions
Fontan's Operation is not performed because of a disease that develops over time - it's a corrective procedure for congenital heart defects present at birth. These defects prevent normal two-ventricle blood flow and oxygenation. Common congenital anomalies requiring Fontan circulation include:
-
Tricuspid Atresia - The tricuspid valve (between the right atrium and right ventricle) is absent, preventing normal blood flow to the lungs.
-
Hypoplastic Left Heart Syndrome (HLHS) - The left ventricle is underdeveloped, unable to pump blood to the body.
-
Double-Inlet Left Ventricle - Both atria connect to the same ventricle, disrupting oxygenated and deoxygenated blood separation.
-
Pulmonary Atresia - The pulmonary valve is malformed or blocked, preventing blood flow from the right ventricle to the lungs.
-
Single-Ventricle Physiology - Any condition where one ventricle cannot pump effectively.
In such cases, the Fontan procedure creates a new route for deoxygenated blood to flow directly to the lungs, enabling oxygen exchange without depending on the heart's pumping action.
B. Risk Factors for Needing and Undergoing Fontan Surgery
Certain factors may increase the risk for congenital heart disease requiring Fontan repair:
-
Genetic factors: Chromosomal abnormalities like Turner or Down syndrome.
-
Maternal illnesses: Diabetes, viral infections during pregnancy, or medication use.
-
Family history: Higher recurrence in families with congenital defects.
-
Environmental exposures: Radiation, alcohol, or certain chemicals during pregnancy.
C. Surgical Risk Factors
While Fontan surgery has become safer, several risk factors affect surgical outcomes:
-
Very small or abnormal pulmonary arteries.
-
Elevated pulmonary vascular resistance.
-
Weak or failing single ventricle function.
-
Atrioventricular valve regurgitation.
-
Abnormal heart rhythm (arrhythmia).
-
Liver congestion or fibrosis before surgery.
Children are thoroughly evaluated to ensure their heart and lungs can handle the Fontan circulation before proceeding.
Symptoms and Signs Indicating the Need for Fontan's Operation
The need for Fontan's Operation arises when a child has single-ventricle physiology and shows signs that their circulation cannot deliver enough oxygen to the body. Symptoms usually appear early in life, often within the first few months.
Common Symptoms Include:
-
Cyanosis (Bluish Skin):
The most recognizable symptom - due to inadequate oxygen in the blood. -
Fatigue and Exercise Intolerance:
The heart struggles to supply oxygen-rich blood, causing easy tiredness during feeding or play. -
Breathing Difficulties:
Shortness of breath and rapid breathing due to inefficient oxygen exchange. -
Poor Growth and Weight Gain:
Known as “failure to thrive,” caused by high energy demand and poor circulation. -
Swelling (Edema):
Accumulation of fluid in legs, abdomen, or around the eyes from poor venous return. -
Heart Murmurs:
Irregular blood flow through malformed structures produces audible murmurs during examination. -
Bluish Lips and Fingertips:
Persistent cyanosis even after earlier palliative surgeries (like Glenn procedure) signals the need for Fontan completion.
When these signs persist despite prior interventions, Fontan's Operation is planned to improve oxygenation and long-term survival.
Diagnosis and Preoperative Evaluation for Fontan's Operation
Before surgery, an extensive diagnostic evaluation is done to ensure that the patient is a suitable candidate. The Fontan procedure requires good ventricular function, low pulmonary pressures, and well-developed pulmonary arteries.
A. Diagnostic Tests Include:
-
Echocardiography (Echo):
Provides detailed visualization of the heart's anatomy, ventricular function, and blood flow patterns. -
Cardiac Catheterization:
Measures pressures in the heart and lungs, ensuring pulmonary resistance is low enough for Fontan physiology. -
Magnetic Resonance Imaging (MRI) / CT Angiography:
Offers 3D mapping of cardiac and vascular anatomy for surgical planning. -
Electrocardiogram (ECG):
Detects arrhythmias or conduction abnormalities. -
Oxygen Saturation Tests:
Monitors oxygen levels before surgery to evaluate need and urgency. -
Blood and Liver Function Tests:
Essential to assess how well the liver is handling blood flow congestion (common in pre-Fontan patients). -
Exercise Testing (Older Children):
Measures exercise tolerance and cardiac response to stress.
B. Pre-Surgical Assessment Criteria
A child is considered ready for Fontan completion if:
-
Pulmonary arteries are of good size.
-
Ventricular function is strong.
-
No major valve leaks are present.
-
Pulmonary resistance is low (< 2 Wood units).
-
Oxygen saturation is typically 75-85% after prior Glenn procedure.
Once these criteria are met, the surgical team proceeds with Fontan repair to establish a permanent, stable circulation.
Treatment Options: The Fontan Surgical Procedure
The Fontan surgical procedure is the third stage in the single-ventricle palliation pathway for children with complex congenital heart disease, especially those with only one functional ventricle. The procedure directs all venous (deoxygenated) blood from the body straight to the lungs, bypassing the heart, and allows the single ventricle to pump only oxygen-rich blood to the body.
A. Surgical Overview
Fontan's Operation is usually the final stage in a three-part surgical sequence:
-
Stage 1: Initial palliation (e.g., Norwood procedure).
-
Stage 2: Glenn or Hemi-Fontan procedure - connects the superior vena cava (SVC) to the pulmonary arteries.
-
Stage 3: The Fontan completion, connecting the inferior vena cava (IVC) to the pulmonary arteries, directing all systemic venous blood to the lungs.
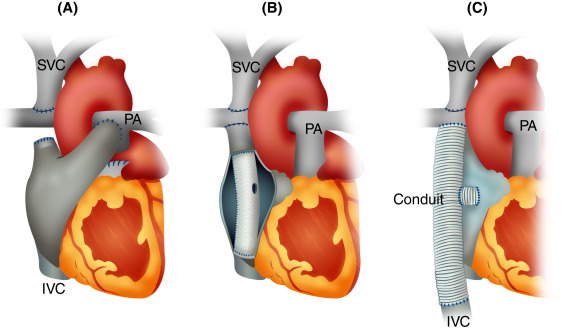
B. Types of Fontan Procedure
-
Lateral Tunnel Fontan:
Uses a baffle inside the right atrium to direct blood from the IVC to the pulmonary arteries. -
Extracardiac Conduit Fontan (Modern Standard):
A synthetic tube connects the IVC directly to the pulmonary artery outside the heart, reducing atrial pressure and arrhythmias.
C. Key Steps in Surgery
-
Performed under general anesthesia with cardiopulmonary bypass.
-
Deoxygenated blood from the IVC is rerouted through a conduit to the pulmonary arteries.
-
The heart continues pumping oxygenated blood to the body.
-
A small fenestration (hole) is sometimes made between the conduit and atrium to allow pressure relief and gradual adaptation.
D. Postoperative Care
-
Intensive monitoring in the cardiac ICU.
-
Oxygen therapy and medications to manage fluid balance and prevent clotting.
-
Gradual return to normal activity as the child stabilizes.
The Fontan circulation significantly improves oxygenation (usually 90-95%), reduces cyanosis, and allows near-normal physical development.
Prevention and Management of Fontan's Operation
Prevention and management after the Fontan operation center around minimizing both immediate surgical risks and long-term complications inherent to this unique circulatory system. The approach requires careful perioperative support, long-term multidisciplinary care, targeted monitoring, and specific treatments for common complications associated with Fontan circulation.
A. Preventing Complications
-
Early Diagnosis: Prenatal and neonatal screening for congenital heart defects.
-
Staged Surgical Timing: Proper timing between Norwood, Glenn, and Fontan stages.
-
Lifestyle and Nutrition: Balanced diet, infection prevention, and growth monitoring.
-
Avoiding Dehydration: Important to maintain adequate Fontan flow.
-
Exercise Moderation: Light physical activity encouraged; avoid overexertion.
B. Post-Fontan Management
-
Lifelong follow-up with a congenital cardiologist.
-
Regular echocardiograms and liver ultrasounds to detect early complications.
-
Blood thinners (anticoagulants) may be prescribed to prevent clot formation.
-
Vaccinations against respiratory and liver infections (hepatitis, flu) are essential.
Continuous monitoring of heart rhythm, liver function, and oxygen levels is vital for maintaining long-term Fontan success.
Complications of Fontan's Operation
Although most children recover well, Fontan circulation is not a “normal” physiology and can lead to long-term complications.
Short-Term Complications:
-
Fluid Retention (Effusions): Fluid buildup in lungs or abdomen post-surgery.
-
Arrhythmias: Irregular heartbeats from altered electrical pathways.
-
Low Cardiac Output: Due to early adaptation of the new circulation.
-
Bleeding or Clot Formation: Managed with anticoagulants.
Long-Term Complications:
-
Fontan-Associated Liver Disease (FALD):
Chronic congestion in the liver may cause fibrosis over years. -
Protein-Losing Enteropathy (PLE):
Loss of proteins through intestines leading to swelling and malnutrition. -
Plastic Bronchitis:
Rare complication where mucus plugs form in the airways. -
Arrhythmias and Heart Failure:
May develop decades later; often managed medically or with catheter-based interventions. -
Exercise Intolerance:
Limited capacity due to lack of a pumping right ventricle.
Thanks to modern surgical refinement and follow-up care, most patients live full, active lives into adulthood, though lifelong medical monitoring is essential.
Living with the Condition of Fontan Circulation
Living with Fontan circulation requires understanding, adaptation, and proactive healthcare.
A. Childhood and Adolescence
-
Children can attend school, participate in mild sports, and lead a near-normal life.
-
Regular checkups are needed to monitor growth, oxygen levels, and heart performance.
B. Adulthood
-
Adults with Fontan circulation (so-called “Fontan survivors”) require lifelong specialized cardiac care.
-
Pregnancy is possible but must be carefully managed by maternal-fetal and cardiac specialists.
-
Patients must avoid dehydration, extreme exertion, and high-altitude travel.
C. Emotional and Psychosocial Health
Many families face anxiety during treatment stages. Emotional support, counseling, and support groups play a vital role in coping and promoting mental well-being.
D. Long-Term Outlook
With proper care, 70-80% of Fontan patients survive beyond 20-30 years, and new therapies aim to further extend quality of life. Advances such as ventricular assist devices (VADs) and heart-liver transplantation are now available for late complications, ensuring continued hope and longevity.
Top 10 Frequently Asked Questions about Fontan's Operation
1. What is Fontan's Operation?
Fontan's Operation is a complex congenital heart
surgery performed to treat children born with single ventricle
heart defects - conditions in which only one ventricle is strong enough to
pump blood effectively.
The procedure directs deoxygenated (blue) blood from the body directly
to the pulmonary arteries (lungs) without passing through the heart.
This allows the single functioning ventricle to pump
oxygen-rich blood to the rest of the body efficiently.
2. Why is the Fontan procedure performed?
Fontan's operation is performed in children who have congenital heart conditions that prevent normal two-ventricle circulation, such as:
-
Tricuspid atresia
-
Hypoplastic left heart syndrome (HLHS)
-
Double inlet left ventricle
-
Pulmonary atresia with intact septum
It helps improve oxygen levels, reduce cyanosis (bluish skin), and enhance quality of life and longevity in children with single ventricle physiology.
3. At what age is Fontan's Operation usually performed?
The Fontan procedure is typically the third and final stage in a series of surgeries for single-ventricle heart defects:
-
Stage 1 (Norwood procedure): Done in the newborn period.
-
Stage 2 (Glenn or Hemi-Fontan procedure): Around 4-6 months of age.
-
Stage 3 (Fontan procedure): Performed between 18 months and 4 years of age, depending on the child's condition and oxygen levels.
Your pediatric cardiologist will determine the ideal timing based on heart function and overall growth.
4. How is Fontan's Operation performed?
During Fontan's Operation:
-
The surgeon connects the inferior vena cava (IVC) - the large vein that brings blood from the lower body - directly to the pulmonary arteries.
-
This allows deoxygenated blood to flow passively to the lungs, bypassing the heart.
-
A conduit (tube or channel) is often used to make this connection.
-
Sometimes, a small fenestration (hole) is created between the conduit and the atrium to reduce pressure and improve recovery.
The procedure is done under general anesthesia and typically takes 4-6 hours.
5. What are the expected benefits of the Fontan procedure?
The main benefits include:
-
Improved oxygenation of blood
-
Reduced cyanosis (blue discoloration)
-
Better exercise tolerance and energy levels
-
Improved growth and development in children
-
Long-term survival into adulthood for single-ventricle patients
It helps stabilize the child's condition and allows for near-normal daily activities.
6. What are the possible risks or complications of Fontan's Operation?
Although Fontan's surgery is life-saving, potential risks include:
-
Bleeding or infection after surgery
-
Heart rhythm disturbances (arrhythmias)
-
Fluid buildup (pleural effusion) around lungs
-
Blood clots in the Fontan circuit
-
Protein-losing enteropathy (PLE) - a rare intestinal complication
-
Liver congestion or long-term liver problems
With modern surgical techniques and specialized care, the risk of major complications has significantly decreased.
7. How long is the recovery period after Fontan's Operation?
Recovery involves:
-
Hospital stay: 2-3 weeks (ICU for the first few days)
-
Monitoring for fluid balance, oxygen levels, and heart rhythm
-
Gradual improvement in energy, breathing, and activity levels
Most children can return to normal daily routines within 2-3 months, but regular follow-up with a pediatric cardiologist is essential.
8. What is life like after Fontan's Operation?
Most children live active, fulfilling lives after the Fontan procedure.
They can attend school, play, and engage in light physical activities.
However:
-
Intense or competitive sports may be restricted.
-
Regular cardiac follow-ups, echocardiograms, and exercise testing are crucial.
-
Some patients may require medications such as blood thinners or diuretics long-term.
With good medical care, many Fontan patients live into adulthood and maintain a good quality of life.
9. Are there any long-term complications of Fontan circulation?
Yes, Fontan circulation can lead to certain long-term issues, including:
-
Liver congestion or fibrosis (Fontan-associated liver disease)
-
Protein-losing enteropathy (PLE)
-
Arrhythmias or heart failure over time
-
Exercise intolerance due to reduced cardiac output
Lifelong follow-up in a congenital heart disease (CHD) specialty clinic is recommended for early detection and management.
10. What is the long-term outlook after Fontan's Operation?
The long-term survival rate after Fontan's surgery is over
80-90% at 10-20 years post-surgery. Advances in surgical techniques and
postoperative care have greatly improved outcomes.
Many patients grow into adulthood, complete education, work, and even have families.
With regular monitoring, a heart-healthy lifestyle, and preventive
care, Fontan patients can lead long, meaningful lives.


